当前位置:
X-MOL 学术
›
J. Vasc. Interv. Radiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Modified Radiation Lobectomy Strategy of Radioembolization for Right-Sided Unresectable Primary Liver Tumors
Journal of Vascular and Interventional Radiology ( IF 2.9 ) Pub Date : 2024-03-13 , DOI: 10.1016/j.jvir.2024.03.005 Qian Yu , Yating Wang , Ethan Ungchusri , Anjana Pillai , Chih-yi Liao , John Fung , Diego DiSabato , Talia Baker , Mikin Patel , Thuong Van Ha , Osman Ahmed
Journal of Vascular and Interventional Radiology ( IF 2.9 ) Pub Date : 2024-03-13 , DOI: 10.1016/j.jvir.2024.03.005 Qian Yu , Yating Wang , Ethan Ungchusri , Anjana Pillai , Chih-yi Liao , John Fung , Diego DiSabato , Talia Baker , Mikin Patel , Thuong Van Ha , Osman Ahmed
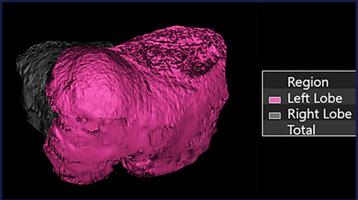
|
To assess the safety and effectiveness of using modified radiation lobectomy (mRL) to treat primary hepatic tumors located in the right hepatic lobe (Segments V–VIII) and determine future liver remnant (FLR) hypertrophy. A retrospective review was performed at a single institution to include 19 consecutive patients (7 females, 12 males) who underwent single-session mRL for right-sided primary hepatic tumors: 15 received segmentectomy plus lobectomy (segmental dose of >190 Gy and lobar dose of >80 Gy); 4 were treated with the double-segmental approach (dominant segments of >190 Gy and nondominant segments of >80 Gy). Treated tumors included 13 hepatocellular carcinoma (HCC), 4 cholangiocarcinoma (CCA), and 2 mixed-type HCC-CCA with a median dominant tumor size of 5.3 cm (interquartile range [IQR], 3.7–7.3 cm). FLR of the left hepatic lobe was measured at baseline, T1 (4–8 weeks), T2 (2–4 months), T3 (4–6 months), and T4 (9–12 months). Objective tumor response and tumor control were achieved in 17 of the 19 (89.5%) and 18 of the 19 (94.7%) patients, respectively. FLR hypertrophy was observed at T1 (median, 47.8%; = .0245), T2 (median, 48.4%; = .0120), T3 (median, 50.4%; = .0147), and T4 (median, 59.1%; = .00023). Patients without cirrhosis demonstrated greater hypertrophy by 6 months (median, 55.8% vs 47.2%; = .0310). One patient developed a Grade 3 adverse event (ascites requiring paracentesis) at 1-month follow-up. Grade 2 or above serum toxicities are associated with worse baseline Child–Pugh Score, serum albumin, and total bilirubin ( < .05). Among 7 patients who underwent neoadjuvant mRL, 2 underwent resection and 1 received liver transplant. mRL appears safe and effective for treatment of right-sided primary hepatic tumors with the benefit of promoting FLR hypertrophy.
中文翻译:

放射栓塞治疗右侧不可切除原发性肝肿瘤的改良放射肺叶切除策略
评估使用改良放射肺叶切除术 (mRL) 治疗位于右肝叶(V-VIII 段)的原发性肝肿瘤的安全性和有效性,并确定未来的肝残余 (FLR) 肥大情况。在同一机构进行了一项回顾性审查,包括 19 名连续接受单次 mRL 治疗右侧原发性肝肿瘤的患者(7 名女性,12 名男性):15 名患者接受了肝段切除加肺叶切除(节段剂量 >190 Gy 和肝叶剂量) >80 Gy); 4 例采用双节段治疗(主导节段 >190 Gy,非主导节段 >80 Gy)。治疗的肿瘤包括 13 例肝细胞癌 (HCC)、4 例胆管癌 (CCA) 和 2 例混合型 HCC-CCA,中位显性肿瘤大小为 5.3 cm(四分位距 [IQR],3.7–7.3 cm)。在基线、T1(4-8 周)、T2(2-4 个月)、T3(4-6 个月)和 T4(9-12 个月)时测量左肝叶 FLR。 19 名患者中的 17 名 (89.5%) 和 19 名患者中的 18 名 (94.7%) 分别实现了客观肿瘤缓解和肿瘤控制。在 T1(中位数,47.8%;= .0245)、T2(中位数,48.4%;= .0120)、T3(中位数,50.4%;= .0147)和 T4(中位数,59.1%;= .0147)观察到 FLR 肥大。 .00023)。无肝硬化的患者在 6 个月时表现出更大的肥厚(中位数,55.8% vs 47.2%;= .0310)。一名患者在 1 个月的随访中出现 3 级不良事件(需要腹腔穿刺术)。 2 级或以上血清毒性与较差的基线 Child-Pugh 评分、血清白蛋白和总胆红素 ( < .05) 相关。 7 例接受新辅助 mRL 的患者中,2 例接受了切除术,1 例接受了肝移植。 mRL 对于治疗右侧原发性肝肿瘤似乎安全有效,并具有促进 FLR 肥大的益处。
更新日期:2024-03-13
中文翻译:

放射栓塞治疗右侧不可切除原发性肝肿瘤的改良放射肺叶切除策略
评估使用改良放射肺叶切除术 (mRL) 治疗位于右肝叶(V-VIII 段)的原发性肝肿瘤的安全性和有效性,并确定未来的肝残余 (FLR) 肥大情况。在同一机构进行了一项回顾性审查,包括 19 名连续接受单次 mRL 治疗右侧原发性肝肿瘤的患者(7 名女性,12 名男性):15 名患者接受了肝段切除加肺叶切除(节段剂量 >190 Gy 和肝叶剂量) >80 Gy); 4 例采用双节段治疗(主导节段 >190 Gy,非主导节段 >80 Gy)。治疗的肿瘤包括 13 例肝细胞癌 (HCC)、4 例胆管癌 (CCA) 和 2 例混合型 HCC-CCA,中位显性肿瘤大小为 5.3 cm(四分位距 [IQR],3.7–7.3 cm)。在基线、T1(4-8 周)、T2(2-4 个月)、T3(4-6 个月)和 T4(9-12 个月)时测量左肝叶 FLR。 19 名患者中的 17 名 (89.5%) 和 19 名患者中的 18 名 (94.7%) 分别实现了客观肿瘤缓解和肿瘤控制。在 T1(中位数,47.8%;= .0245)、T2(中位数,48.4%;= .0120)、T3(中位数,50.4%;= .0147)和 T4(中位数,59.1%;= .0147)观察到 FLR 肥大。 .00023)。无肝硬化的患者在 6 个月时表现出更大的肥厚(中位数,55.8% vs 47.2%;= .0310)。一名患者在 1 个月的随访中出现 3 级不良事件(需要腹腔穿刺术)。 2 级或以上血清毒性与较差的基线 Child-Pugh 评分、血清白蛋白和总胆红素 ( < .05) 相关。 7 例接受新辅助 mRL 的患者中,2 例接受了切除术,1 例接受了肝移植。 mRL 对于治疗右侧原发性肝肿瘤似乎安全有效,并具有促进 FLR 肥大的益处。



























 京公网安备 11010802027423号
京公网安备 11010802027423号