当前位置:
X-MOL 学术
›
J. Thorac. Cardiovasc. Surg.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Identifying and mitigating risk of postcardiotomy cardiogenic shock in patients with ischemic and nonischemic cardiomyopathy
The Journal of Thoracic and Cardiovascular Surgery ( IF 6 ) Pub Date : 2024-03-05 , DOI: 10.1016/j.jtcvs.2024.02.025 Michael J. Javorski , Karolis Bauza , Fei Xiang , Edward Soltesz , Lin Chen , Faisal G. Bakaeen , Lars Svensson , Lucy Thuita , Eugene H. Blackstone , Michael Z. Tong
The Journal of Thoracic and Cardiovascular Surgery ( IF 6 ) Pub Date : 2024-03-05 , DOI: 10.1016/j.jtcvs.2024.02.025 Michael J. Javorski , Karolis Bauza , Fei Xiang , Edward Soltesz , Lin Chen , Faisal G. Bakaeen , Lars Svensson , Lucy Thuita , Eugene H. Blackstone , Michael Z. Tong
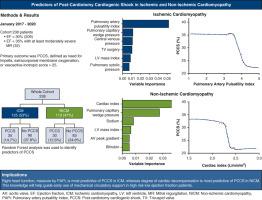
|
To identify preoperative predictors of postcardiotomy cardiogenic shock in patients with ischemic and nonischemic cardiomyopathy and evaluate trajectory of postoperative ventricular function. From January 2017 to January 2020, 238 patients with ejection fraction <30% (206/238) or 30% to 34% with at least moderately severe mitral regurgitation (32/238) underwent conventional cardiac surgery at Cleveland Clinic, 125 with ischemic and 113 with nonischemic cardiomyopathy. Preoperative ejection fraction was 25 ± 4.5%. The primary outcome was postcardiotomy cardiogenic shock, defined as need for microaxial temporary left ventricular assist device, extracorporeal membrane oxygenation, or vasoactive-inotropic score >25. RandomForestSRC was used to identify its predictors. Postcardiotomy cardiogenic shock occurred in 27% (65/238). Pulmonary artery pulsatility index <3.5 and pulmonary capillary wedge pressure >19 mm Hg were the most important factors predictive of postcardiotomy cardiogenic shock in ischemic cardiomyopathy. Cardiac index <2.2 L·min m and pulmonary capillary wedge pressure >21 mm Hg were the most important predictive factors in nonischemic cardiomyopathy. Operative mortality was 1.7%. Ejection fraction at 12 months after surgery increased to 39% (confidence interval, 35-40%) in the ischemic group and 37% (confidence interval, 35-38%) in the nonischemic cardiomyopathy group. Predictors of postcardiotomy cardiogenic shock were different in ischemic and nonischemic cardiomyopathy. Right heart dysfunction, indicated by low pulmonary artery pulsatility index, was the most important predictor in ischemic cardiomyopathy, whereas greater degree of cardiac decompensation was the most important in nonischemic cardiomyopathy. Therefore, preoperative right heart catheterization will help identify patients with low ejection fraction who are at greater risk of postcardiotomy cardiogenic shock.
中文翻译:

识别和减轻缺血性和非缺血性心肌病患者心切开术后心源性休克的风险
确定缺血性和非缺血性心肌病患者心切开术后心源性休克的术前预测因素,并评估术后心室功能的轨迹。 2017 年 1 月至 2020 年 1 月,238 名射血分数 <30% (206/238) 或 30% 至 34% 且至少中重度二尖瓣反流的患者 (32/238) 在克利夫兰诊所接受了传统心脏手术,其中 125 名患有缺血性和二尖瓣关闭不全的患者接受了常规心脏手术。 113 患有非缺血性心肌病。术前射血分数为25±4.5%。主要结局是心切开术后心源性休克,定义为需要微轴临时左心室辅助装置、体外膜氧合或血管活性肌力评分>25。 RandomForestSRC 用于识别其预测因子。 27% (65/238) 发生心脏切开术后心源性休克。肺动脉搏动指数<3.5和肺毛细血管楔压>19mmHg是缺血性心肌病心切开术后心源性休克的最重要预测因素。心脏指数<2.2 L·min m 和肺毛细血管楔压>21 mm Hg 是非缺血性心肌病最重要的预测因素。手术死亡率为1.7%。术后 12 个月的射血分数在缺血组中增加至 39%(置信区间,35-40%),在非缺血性心肌病组中增加至 37%(置信区间,35-38%)。缺血性和非缺血性心肌病的心切开术后心源性休克的预测因素是不同的。以低肺动脉搏动指数表示的右心功能障碍是缺血性心肌病最重要的预测因素,而较大程度的心脏代偿失调是非缺血性心肌病最重要的预测因素。因此,术前右心导管检查将有助于识别射血分数低的患者,这些患者发生心脏切开术后心源性休克的风险更大。
更新日期:2024-03-05
中文翻译:

识别和减轻缺血性和非缺血性心肌病患者心切开术后心源性休克的风险
确定缺血性和非缺血性心肌病患者心切开术后心源性休克的术前预测因素,并评估术后心室功能的轨迹。 2017 年 1 月至 2020 年 1 月,238 名射血分数 <30% (206/238) 或 30% 至 34% 且至少中重度二尖瓣反流的患者 (32/238) 在克利夫兰诊所接受了传统心脏手术,其中 125 名患有缺血性和二尖瓣关闭不全的患者接受了常规心脏手术。 113 患有非缺血性心肌病。术前射血分数为25±4.5%。主要结局是心切开术后心源性休克,定义为需要微轴临时左心室辅助装置、体外膜氧合或血管活性肌力评分>25。 RandomForestSRC 用于识别其预测因子。 27% (65/238) 发生心脏切开术后心源性休克。肺动脉搏动指数<3.5和肺毛细血管楔压>19mmHg是缺血性心肌病心切开术后心源性休克的最重要预测因素。心脏指数<2.2 L·min m 和肺毛细血管楔压>21 mm Hg 是非缺血性心肌病最重要的预测因素。手术死亡率为1.7%。术后 12 个月的射血分数在缺血组中增加至 39%(置信区间,35-40%),在非缺血性心肌病组中增加至 37%(置信区间,35-38%)。缺血性和非缺血性心肌病的心切开术后心源性休克的预测因素是不同的。以低肺动脉搏动指数表示的右心功能障碍是缺血性心肌病最重要的预测因素,而较大程度的心脏代偿失调是非缺血性心肌病最重要的预测因素。因此,术前右心导管检查将有助于识别射血分数低的患者,这些患者发生心脏切开术后心源性休克的风险更大。



























 京公网安备 11010802027423号
京公网安备 11010802027423号