当前位置:
X-MOL 学术
›
J. Intern. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Impact of nutritional support routes on mortality in acute pancreatitis: A network meta‐analysis of randomized controlled trials
Journal of Internal Medicine ( IF 11.1 ) Pub Date : 2024-04-02 , DOI: 10.1111/joim.13782 Ping‐Han Hsieh, Tsung‐Chieh Yang, Enoch Yi‐No Kang, Pei‐Chang Lee, Jiing‐Chyuan Luo, Yi‐Hsiang Huang, Ming‐Chih Hou, Shih‐Ping Huang
Journal of Internal Medicine ( IF 11.1 ) Pub Date : 2024-04-02 , DOI: 10.1111/joim.13782 Ping‐Han Hsieh, Tsung‐Chieh Yang, Enoch Yi‐No Kang, Pei‐Chang Lee, Jiing‐Chyuan Luo, Yi‐Hsiang Huang, Ming‐Chih Hou, Shih‐Ping Huang
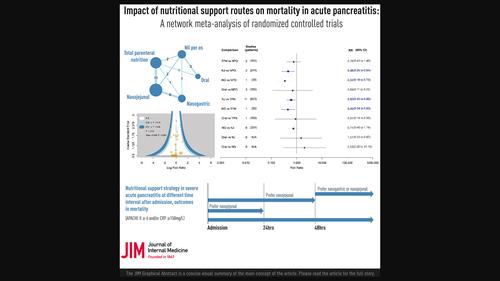
|
BackgroundNutritional administration in acute pancreatitis (AP) management has sparked widespread discussion, yet contradictory mortality results across meta‐analyses necessitate clarification. The optimal nutritional route in AP remains uncertain. Therefore, this study aimed to compare mortality among nutritional administration routes in patients with AP using consistency model.MethodsThis study searched four major databases for relevant randomized controlled trials (RCTs). Two authors independently extracted and checked data and quality. Network meta‐analysis was conducted for estimating risk ratios (RRs) with 95% confidence interval (CI) based on random‐effects model. Subgroup analyses accounted for AP severity and nutrition support initiation.ResultsA meticulous search yielded 1185 references, with 30 records meeting inclusion criteria from 27 RCTs (n = 1594). Pooled analyses showed the mortality risk reduction associated with nasogastric (NG) (RR = 0.34; 95%CI: 0.16–0.73) and nasojejunal (NJ) feeding (RR = 0.46; 95%CI: 0.25–0.84) in comparison to nil per os. Similarly, NG (RR = 0.45; 95%CI: 0.24–0.83) and NJ (RR = 0.60; 95%CI: 0.40–0.90) feeding also showed lower mortality risk than total parenteral nutrition. Subgroup analyses, stratified by severity, supported these findings. Notably, the timing of nutritional support initiation emerged as a significant factor, with NJ feeding demonstrating notable mortality reduction within 24 and 48 h, particularly in severe cases.ConclusionFor severe AP, both NG and NJ feeding appear optimal, with variations in initiation timings. NG feeding does not appear to merit recommendation within the initial 24 h, whereas NJ feeding is advisable within the corresponding timeframe following admission. These findings offer valuable insights for optimizing nutritional interventions in AP.
中文翻译:

营养支持途径对急性胰腺炎死亡率的影响:随机对照试验的网络荟萃分析
背景急性胰腺炎(AP)治疗中的营养管理引发了广泛的讨论,但荟萃分析中相互矛盾的死亡率结果需要澄清。 AP 的最佳营养途径仍不确定。因此,本研究旨在利用一致性模型比较AP患者营养给药途径的死亡率。方法本研究检索四大数据库中的相关随机对照试验(RCT)。两位作者独立提取并检查数据和质量。进行网络荟萃分析,以基于随机效应模型的 95% 置信区间 (CI) 估计风险比 (RR)。亚组分析考虑了 AP 严重程度和营养支持启动。结果经过细致的搜索,产生了 1185 条参考文献,其中 30 条记录符合 27 项 RCT 的纳入标准(n = 1594)。汇总分析显示,与无死亡率风险相比,鼻胃管 (NG)(RR = 0.34;95%CI:0.16–0.73)和鼻空肠 (NJ) 喂养(RR = 0.46;95%CI:0.25–0.84)可降低死亡风险。操作系统。同样,NG(RR = 0.45;95%CI:0.24–0.83)和 NJ(RR = 0.60;95%CI:0.40–0.90)喂养也显示出比全肠外营养更低的死亡风险。按严重程度分层的亚组分析支持了这些发现。值得注意的是,开始营养支持的时间是一个重要因素,NJ 喂养在 24 和 48 小时内显示死亡率显着降低,特别是在严重病例中。结论对于严重 AP,NG 和 NJ 喂养似乎都是最佳的,但起始时间有所不同。 NG 喂养似乎不值得在最初 24 小时内推荐,而 NJ 喂养则建议在入院后相应的时间范围内进行。这些发现为优化 AP 营养干预措施提供了宝贵的见解。
更新日期:2024-04-02
中文翻译:

营养支持途径对急性胰腺炎死亡率的影响:随机对照试验的网络荟萃分析
背景急性胰腺炎(AP)治疗中的营养管理引发了广泛的讨论,但荟萃分析中相互矛盾的死亡率结果需要澄清。 AP 的最佳营养途径仍不确定。因此,本研究旨在利用一致性模型比较AP患者营养给药途径的死亡率。方法本研究检索四大数据库中的相关随机对照试验(RCT)。两位作者独立提取并检查数据和质量。进行网络荟萃分析,以基于随机效应模型的 95% 置信区间 (CI) 估计风险比 (RR)。亚组分析考虑了 AP 严重程度和营养支持启动。结果经过细致的搜索,产生了 1185 条参考文献,其中 30 条记录符合 27 项 RCT 的纳入标准(



























 京公网安备 11010802027423号
京公网安备 11010802027423号