Hellenic Journal of Cardiology ( IF 4.1 ) Pub Date : 2023-11-11 , DOI: 10.1016/j.hjc.2023.11.003 Hugo Costa 1 , Miguel Espírito-Santo 1 , Raquel Fernandes 1 , João Bispo 1 , João Guedes 1 , Pedro Azevedo 1 , Daniela Carvalho 1 , Hugo Vinhas 1 , Rui Baptista Gonçalves 2 , Jorge Mimoso 1 , 3
|
Background
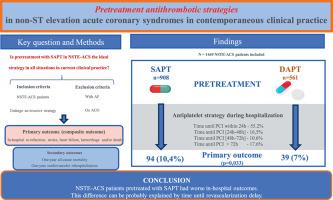
Pretreatment antithrombotic strategies in non-ST elevation acute coronary syndromes (NSTE-ACS) during hospitalization is still a matter of contention within the cardiology community. Our aim was to analyze in-hospital and one-year follow-up outcomes of patients with NSTE-ACS pretreated with dual antiplatelet therapy (DAPT) versus single antiplatelet therapy (SAPT).
Methods
A retrospective study was carried out with NSTE-ACS patients planned to undergo an invasive strategy and were included in the Portuguese Registry of ACS between 2018-2021. A composite primary outcome (in-hospital re-infarction, stroke, heart failure, hemorrhage, death) was compared regarding antiplatelet strategy (DAPT versus SAPT). Secondary outcomes were defined as one-year all-cause mortality and one-year cardiovascular rehospitalization.
Results
A total of 1469 patients were included, with a mean age of 66±12 years and 73.9% were male. DAPT regime was used in 38.2% and SAPT in 61.8% of patients. NSTE myocardial infarction was the most frequent presentation (88.5%). Revascularization after 24h occurred in 44.8% patients (63% of these after 48h). Enoxaparin was the anticoagulant more frequently used (45.1%). The primary outcome was more frequently observed in the SAPT group (10.4%, p=0.033), mainly driven by more ischemic events. Time until revascularization > 48h and SAPT regime were independent predictors of the primary outcome (OR 1.66, p=0.036 and OR 2.03, p=0.008, respectively).
Conclusion
NSTE-ACS patients pretreated with SAPT had worse in-hospital outcomes. This difference can be probably explained by a delay in time until revascularization. Pretreatment DAPT strategy and crossover between heparins is still frequently used in clinical practice.
中文翻译:

同期临床实践中非 ST 段抬高型急性冠脉综合征的预处理抗血栓策略
背景
非 ST 段抬高型急性冠状动脉综合征 (NSTE-ACS) 住院期间的预处理抗血栓策略仍然是心脏病学界争论的问题。我们的目的是分析接受双重抗血小板治疗 (DAPT) 与单一抗血小板治疗 (SAPT) 预处理的 NSTE-ACS 患者的院内和一年随访结果。
方法
对计划接受侵入性策略并在 2018 年至 2021 年间纳入葡萄牙 ACS 登记的 NSTE-ACS 患者进行了一项回顾性研究。比较抗血小板策略(DAPT 与 SAPT)的复合主要结局(院内再梗死、中风、心力衰竭、出血、死亡)。次要结局被定义为一年全因死亡率和一年心血管再住院率。
结果
共纳入 1469 名患者,平均年龄 66±12 岁,73.9%为男性。38.2% 的患者使用了 DAPT 方案,61.8% 的患者使用了 SAPT。NSTE 心肌梗死是最常见的表现(88.5%)。44.8% 的患者在 24 小时后进行血运重建(其中 63% 在 48 小时后)。依诺肝素是最常用的抗凝剂(45.1%)。主要结局在 SAPT 组中更为常见(10.4%,p=0.033),主要是由于更多的缺血事件所致。血运重建时间 > 48 小时和 SAPT 方案是主要结局的独立预测因子(分别为 OR 1.66,p=0.036 和 OR 2.03,p=0.008)。
结论
接受 SAPT 预处理的 NSTE-ACS 患者院内结局较差。这种差异可能可以用血运重建之前的时间延迟来解释。预处理 DAPT 策略和肝素之间的交叉在临床实践中仍然经常使用。



























 京公网安备 11010802027423号
京公网安备 11010802027423号