当前位置:
X-MOL 学术
›
J. Thorac. Cardiovasc. Surg.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Ex vivo lung perfusion in donation after circulatory death: A post hoc analysis of the Normothermic Ex Vivo Lung Perfusion as an Assessment of Extended/Marginal Donors Lungs trial
The Journal of Thoracic and Cardiovascular Surgery ( IF 6 ) Pub Date : 2024-03-19 , DOI: 10.1016/j.jtcvs.2024.03.011 Doug A. Gouchoe , Pablo G. Sanchez , Jonathan D’Cunha , Christian A. Bermudez , Mani A. Daneshmand , Robert D. Davis , Matthew G. Hartwig , Thomas C. Wozniak , Zachary N. Kon , Bartley P. Griffith , William R. Lynch , Tiago N. Machuca , Michael J. Weyant , Michael E. Jessen , Michael S. Mulligan , Frank D’Ovidio , Phillip C. Camp , Edward Cantu , Bryan A. Whitson , Pablo G. Sanchez , Robert D. Davis , Matthew G. Hartwig , Tiago N. Machuca , Mani A. Daneshmand , Frank D’Ovidio , John P. Ryan , Jonathan D’Cunha , Christian A. Bermudez , Michael J. Weyant , Michael E. Jessen , Michael S. Mulligan , Thomas Wozniak , William Lynch , Hassan Nemeh , Christiano Caldeira , Tae Song , Daniel Kreisel , Phillip C. Camp , Danny Ramzy , Bartley P. Griffith , Edward Cantu , Bryan A. Whitson
The Journal of Thoracic and Cardiovascular Surgery ( IF 6 ) Pub Date : 2024-03-19 , DOI: 10.1016/j.jtcvs.2024.03.011 Doug A. Gouchoe , Pablo G. Sanchez , Jonathan D’Cunha , Christian A. Bermudez , Mani A. Daneshmand , Robert D. Davis , Matthew G. Hartwig , Thomas C. Wozniak , Zachary N. Kon , Bartley P. Griffith , William R. Lynch , Tiago N. Machuca , Michael J. Weyant , Michael E. Jessen , Michael S. Mulligan , Frank D’Ovidio , Phillip C. Camp , Edward Cantu , Bryan A. Whitson , Pablo G. Sanchez , Robert D. Davis , Matthew G. Hartwig , Tiago N. Machuca , Mani A. Daneshmand , Frank D’Ovidio , John P. Ryan , Jonathan D’Cunha , Christian A. Bermudez , Michael J. Weyant , Michael E. Jessen , Michael S. Mulligan , Thomas Wozniak , William Lynch , Hassan Nemeh , Christiano Caldeira , Tae Song , Daniel Kreisel , Phillip C. Camp , Danny Ramzy , Bartley P. Griffith , Edward Cantu , Bryan A. Whitson
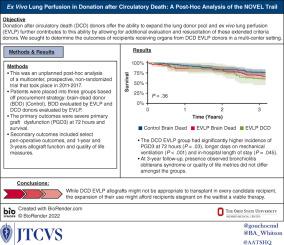
|
Donation after circulatory death (DCD) donors offer the ability to expand the lung donor pool and ex vivo lung perfusion (EVLP) further contributes to this ability by allowing for additional evaluation and resuscitation of these extended criteria donors. We sought to determine the outcomes of recipients receiving organs from DCD EVLP donors in a multicenter setting. This was an unplanned post hoc analysis of a multicenter, prospective, nonrandomized trial that took place during 2011 to 2017 with 3 years of follow-up. Patients were placed into 3 groups based off procurement strategy: brain-dead donor (control), brain-dead donor evaluated by EVLP, and DCD donors evaluated by EVLP. The primary outcomes were severe primary graft dysfunction at 72 hours and survival. Secondary outcomes included select perioperative outcomes, and 1-year and 3-years allograft function and quality of life measures. The DCD EVLP group had significantly higher incidence of severe primary graft dysfunction at 72 hours ( = .03), longer days on mechanical ventilation ( < .001) and in-hospital length of stay ( = .045). Survival at 3 years was 76.5% (95% CI, 69.2%-84.7%) for the control group, 68.3% (95% CI, 58.9%-79.1%) for the brain-dead donor group, and 60.7% (95% CI, 45.1%-81.8%) for the DCD group ( = .36). At 3-year follow-up, presence observed bronchiolitis obliterans syndrome or quality of life metrics did not differ among the groups. Although DCD EVLP allografts might not be appropriate to transplant in every candidate recipient, the expansion of their use might afford recipients stagnant on the waitlist a viable therapy.
中文翻译:

循环死亡后捐献中的离体肺灌注:常温离体肺灌注的事后分析作为扩展/边缘供体肺试验的评估
循环死亡后捐赠 (DCD) 供体提供了扩大肺供体库的能力,而离体肺灌注 (EVLP) 通过允许对这些扩展标准供体进行额外评估和复苏,进一步增强了这种能力。我们试图确定在多中心环境中接受 DCD EVLP 捐献者器官的受者的结果。这是对 2011 年至 2017 年进行的一项多中心、前瞻性、非随机试验进行的计划外事后分析,并进行了 3 年的随访。根据采购策略将患者分为 3 组:脑死亡供体(对照)、通过 EVLP 评估的脑死亡供体和通过 EVLP 评估的 DCD 供体。主要结局是 72 小时时严重的原发性移植物功能障碍和存活率。次要结局包括特定的围手术期结局以及 1 年和 3 年同种异体移植功能和生活质量指标。 DCD EVLP 组在 72 小时内严重原发性移植物功能障碍的发生率 (= .03)、机械通气天数 (< .001) 和住院时间 (= .045) 更长。对照组的 3 年生存率为 76.5%(95% CI,69.2%-84.7%),脑死亡供体组的 3 年生存率为 68.3%(95% CI,58.9%-79.1%),脑死亡供体组的 3 年生存率为 60.7%(95% CI)。 DCD 组的 CI,45.1%-81.8% (= .36)。在 3 年随访中,观察到的闭塞性细支气管炎综合征或生活质量指标在各组之间没有差异。尽管 DCD EVLP 同种异体移植物可能并不适合在每个候选受者中进行移植,但其用途的扩大可能为停滞在等待名单上的受者提供可行的治疗方法。
更新日期:2024-03-19
中文翻译:

循环死亡后捐献中的离体肺灌注:常温离体肺灌注的事后分析作为扩展/边缘供体肺试验的评估
循环死亡后捐赠 (DCD) 供体提供了扩大肺供体库的能力,而离体肺灌注 (EVLP) 通过允许对这些扩展标准供体进行额外评估和复苏,进一步增强了这种能力。我们试图确定在多中心环境中接受 DCD EVLP 捐献者器官的受者的结果。这是对 2011 年至 2017 年进行的一项多中心、前瞻性、非随机试验进行的计划外事后分析,并进行了 3 年的随访。根据采购策略将患者分为 3 组:脑死亡供体(对照)、通过 EVLP 评估的脑死亡供体和通过 EVLP 评估的 DCD 供体。主要结局是 72 小时时严重的原发性移植物功能障碍和存活率。次要结局包括特定的围手术期结局以及 1 年和 3 年同种异体移植功能和生活质量指标。 DCD EVLP 组在 72 小时内严重原发性移植物功能障碍的发生率 (= .03)、机械通气天数 (< .001) 和住院时间 (= .045) 更长。对照组的 3 年生存率为 76.5%(95% CI,69.2%-84.7%),脑死亡供体组的 3 年生存率为 68.3%(95% CI,58.9%-79.1%),脑死亡供体组的 3 年生存率为 60.7%(95% CI)。 DCD 组的 CI,45.1%-81.8% (= .36)。在 3 年随访中,观察到的闭塞性细支气管炎综合征或生活质量指标在各组之间没有差异。尽管 DCD EVLP 同种异体移植物可能并不适合在每个候选受者中进行移植,但其用途的扩大可能为停滞在等待名单上的受者提供可行的治疗方法。



























 京公网安备 11010802027423号
京公网安备 11010802027423号