Strahlentherapie und Onkologie ( IF 3.1 ) Pub Date : 2024-01-24 , DOI: 10.1007/s00066-024-02199-6 Xiaoyan Lv , Yajing Wu , Qihui Li , Chen Zheng , Qiang Lin , Qingsong Pang , Min Zhao , Jiandong Zhang , Jun Wang
|
Purpose
This study aims to evaluate the risk factors of treatment-related pneumonitis (TRP) following thoracic radiotherapy/chemoradiotherapy combined with anti-PD‑1 monoclonal antibodies (mAbs) in patients with advanced esophageal squamous cell carcinoma (ESCC).
Methods
We retrospectively reviewed 97 patients with advanced ESCC who were treated with thoracic radiotherapy/chemoradiotherapy combined with anti-PD‑1 mAbs. Among them, 56 patients received concurrent radiotherapy with anti-PD‑1 mAbs and 41 patients received sequential radiotherapy with anti-PD‑1 mAbs. The median prescribed planning target volume (PTV) dose was 59.4 Gy (range from 50.4 to 66 Gy, 1.8–2.2 Gy/fraction). Clinical characteristics, the percentage of lung volume receiving more than 5–50 Gy in increments of 5 Gy (V5–V50, respectively) and the mean lung dose (MLD) were analyzed as potential risk factors for TRP.
Results
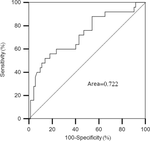
46.4% (45/97), 20.6% (20/97), 20.6% (20/97), 4.1% (4/97), and 1.0% (1/97) of the patients developed any grade of TRP, grade 1 TRP, grade 2 TRP, grade 3 TRP, and fatal (grade 5) TRP, respectively. Anti-PD‑1 mAbs administered concurrently with radiotherapy, V5, V10, V15, V25, V30, V35, V40 and MLD were associated with the occurrence of grade 2 or higher TRP. Concurrent therapy (P = 0.010, OR = 3.990) and V5 (P = 0.001, OR = 1.126) were independent risk factors for grade 2 or higher TRP. According to the receiver operating characteristic (ROC) curve analysis, the optimal V5 threshold for predicting grade 2 or higher TRP was 55.7%.
Conclusion
The combination of thoracic radiotherapy/chemoradiotherapy with anti-PD‑1 mAbs displayed a tolerable pulmonary safety profile. Although the incidence of TRP was high, grade 1–2 TRP accounted for the majority. Anti-PD‑1 mAbs administered concurrently with radiotherapy and the lung V5 were significantly associated with the occurrence of grade 2 or higher TRP. Therefore, it seems safer to control V5 below 55% in clinical, especially for the high-risk populations receiving concurrent therapy.
中文翻译:

晚期食管鳞癌胸部放疗/放化疗联合抗PD-1单克隆抗体后治疗相关性肺炎
目的
本研究旨在评估晚期食管鳞状细胞癌(ESCC)患者胸部放疗/放化疗联合抗PD-1单克隆抗体(mAb)后发生治疗相关性肺炎(TRP)的危险因素。
方法
我们回顾性分析了 97 例接受胸部放疗/放化疗联合抗 PD-1 mAb 治疗的晚期 ESCC 患者。其中,56名患者接受抗PD-1单克隆抗体同步放疗,41名患者接受抗PD-1单克隆抗体序贯放疗。中位规定计划靶体积 (PTV) 剂量为 59.4 Gy(范围为 50.4 至 66 Gy,1.8–2.2 Gy/分次)。临床特征、接受超过 5-50 Gy 以 5 Gy 增量(分别为 V 5 –V 50 )的肺体积百分比和平均肺剂量 (MLD) 被分析为 TRP 的潜在危险因素。
结果
46.4% (45/97)、20.6% (20/97)、20.6% (20/97)、4.1% (4/97) 和 1.0% (1/97) 的患者出现任何级别的 TRP、分别为 1 级 TRP、2 级 TRP、3 级 TRP 和致命(5 级)TRP。抗 PD-1 mAb 与放射治疗同时使用,V 5、V 10、V 15、V 25、V 30、V 35、V 40和 MLD 与 2 级或更高级别 TRP 的发生相关。同步治疗 ( P = 0.010, OR = 3.990) 和 V 5 ( P = 0.001, OR = 1.126) 是 2 级或以上 TRP 的独立危险因素。根据受试者工作特征(ROC)曲线分析,预测2级或更高TRP的最佳V 5阈值为55.7%。
结论
胸部放疗/放化疗与抗 PD-1 mAb 的组合显示出可耐受的肺部安全性。尽管TRP的发生率较高,但1~2级TRP占大多数。与放疗和肺 V 5同时施用的抗 PD-1 mAb 与2 级或更高级别 TRP 的发生显着相关。因此,临床上将V 5控制在55%以下似乎更安全,特别是对于接受同步治疗的高危人群。



























 京公网安备 11010802027423号
京公网安备 11010802027423号