Abstract
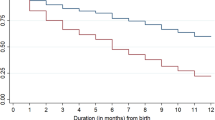
Maternal age is one of the strongest predictors of infant mortality. Despite the relatively high prevalence of childbearing at younger and advanced ages and high infant mortality rates in India, systematic studies on the relationship between these variables are lacking. This study fills this gap by analyzing the data obtained from 2015-16 India’s National Family Health Survey. The analysis is based on a sample of 230,475 children born in the 5 years preceding the survey. We find that, generally, there is a mild U-shaped relationship between maternal age and mortality risk in the first year of life, with children born to mothers in their teens and late 30s and beyond being most at risk and those born to mothers aged 25–29 being least at risk. In addition, we find that socioeconomic, biodemographic, and other health-related factors account for some, but not all, maternal-age effects on mortality, suggesting that maternal age is an independent risk factor for both neonatal and post-neonatal mortality. While biodemographic and other health-related factors play important roles in explaining why children born to mothers at both ends of the reproductive-age spectrum are at significantly increased risks, the effects of socioeconomic factors are relatively modest, and that is the case among children born to mothers at advanced ages only. The results underscore the importance of maternal and child health care policies, which can help teenage mothers postpone having children until their late 20s, not have a child shortly after the preceding birth, and continuously monitor the health conditions of low-birthweight children.
Résumé
L'âge maternel est l'un des prédicteurs les plus importants de la mortalité infantile. Malgré la prévalence relativement élevée de la maternité aux jeunes âges et aux âges avancés et des taux de mortalité infantile élevés en Inde, il n'y pas des études systématiques sur la relation entre ces variables. Cette étude comble cette lacune en analysant les données obtenues de l’enquête nationale sur la santé de la famille en Inde de 2015-2016. L'analyse est basée sur un échantillon de 230 475 enfants nés dans les 5 années précédant l'enquête. Nous constatons qu'en général, il existe une légère relation en forme de U entre l'âge maternel et le risque de mortalité au cours de la première année de vie, les enfants nés de mères adolescentes et à la fin de la trentaineet au-delà étant les plus vulnérables à risque et ceux nés à les mères âgées de 25 à 29 ans étant les moins à risque. En outre, nous constatons que les facteurs socioéconomiques, biodémographiques et les autres facteurs liés à la santé expliquent certains effets de l'âge maternel sur la mortalité, mais pas tous, ce qui suggère que l'âge maternel est un facteur de risque indépendant de mortalité néonatale et post-néonatale. Alors que les facteurs biodémographiques et autres facteurs liés à la santé jouent un rôle important dans l'explication des raisons pour lesquelles les enfants nés de mères aux deux extrémités de l'éventail de l'âge de la procréation sont exposés à des risques considérablement accrus, les effets des facteurs socio-économiquessont relativement modestes, et c'est également le cas chez les enfants. nés de mères à un âge avancé seulement. Les résultats soulignent l'importance des politiques de santé maternelle et infantile, qui peuvent aider les mères adolescentes à différer leurs projets de maternité jusqu'à la fin de la vingtaine, à ne pas avoir des naissances trop rapprochées et à surveiller l'état de santé des enfants de faible poids à la naissance.

Similar content being viewed by others
References
Aasheim, V., Waldenstrom, U., Hjelmstedt, A., Rasmussen, S., Pettersson, H., & Schytta, E. (2012). Associations between advanced maternal age and psychological distress in primiparous women, from early pregnancy to 18 months postpartum. BJOG: International Journal of Obstetrics and Gynaecology, 119, 1108–1116.
Aldous, M. B., & Edmonson, M. B. (1993). Maternal age at first childbirth and risk of low birth weight and preterm delivery in Washington State. Journal of American Medical Association, 270, 2574–2577.
An, C. B., Haveman, R., & Wolfe, B. (1993). Teen out-of-wedlock births and welfare receipt: The role of childhood events and economic circumstances. Review of Economics and Statistics, 75, 195–208.
Aras, R. Y. (2015). Is maternal age a risk factor for low birth weight? Achieves of Medicine and Health Sciences, 1, 33–37.
Barclay, K., & Myrskylä, M. (2016). Maternal age and offspring health and health behaviors in late adolescence in Sweden. Social Science and Medicine – Population Health, 2, 68-76.
Bassani, D. G., & Jha, P. (2010). Causes of neonatal and child mortality in India: Nationally representative mortality survey. Lancet, 376, 1853–1860. https://doi.org/10.1016/S0140-6736(10)61461-4 Published online 2010 Nov 12.
Bissell, M. (2000). Socio-economic outcomes of teen pregnancy and parenthood: A review of the literature. Canadian Journal of Human Sexuality, 9, 191–204.
Blomberg, M., Birch, T. R., & Kjølhede, P. (2014). Impact of maternal age on obstetric and neonatal outcome with emphasis on primiparous adolescents and older women: a Swedish Medical Birth Register Study. British Medical Journal Open, 4(11), e005840. https://doi.org/10.1136/bmjopen-2014-05840.
Cavazos-Rehg, P. A., Krauss, M. J., Spitznagel, E. L., Bommarito, K., Madden, T., Olsen, M. A., Subramaniam, H., Peipert, J. F., & Bierut, L. J. (2015). Maternal age and risk of labor and delivery complications. Maternal and Child Health Journal, 19, 1202–1211.
Chen, X.-K., Wen, S. W., Fleming, N., Demissie, K., George, G., Rhoads, G., & Mark Walker, M. (2007). Teenage pregnancy and adverse birth outcomes: A large population-based retrospective cohort study. International Journal of Epidemiology, 36, 368–373.
Cnattingius, S., Foreman, M. R., Berendes, H. W., & Isotalo, L. (1992). Delayed childbearing and risk of adverse perinatal outcome. A population-based study. Journal of American Medical Association, 268, 886–890.
Conde-Agudelo, A., Belizan, J. M., & Lammers, C. (2005). Maternal-perinatal morbidity and mortality associated with adolescent pregnancy in Latin America: A cross-sectional study. American Journal of Obstetrics and Gynecology, 192, 342–349.
DaVanzo, J., Hale, L., Razzaque, A., & Rahman, M. (2008). The effects of pregnancy spacing on infant and child mortality in Matlab, Bangladesh: How they vary by the type of pregnancy outcome that began the interval. Population Studies, 62, 131–154.
Fall, C., Sachdev, H. S., Osmond, C., Restrepo-Mentez, M. C., Victoria, C., et al. (2015). Association between maternal age at childbirth and child and adult outcomes in the offspring: A prospective study in five low-income and middle-income countries (COHORTS collaboration). Lancet Global Health, 3, e341–e422.
Finer, L. B., & Zolna, M. R. (2016). Declines in unintended pregnancy in the United States, 2008–2011. New England Journal of Medicine, 374, 843–852.
Finlay, J. E., Ozaltin, E., & Canning, D. (2011). The association of maternal age with infant mortality, child anthropometric failure, diarrhea, and anemia for first births: evidence from 55 low- and middle-income countries. British Medical Journal Open, 1, e00022. https://doi.org/10.1136/bmjopen-2011-00226.
Fosto, J. C., Cleland, J., Mberu, B., Mutua, M., & Elungata, P. (2013). Birthsapcing and child mortality: An analysis of prospective data from the Nairobi Urban Health and Demographic Surveillance System. Journal of Bioscial Science, 45, 779–798.
Fraser, A. M., Brockert, J. E., & Ward, R. H. (1995). Association of young maternal age with adverse reproductive outcomes. New England Journal of Medicine, 332, 1113–1118.
Friede, A., Baldwin, W., Rhodes, P. H., Buehler, J. W., Strauss, L. T., Smith, J. C., & Hogue, C. J. (1987). Young maternal age and infant mortality: The role of low birth weight. Public Health Reports, 102, 192–199.
Geronimus, A. T. (1987). On teenage childbearing and neonatal mortality in the United States. Population and Development Review, 13, 245–279.
Geronimus, A. T., & Korenman, S. (1993). Maternal youth or family background?—On the health disadvantages of infants with teenage mothers. American Journal of Epidemiology, 137, 213–225.
Geronimus, A. T., Korenman, S., & Hillemeier, M. M. (1994). Does young maternal age adversely affect child development? Evidence from cousin comparisons in the United States. Population and Development Review, 20, 585–609.
Gibbs, C. A., Wendt, A., Peters, S., & Hogue, C. J. (2012). The impact of early age at first childbirth on maternal and infant health. Paediatrics Perinatal Epidemiology, 26, 259–284.
Goisis, A., Remes, H., Barclay, K., Martikainen, P., & Myrskylä, M. (2017). Advanced maternal age and the risk of low birth weight and preterm delivery: A within-familyanalysis using Finnish population registers. American Journal of Epidemiology, 186, 1219–2126.
Hoffman, M. C., Jeffers, S., Carter, J., Duthely, L., Cotter, A., & González-Quintero, V. H. (2007). Pregnancy at or beyond age 40 years is associated with an increased risk of fetal death and other adverse outcomes. American Journal of Obstetrics and Gynecology, 196, e11–e13.
Huang, L., Sauve, R., Birkett, N., Fergusson, D., & van Walraven, C. (2008). Maternal age and risk of stillbirth: A systematic review. Canadian Medical Association Journal, 178, 165–172.
IIPS and ICF. (2017). National Family Health Survey (NFHS-4) 2015–16. International Institute for Population Sciences.
Kamal, S. M. M. (2015). What is the association between maternal age and neonatal mortality? An Analysis of the 2007 Bangladesh Demographic and Health Survey. Asia-Pacific Journal of Public Health, 27, 106–117.
Kane, J. B., Morgan, S. P., Harris, K. M., & Guilkey, D. K. (2013). The educational consequencesof teen childbearing. Demography, 50, 2129–2150.
Knodel, J., & Hermalin, A. I. (1984). Effects of birth rank, maternal age, birth interval, and sibship size on infant and child mortality: Evidence from 18th and 19th-century reproductive histories. American Journal of Public Health, 74, 1098–1106.
Kozuki, N., Lee, A. C., et al. (2013). The associations of parity and maternal age with small-for-gestational-age, preterm, and neonatal and infant mortality: A meta-analysis. BMC PublicHealth, 13(Suppl 3), S2. https://doi.org/10.1186/1471-2458-13-S3-S2.
Kramer, K. L., & Lancaster, J. B. (2010). Teen motherhood in cross-cultural perspective. Annals of Human Biology, 37, 613–628.
Kumar, C., Singh, P. K., & Singh, L. (2013). Early neonatal mortality in India, 1990–2006. Journal of Community Health, 38, 120–130.
Liu, Y., Zhi, M., & Li, X. (2011). Parental age and characteristics of the offspring. Ageing Research Reviews, 10(1), 115–123. https://doi.org/10.1016/j.arr.2010.09.004.
Markovitz, B. P., Cook, R., Flick, L. H., Flick, L. H., & Leet, T. L. (2005). Socioeconomic factor and adolescent pregnancy outcomes: Distinctions between neonatal and post-neonatal deaths? BMC Public Health, 5, 79. https://doi.org/10.1186/1471-2458-5-79.
Mirowsky, J., & Ross, C. E. (2002). Depression, parenthood, and age at first birth. Social Science and Medicine, 54, 1281–1298.
Mishra, S. K., Ram, B., Singh, A., & Yadav, A. (2018). Birth order, stage of infancy, and infant mortality in India. Journal of Biosocial Science, 50, 604–625.
Mosley, W. H., & Chen, C. (1984). An analytical framework for the study of child survival in developing countries. Population and Development Review, 10(supplement), 25–45.
Myrskyla, M., & Fenelon, A. (2012). Maternal age and offspring adult health: Evidence from the Health and Retirement Study. Demography, 49, 1231–1257.
Neal, S., Channon, A. A., Chintsanya, J. (2018) The impact of young maternal age at birth on neonatal mortality: Evidence from 45 low and middle-income countries. PLoS ONE, 13(5). https://doi.org/10.1371/journal.pone.0195731.
Olausson, P. O., Cnattingius, S., & Haglund, B. (1999). Teenage pregnancies and risk of late fetal death and infant mortality. British Journal of Obstetrics and Gynaecology, 106, 116–121.
Penman-Aguilar, A., Crater, M., Christine Snead, M., & Kourtis, A. P. (2013). Socioeconomic disadvantage as a social determinant of teen childbearing in the U.S. Public Health Reports, 128, 5–22.
Puffer, R. R., Serrano, C. V. (1975). Birth-weight, maternal age and birth order: Three important determinants of infant mortality. Pan American Health Organization, World Health Organization.
Raj, A., Saggurti, N., Winter, M., Labonte, A., Decker, M. R., Balaiah, D., & Silverman, J. G. (2010). The effect of maternal child marriage on morbidity and mortality of children under 5 in India: a cross-sectional study of a nationally representative sample. British Medical Journal, 340, b4258. https://doi.org/10.1136/bmj.b4258.
Ram, B., Ram, S. S., & Yadav, A. (2019). The effect of a child’s body size at birth on infant and child mortality in India. Canadian Studies in Population, 46, 77–98.
Reddy, U. M., Ko, C. W., & Willinger, M. (2006). Maternal age and the risk of stillbirth throughout pregnancy in the United States. American Journal of Obstetrics and Gynecology, 195, 764–770.
Reichman, N. E., & Pagnini, D. L. (1997). Maternal age and birth outcomes: Data from New Jersey. Family Planning Perspectives, 29, 268–272.
Roth, J., Hendrickson, J., Schilling, M., & Stowell, D. (1998). The risk of teen mothers having low birth weight babies: Implications for recent medical research for school health personnel. Journal of School Health, 68, 271–275.
Rutstein, S. O. (2005). Effects of preceding birth intervals on neonatal, infant and under five years mortality and nutritional status in developing countries: Evidence from the demographic and health surveys. International Journal of Gynecology and Obstetric, 89, S7-24.
Rutstein, S. O., & Winter, R. (2014). The effects of fertility behavior on child survival and child nutritional status: Evidence from the Demographic and Health Surveys, 2006 to 2012. DHS Analytical Studies No. 37. ICF International.
Scholl, T. O., Hediger, M. L., Schall, J. I., Khoo, C. S., & Fischer, R. L. (1994). Maternal growth during pregnancy and the competition for nutrients. American Journal of Clinical Nutrition, 60, 183–188.
Schummers, L., Hutcheon, J. A., Hernandez-Diaz, S., Williams, P. L., Hacker, M. R., VenderWell, T. J., & Norman, W. V. (2018). Association of short interpregnancy interval with pregnancy outcomes according to maternal age. Journal of American Medical Association Internal Medicine, 178, 1661–1670.
Singh, A., Kumar, A., Kumar, A. (2013).Determinants of neonatal mortality in rural India 2007–2008. Peer J. https://doi.org/10.7717/peerj.75.
Sinha, S., Aggarwal, A. R., Osmond, C., Fall, C. H. D., Bhargava, S. K., & Sachdev, H. S. (2016). Association between maternal age at childbirth and perinatal and under-five mortality in a prospective birth cohort from Delhi. Indian Pediatrics, 53, 871–877.
UNICEF. (2017). Levels and trends of child mortality: Report 2017. UNICEF.
Van der Klaauw, B., & Wang, L. (2011). Child mortality in rural India. Journal of Population Economics, 24, 601–628.
Weng, Y.-H., Yang, C.-Y., Chiu, Y. W. (2014) Risk assessment of adverse birth outcomes in relation to maternal age. PLoS ONE, 9. https://doi.org/10.1371/journal.pone.0114843.
Whitworth, A., & Stephenson, R. (2002). Birth spacing, sibling rivalry, and child mortality in India. Social Science and Medicine, 55, 2107–2119.
Acknowledgements
We are thankful to Anshumala Ram, R. D. Sharma, and two anonymous referees for their helpful comments on an earlier draft.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research Involving Human Participants and/or Animals
Not Applicable.
Informed Consent
Not Applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ram, S.S., Ram, B. & Yadav, A. The Effects of Maternal Age on Neonatal and Post-neonatal Mortality in India: Roles of Socioeconomic and Biodemographic Factors. Can. Stud. Popul. 48, 59–89 (2021). https://doi.org/10.1007/s42650-021-00041-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42650-021-00041-3
Keywords
- Infant mortality
- Neonatal mortality
- Post-neonatal mortality
- Maternal age
- Teenage motherhood
- Advanced-age motherhood
- Biodemographic factors