当前位置:
X-MOL 学术
›
J. Vasc. Surg.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Surgeon volume and outcomes following thoracic endovascular aortic repair for blunt thoracic aortic injury
Journal of Vascular Surgery ( IF 4.3 ) Pub Date : 2024-03-01 , DOI: 10.1016/j.jvs.2024.02.032 Tim J. Mandigers , Sai Divya Yadavalli , Vinamr Rastogi , Christina L. Marcaccio , Sophie X. Wang , Sara L. Zettervall , Benjamin W. Starnes , Hence J.M. Verhagen , Joost A. van Herwaarden , Santi Trimarchi , Marc L. Schermerhorn
Journal of Vascular Surgery ( IF 4.3 ) Pub Date : 2024-03-01 , DOI: 10.1016/j.jvs.2024.02.032 Tim J. Mandigers , Sai Divya Yadavalli , Vinamr Rastogi , Christina L. Marcaccio , Sophie X. Wang , Sara L. Zettervall , Benjamin W. Starnes , Hence J.M. Verhagen , Joost A. van Herwaarden , Santi Trimarchi , Marc L. Schermerhorn
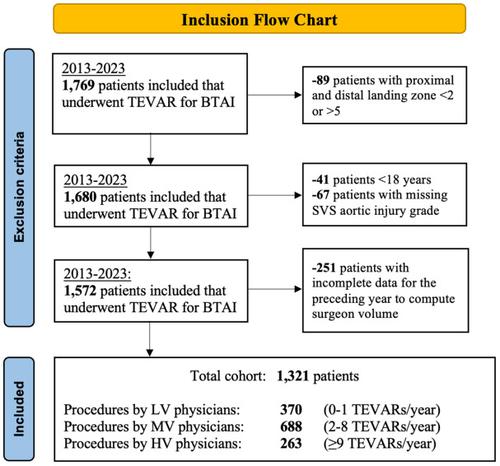
|
Thoracic endovascular aortic repair (TEVAR) for blunt thoracic aortic injury (BTAI) at high-volume hospitals has previously been associated with lower perioperative mortality, but the impact of annual surgeon volume on outcomes following TEVAR for BTAI remains unknown. We analyzed Vascular Quality Initiative (VQI) data from patients with BTAI that underwent TEVAR between 2013 and 2023. Annual surgeon volumes were computed as the number of TEVARs (for any pathology) performed over a 1-year period preceding each procedure and were further categorized into quintiles. Surgeons in the first volume quintile were categorized as low volume (LV), the highest quintile as high volume (HV), and the middle three quintiles as medium volume (MV). TEVAR procedures performed by surgeons with less than 1-year enrollment in the VQI were excluded. Using multilevel logistic regression models, we evaluated associations between surgeon volume and perioperative outcomes, accounting for annual center volumes and adjusting for potential confounders, including aortic injury grade and severity of coexisting injuries. Multilevel models accounted for the nested clustering of patients and surgeons within the same center. Sensitivity analysis excluding patients with grade IV BTAI was performed. We studied 1321 patients who underwent TEVAR for BTAI (28% by LV surgeons [0-1 procedures per year], 52% by MV surgeons [2-8 procedures per year], 20% by HV surgeons [≥9 procedures per year]). With higher surgeon volume, TEVAR was delayed more (in <4 hours: LV: 68%, MV: 54%, HV: 46%; < .001; elective (>24 hours): LV: 5.1%; MV: 8.9%: HV: 14%), heparin administered more (LV: 80%, MV: 81%, HV: 87%; = .007), perioperative mortality appears lower (LV: 11%, MV: 7.3%, HV: 6.5%; = .095), and ischemic/hemorrhagic stroke was lower (LV: 6.5%, MV: 3.6%, HV: 1.5%; = .006). After adjustment, compared with LV surgeons, higher volume surgeons had lower odds of perioperative mortality (MV: 0.49; 95% confidence interval [CI], 0.25-0.97; = .039; HV: 0.45; 95% CI, 0.16–1.22; = .12; MV/HV: 0.50; 95% CI, 0.26-0.96; = .038) and ischemic/hemorrhagic stroke (MV: 0.38; 95% CI, 0.18-0.81; = .011; HV: 0.16; 95% CI, 0.04-0.61; = .008). Sensitivity analysis found lower adjusted odds for perioperative mortality (although not significant) and ischemic/hemorrhagic stroke for higher volume surgeons. In patients undergoing TEVAR for BTAI, higher surgeon volume is independently associated with lower perioperative mortality and postoperative stroke, regardless of hospital volume. Future studies could elucidate if TEVAR for non-ruptured BTAI might be delayed and allow stabilization, heparinization, and involvement of a higher TEVAR volume surgeon.
中文翻译:

胸主动脉闭合性损伤胸主动脉腔内修复术后的外科医生数量和结果
此前,在大型医院进行胸主动脉腔内修复术 (TEVAR) 治疗钝性胸主动脉损伤 (BTAI) 曾被认为与较低的围手术期死亡率相关,但每年外科医生数量对 BTAI TEVAR 治疗结果的影响仍不清楚。我们分析了 2013 年至 2023 年间接受 TEVAR 的 BTAI 患者的血管质量倡议 (VQI) 数据。年度外科医生手术量计算为每次手术前 1 年内进行的 TEVAR(针对任何病理)的数量,并进一步分类分成五分位数。第一个五分位的外科医生被归类为低容量(LV),最高五分位的外科医生被归类为高容量(HV),中间三个五分位的外科医生被归类为中容量(MV)。由加入 VQI 不足 1 年的外科医生进行的 TEVAR 手术被排除在外。使用多级逻辑回归模型,我们评估了外科医生手术量和围手术期结果之间的关联,考虑了年度中心手术量并调整了潜在的混杂因素,包括主动脉损伤等级和共存损伤的严重程度。多级模型考虑了同一中心内患者和外科医生的嵌套聚类。进行了排除 IV 级 BTAI 患者的敏感性分析。我们研究了 1321 名接受 TEVAR 治疗 BTAI 的患者(28% 由左室外科医生 [每年 0-1 次手术],52% 由中静脉外科医生 [每年 2-8 次手术],20% 由高压外科医生 [每年≥9 次手术] )。随着外科医生手术量的增加,TEVAR 延迟得更多(<4 小时内:LV:68%,MV:54%,HV:46%;< .001;选择性(>24 小时):LV:5.1%;MV:8.9% :HV:14%),肝素用量较多(LV:80%,MV:81%,HV:87%;= .007),围手术期死亡率似乎较低(LV:11%,MV:7.3%,HV:6.5%) ; = .095),缺血性/出血性中风较低(LV:6.5%,MV:3.6%,HV:1.5%;= .006)。调整后,与左室外科医生相比,手术量较大的外科医生围手术期死亡率较低(MV:0.49;95% 置信区间 [CI],0.25-0.97;= 0.039;HV:0.45;95% CI,0.16-1.22; = .12;MV/HV:0.50;95% CI,0.26-0.96;= .038)和缺血性/出血性中风(MV:0.38;95% CI,0.18-0.81;= .011;HV:0.16;95% CI,0.04-0.61;= .008)。敏感性分析发现,对于高手术量的外科医生来说,围手术期死亡率(尽管不显着)和缺血性/出血性中风的调整后赔率较低。在接受 TEVAR 治疗 BTAI 的患者中,无论医院规模如何,较高的外科医生数量与较低的围手术期死亡率和术后卒中独立相关。未来的研究可以阐明非破裂 BTAI 的 TEVAR 是否可以延迟,并允许稳定、肝素化以及更高 TEVAR 体积的外科医生的参与。
更新日期:2024-03-01
中文翻译:

胸主动脉闭合性损伤胸主动脉腔内修复术后的外科医生数量和结果
此前,在大型医院进行胸主动脉腔内修复术 (TEVAR) 治疗钝性胸主动脉损伤 (BTAI) 曾被认为与较低的围手术期死亡率相关,但每年外科医生数量对 BTAI TEVAR 治疗结果的影响仍不清楚。我们分析了 2013 年至 2023 年间接受 TEVAR 的 BTAI 患者的血管质量倡议 (VQI) 数据。年度外科医生手术量计算为每次手术前 1 年内进行的 TEVAR(针对任何病理)的数量,并进一步分类分成五分位数。第一个五分位的外科医生被归类为低容量(LV),最高五分位的外科医生被归类为高容量(HV),中间三个五分位的外科医生被归类为中容量(MV)。由加入 VQI 不足 1 年的外科医生进行的 TEVAR 手术被排除在外。使用多级逻辑回归模型,我们评估了外科医生手术量和围手术期结果之间的关联,考虑了年度中心手术量并调整了潜在的混杂因素,包括主动脉损伤等级和共存损伤的严重程度。多级模型考虑了同一中心内患者和外科医生的嵌套聚类。进行了排除 IV 级 BTAI 患者的敏感性分析。我们研究了 1321 名接受 TEVAR 治疗 BTAI 的患者(28% 由左室外科医生 [每年 0-1 次手术],52% 由中静脉外科医生 [每年 2-8 次手术],20% 由高压外科医生 [每年≥9 次手术] )。随着外科医生手术量的增加,TEVAR 延迟得更多(<4 小时内:LV:68%,MV:54%,HV:46%;< .001;选择性(>24 小时):LV:5.1%;MV:8.9% :HV:14%),肝素用量较多(LV:80%,MV:81%,HV:87%;= .007),围手术期死亡率似乎较低(LV:11%,MV:7.3%,HV:6.5%) ; = .095),缺血性/出血性中风较低(LV:6.5%,MV:3.6%,HV:1.5%;= .006)。调整后,与左室外科医生相比,手术量较大的外科医生围手术期死亡率较低(MV:0.49;95% 置信区间 [CI],0.25-0.97;= 0.039;HV:0.45;95% CI,0.16-1.22; = .12;MV/HV:0.50;95% CI,0.26-0.96;= .038)和缺血性/出血性中风(MV:0.38;95% CI,0.18-0.81;= .011;HV:0.16;95% CI,0.04-0.61;= .008)。敏感性分析发现,对于高手术量的外科医生来说,围手术期死亡率(尽管不显着)和缺血性/出血性中风的调整后赔率较低。在接受 TEVAR 治疗 BTAI 的患者中,无论医院规模如何,较高的外科医生数量与较低的围手术期死亡率和术后卒中独立相关。未来的研究可以阐明非破裂 BTAI 的 TEVAR 是否可以延迟,并允许稳定、肝素化以及更高 TEVAR 体积的外科医生的参与。



























 京公网安备 11010802027423号
京公网安备 11010802027423号