Trends in Cardiovascular Medicine ( IF 9.3 ) Pub Date : 2023-12-23 , DOI: 10.1016/j.tcm.2023.12.005 Michel Pompeu Sá , Xander Jacquemyn , James A. Brown , Danial Ahmad , Derek Serna-Gallegos , George J. Arnaoutakis , Michael J. Singh , Ibrahim Sultan
|
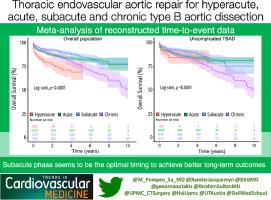
Since the optimal timing for thoracic endovascular aortic repair (TEVAR) in the context of type B aortic dissections (TBAD) remains an open question, we performed a systematic review with meta-analysis to evaluate outcomes of TEVAR according to the phases of TBAD – hyperacute, acute, subacute and chronic. We carried out a pooled meta-analysis of time-to-event data extracted from studies published by June 2023 for the following outcomes: all-cause mortality, aortic-related mortality, and late aortic reinterventions. Thirteen studies met our eligibility criteria, comprising 4,793 patients (10.3% hyperacute, 51.9% acute, 25.9% subacute, 11.9% chronic). Considering the overall population, we observed a statistically significant difference between the groups (Log-rank test, P<0.0001) and the main differences were found in the following comparisons: hyperacute versus acute (HR 1.61; 95%CI 1.21-2.13; P=0.001); hyperacute versus chronic (HR 1.70; 95%CI 1.17-2.46; P=0.005); subacute versus acute (HR 0.78; 95%CI 0.63-0.98; P=0.032). Considering the population with uncomplicated TBAD, we also observed a statistically significant difference for all-cause death between the groups (Log-rank test, P<0.0001) and the main differences were found in the comparisons for subacute versus acute (HR 0.72; 95%CI 0.58-0.88; P=0.002). Furthermore, we observed statistically significant differences between the groups for aortic-related death (Log-rank test, P<0.0001) and late aortic reintervention (Log-rank test, P<0.0001), all favoring mostly the subacute phase as the optimal timing for TEVAR. In conclusion, there seems to be a timing-specific difference in the outcomes of TEVAR for TBAD pointing to the subacute phase as the optimal timing to achieve better long-term outcomes.
中文翻译:

胸主动脉腔内修复术治疗超急性、急性、亚急性和慢性 B 型主动脉夹层:重建事件时间数据的荟萃分析
由于 B 型主动脉夹层 (TBAD) 背景下胸主动脉腔内修复术 (TEVAR) 的最佳时机仍然是一个悬而未决的问题,我们进行了系统回顾和荟萃分析,根据 TBAD 的阶段评估 TEVAR 的结果 - 超急性期,急性,亚急性和慢性。我们对从 2023 年 6 月发表的研究中提取的事件发生时间数据进行了汇总荟萃分析,结果如下:全因死亡率、主动脉相关死亡率和晚期主动脉再干预。13 项研究符合我们的资格标准,包括 4,793 名患者(10.3% 超急性、51.9% 急性、25.9% 亚急性、11.9% 慢性)。考虑到总体人群,我们观察到各组之间存在统计学显着差异(对数秩检验,P<0.0001),主要差异在以下比较中发现:超急性与急性(HR 1.61;95%CI 1.21-2.13;P =0.001); 超急性与慢性(HR 1.70;95%CI 1.17-2.46;P=0.005);亚急性与急性(HR 0.78;95%CI 0.63-0.98;P=0.032)。考虑到无并发症的 TBAD 人群,我们还观察到各组之间全因死亡存在统计学显着差异(对数秩检验,P<0.0001),主要差异发现于亚急性与急性的比较中(HR 0.72;95) %CI 0.58-0.88;P=0.002)。此外,我们观察到主动脉相关死亡(对数秩检验,P<0.0001)和晚期主动脉再干预(对数秩检验,P<0.0001)各组之间存在统计学显着差异,所有这些都倾向于将亚急性期作为最佳时机对于 TEVAR。总之,TEVAR 治疗 TBAD 的结果似乎存在时间特异性差异,表明亚急性期是实现更好长期结果的最佳时机。



























 京公网安备 11010802027423号
京公网安备 11010802027423号