Abstract
The emergence of the current global crisis induced by the rapid spread of the COVID-19 pandemic brings about an urgent need to rethink and reshape recovery strategies adapted to this specific challenging context. Neglecting this reconfiguration could lead to system lockdown, affecting all sectors, both on medium and long term. The coronavirus has penetrated various countries with different degrees of intensity, thus being spatially diversified; even within the same country, with the same lockdown measures, an enormous variety in cases is encountered. Subsequently, even if crises may manifest heterogeneously and the long-term impact of implementing recovery policies cannot be accurately known ex ante by governments, institutions could adapt themselves to changing circumstances and respond promptly and appropriately to emerging shocks only if their functioning framework had been well set up by the outbreak of the crisis. Considering these aspects, the main questions that this paper aims to answer are: How effective have governmental measures in European countries been in combating the COVID-19 crisis?; Could the solutions offered by the European states’ governments have an influence on diminishing the intensity of negative effects of a possible more serious return of this health crisis? What more could national authorities and international actors do to control the epidemiological evolution of SARS-CoV-2? Is a generic European Union policy helpful or should there be a case for local policy? Based on these issues, a comprehensive picture of the differences between the East and the West of Europe in terms of some medical, socio-economic, institutional and cultural factors will be outlined, in order to emphasize which of the two groups better-handled the COVID-19 situation in the first wave, covering the lockdown period (March 1, 2020 – June 1, 2020) and the relaxation period (June 1, 2020 – September 1, 2020); at the same time, some policy recommendations on how governments should more effectively manage future similar crises to generate a higher resilience of the systems will be provided.
Similar content being viewed by others
Introduction
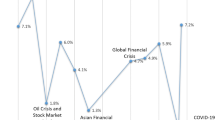
Epidemics have always affected societies at a multidimensional level: economic, social, institutional, cultural, etc. (McMillen, 2013). This is as valid today as it ever was, given the large-scale challenges and implications of the coronavirus pandemic worldwide. Since March 13th, 2020, when the World Health Organization (WHO) officially declared the novel coronavirus disease (COVID-19) a pandemic, “the humankind is experiencing an ongoing global crisis, which is unique in terms of spatial extent, rapid onset and its complexity of consequences” (Cheval et al., 2020, p. 2). Subsequently, the current COVID-19 pandemic induced the most severe crisis that the world has known over the past century, in terms of affected countries, and given the economic, health and social issues it poses. From an economic standpoint, this pandemic has hit the world economy, practically representing “the biggest shock installed after World War II” (IMF, 2020; OECD, 2020a), weighing heavily on world trade, with various industries that shut down and countries that closed their borders. Governments and international institutions have been on board since the outbreak to better mitigate its harmful repercussions through interventions in financial markets, offering governmental support and aid to vulnerable individuals and firms, and adopting measures to cope with growing budget deficits. In this context, it becomes clear that the COVID-19 pandemic is likely to have a long-term impact on the social (especially health), economic and governance systems, far beyond current times.
The literature (Arnold, 2018; Barry, 2005; Gualde, 2016; Outka, 2020; Spinney, 2018) has highlighted, over time, the negative effects of such humanitarian disasters around the world (e.g., the 1918–19 Spanish flu or Great Influenza epidemic) which, in addition to the significant death toll, also meant a social collapse and a paradigm shift in the sphere of culture. Although the previous crises differ in scale, there might be some insights that they could offer for exploring what should be done in order to diminish the impact of COVID-19 (Ali & Alharbi, 2020). However, the current SARS-CoV-2 virus could provide relevant information as the first wave alone came with more than 35 million reported infections worldwide and a mortality rate estimated at 3.4% (WHO, 2020b). This virus is part of the coronaviruses group which are generally of very high societal concern (Memish et al., 2020), claiming to this date (April 2022) over 6 million deaths and over half a billion infections around the world (Worldometer, 2022). Furthermore, since the initial outbreak in Wuhan, several countries around the globe have experienced multiple waves of coronavirus outbreaks, with surges in new cases followed by declines. Besides these, since the outbreak, the SARS-CoV-2 has also mutated, resulting in variants of the virus (like Delta, Omicron, etc.), which make infections possible even among the vaccinated population. Under this dynamic context, overcoming the ongoing crisis crucially depends on whether European countries will be able to better coordinate their responses and to deliver collectively, which will require fast and decisive joint action, including unconditional and effective solidarity.
Undoubtedly, the multidimensional impact of COVID-19 pandemic has radically reconfigured the realities of European Union’s (EU) Member States, which, during the year 2020, registered over half a million deaths due to the SARS-CoV-2, according to Worldometer. Meanwhile, the EU governments’ responses, consisting in several restrictive measures designed to contain the emerging health crisis, have also led to dire economic consequences as the EU’s GDP in 2020 met a record high contraction of 6.4% (Eurostat, 2020). Nevertheless, we have come a long way since the initial outbreak, with countries in Europe and beyond becoming more resilient and proficient in addressing the coronavirus, from mass-vaccination campaigns to reforms for enhanced digitalisation of governmental processes and institutions, but also for education (online schooling) and labour (remote work). However, considering that the first wave of the pandemic and its unprecedented consequences took the EU governments by surprise, the majority of measures were uncoordinated and more difficult to implement. As such, although we have been witnessing four waves with their specific impacts, patterns and territorial distribution, the first wave remains an interesting and relevant period of analysis.
The study generally aims at highligting the relation between governments’ responses and the COVID-19 death rate in Europe during the first wave, in order to identify the main drivers (factors) that have enhanced the countries’ ability to better withstand and cope with the pandemic’s severe negative effects. In this regard, the study is focused on a 6-month timeframe, thus covering two specific periods: the first period, known as the lockdown (March 1, 2020 – June 1, 2020) and the second period of relaxation with restrictions being lifted (June 1, 2020 – September 1, 2020). In other words, the main research goal is to analyse European governments’ initial responses in fighting against COVID-19 from a multidimensional perspective. Since the crisis has clearly amplified socio-economic inequalities across Europe, and the measures related to the two periods are also quite different, another important research objective is to identify a possible East–West division in Europe in relation to the ability of states to cope with this shock.
The paper is structured as follows: the first section offers a contextualisation of the pandemic crisis in Europe during the first wave, by looking closely at its implications until the fall of 2020, as well as offering an overview of governmental responses to mitigating its effects across the EU; the second section goes further in analysing the discrepancies between the East and the West of Europe in the coronavirus context, pointing out their effectiveness in diminishing the adverse consequences (multidimensional approach); the third section emphasizes the importance of good governance for better-coping with the current crisis, drawing both on current literature, as well as on the lessons learnt from the current and previous crises; the last section of the paper offers a normative added value to the current research, as it draws from the conducted analysis specific policy recommendations on how governments should more effectively manage future similar crisis.
Overview of the First Wave of Pandemic Crisis in the European Union
In the context of globalization, characterized by interconnected systems, the current COVID-19 crisis highlights how it has allowed the spread of risks and vulnerabilities across countries, thus “reducing the resilience of key systems to shocks” (OECD, 2020d, p. 1). Subsequently, this health crisis spilled over into the economic sphere, turning into an unprecedented global economic shock. Over the last years, resilience has often been criticised for being merely a “buzzword” in the academia (Béné et al., 2014), a universal solution or the “go to objective/sollution” in all spheres and policies of the EU’s agenda (Korosteleva, 2018). However, the current pandemics has undoubtedly brought back the debates and discussions around coping with this severe crisis, thus bringing resilience back into the spotlight. In this regard, in order to prepare for future shocks, most European governments have adopted a systems’ approach based on resilience (Hainbach, 2020; Hainbach & Redeker, 2020; McKinsey, 2020; OECD, 2020d). Such an approach is not surprising, considering that the economic condition today is clearly defined by uncertainty over: how long restrictions and social distancing will take, how long it will take to get vaccines broadly distributed; or, in general, over the moment when life will get back to normal, if ever. Under these uncertain circumstances, governments and companies alike find it particularly difficult to operate and plan. Only by reducing this uncertainty will governments and companies be able to go forward and start planning more effectively and find the path out of this crisis.
Understanding more about the pandemic and its consequences is challenging and it still looks like we will be learning about COVID-19 for many years to come. Subsequently, despite a consistent surge in research studies about the coronavirus in various fields, its implications remain largely unknown, considering that: the crisis is unprecedented in terms of scale and multifaceted nature (1); the regional and local impact is highly heterogenous at territorial level (2), as well as the fact that the crisis is still unfolding (3).
-
(1)
The crisis is multifaceted, affecting different sectors and spheres from social, economic and political systems which, in turn, pushes policy makers and academia alike to analyse its complexity and find solutions from different fields such as economics, international relations, governance and policy responses. Accordingly, researchers in various domains have focused their interests on studying the effects and overall impacts of the global pandemic, from medical sciences (Harapan et al., 2020; WHO, 2020a), economics (IMF, 2020; OECD, 2020a, b, c), governance and regional development (Krishna & Kummitha, 2020; Mazza & Mavri, 2020), to environment (Cheval et al., 2020), etc.
-
(2)
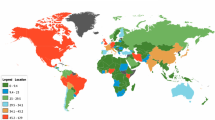
The existing data and forecast provided by the most important international institutions (ECB, 2020; ECDPC, 2020; IMF, 2020; OECD, 2020a) highlight that the first wave’s impact of the global pandemic was highly heterogenous, with a strong territorial dimension. In this regard, the crisis has shown a very different regional and local distribution, being significantly asymmetric within countries (OECD, 2020a), thus pointing out “a spatial dimension that needs to be managed” (McCoy, 2020). Because such responsibility is shared among various levels of government, WHO has emphasized the relevance of effective coordination mechanisms since the outbreak of the coronavirus (WHO, 2020a). Subsequently, national, regional and local bodies are on the frontline in responding to the pandemic, considering that they are first to act and called upon to implement tailored made containment measures, which are to be context and place specific (Batabyal & Beladi, 2022). As such, the social, economic and fiscal constraints have pushed governments to consider large social (including health) and economic relief programs, imposing, in the first half of 2020, stringent lockdown measures. Accordingly, in the European context, the states took necessary measures and actions in order to better contain the spread of the virus, to prevent the collapse of public healthcare systems, as well as to diminish the considerable negative effects on their economies, while reinforcing the responsiveness and efficiency of these systems. Regarding the specific elements that contribute to the differentiated impact of the pandemic, they also differ a lot, from point of entry, to urban/rural, to development gaps, access to healthcare & education, job market and possibility to work remotely, to the structure of the economic sectors (i.e. tourism was more affected than IT).
-
(3)
At present, despite mass-vaccination, countries across the world, including the European states, are still vigilent to potential surges of COVID-19 cases, considering the mutations the virus met over the last years. As such, despite launching mass vaccination campaigns, the fast-spreading variants (like Delta or Omicron) keep governments concerned over potential new waves, despite relaxing most of the existing restrictions.
With respect to easing the restrictions due to COVID-19 crisis, IMF (2020) has presented at length the specific measures and policy responses of different countries. When browsing through the myriad of various responses, it becomes clear that the timing of restrictions’ enforcement and of their easing, as well, has greatly varied, from one country to the other. Han et al. (2020) examined the consequences of easing COVID-19 restrictions in five high-income countries in Asia Pacific and four in Europe, concluding that although the outcome of the pandemic crisis is still uncertain, countries should continue to learn from the experiences they face so as to limit the transmission of the virus and to protect vulnerable groups. Ultimately, it stands to reason that countries strive to make decisions about easing restrictions based on a combination of infection severity/mortality rate and on the multidimensional effects of restrictions (Harris & Brunsdon, 2021).
Given this volatile pandemic context, it is more important than ever to call for collective action, thus reminding the local communities of their vital role to help keep the pandemic under control. In this regard, the local and national institutions, including the representatives of the public health sector, have to constantly motivate people to follow their recommendations, by stressing on their invaluable input to influencing the epidemiological evolution. These aspects are particularly relevant, mainly if considering that the general population grows fatigued of following the recommendations, especially since the second wave; in this context, people are not always aware of the positive benefits of social distancing, wearing masks or other measures that have affected their lifestyle and find it more challenging to keep on following specific restrictions. The EU Member States should continue to implement adequate measures for reducing the risk of transmission. However, should the situation escalate, these measures could be more restrictive and legally binding, so that public institutions may need to close public spaces all together and even enforce quarantine conditions. All these can be adopted at European, national or local levels, depending on the specific context, which induces a thorough assessment of the local situation (place-specific), coupled with a transparent decision-making process which should be openly and directly communicated to the general public. Specifically, for a better management of the public health situation, the designated authorities should reinforce healthcare capacity to cope with potential surges in COVID-19 infections, as well as to make sure that health services do not become overwhelmed. Faster and more accessible testing is vital for detecting infections in the community, for having a comprehensive picture on the evolution of the epidemic and for improving the effectiveness of specific measures such as case isolation and contact tracing. Moreover, national and sub-national institutions should constantly ensure that public health institutions are appropriately equipped with necessary medical supplies, considering the high demand at a global scale; at the same time, protecting vulnerable people and minimising the risk of SARS-CoV-2 transmission is highly relevant.
Is There an East–West Divide in Europe in Terms of Government Responses to the Coronavirus Crisis?
In such times of great uncertainty, governments across the globe try to cope with systemic failure of multi-level governance, from inter-regional, to European, national and local levels, thus pushing them to consider large social (including health) and economic relief programs. It should now be a top priority for policy-makers and academia alike to assess and quantify the effects of these measures as they will help guide the response strategies in other locations. A wide range of control measures have been targeted to mitigate the ongoing infection with SARS-CoV-2. Considering the severity of the next waves that kept hitting all the countries in Europe, the majority of European governments have adopted a series of immediate, restrictive measures to contain the spread of the virus prior to additional policy responses, such as: enforcing general rules of conduct and hygiene, mobility restrictions that have a big potential in effectively delaying local epidemics (Ryu et al., 2020); or further advancing social distancing measures (Fong et al., 2020). In the last years, however, the pandemic context has shown that there is no recipe for best-coping with its adverse effects, but that appropriate measures to mitigate crisis could be drawn on the insights and experience of the countries that have recovered after the surges more swiftly and with fewer causalities, as well as on the lessons learnt from managing and mitigating the negative effects of previous pandemics and global crisis situations.
When it comes to the literature and comparative analyses of the pandemic’ outcome across the world, most studies outline the differences in terms of spread and impact between the West (European states and/or USA) and the Asian countries (specifically the Eastern ones). This comparison among the two regions mainly stemmed from the necessity to cross-compare the efficiency of governmental measures and policy responses between two different systems: the Western democratic model, characterised by multi-level governance and power decentralisation versus the Asian model, which is far more centralised and autocratic. In this regard, Yamamoto and Bauer (2020) conducted a comparative analysis between Central Europe and East Asia of “people infected with SARS-CoV-2” or simply named “COVID-19 cases” and have explored the myriad of factors that made the pandemic crisis more severe in the Western world. The research concluded that Europe is far more affected than Asia due to specific elements, such as major disparities in the closeness of direct human contact (much higher in Europe), marked gap in obesity between Westerners and Asians (more pronounced in the West), but also notable cultural differences (food culture, wearing shoes indoors, normality of wearing masks, indoor-outdoor life clear distinction). There are also several studies that analyze the main discrepancies among European economies in relation to their health systems and how they coped with the crisis (Celi et al., 2020; Tooze & Schularick, 2020; Walker & Smith, 2020; Wiiw, 2020). It should be noted that amid this pandemic, some of these gaps are going to be accentuated, with governments and societies becoming more and more aware of them (Amdaoud et al., 2021; Cabrera-Barona et al., 2018; Himmler et al., 2022; Panteli & Maier, 2021; Tocci, 2020).
From a territorial perspective, due to the increased adoption of smart technologies, cities represent the hubs for both the transmission of pandemics, as well as the most resilient systems to help fight against it. In this context, in terms of combating the pandemic in smart-cities framing, Kummitha (2020, p. 1) outlined that “the techno-driven approach is more productive to identify, isolate and quarantine infected individuals”; although a more strict and technological approach offers a better grasp and control of the crisis to public institutions, it infringes human liberties and rights, as governments’ powers generally present a challenge for democracy.
Despite the fact that it has already been over two years since we have been living with the pandemic, governments are still committed to and concerned about outlining the best measures and responses in order to better cope with and mitigate its various effects. Subsequently, this global health crisis, which came in many waves (and counting) also brought about different national responses implemented by governments. To complement and support their efforts, scholars and research institutes have centered their attention on analysing the effectiveness of various governments’ responses, but also on identifying the main determinants of swift and rapid recoveries. After four waves, with surges and recovery phases, the latest studies of the responses’ effectiveness confirm the impact following the first wave and conclude that the strength of the economy, the promptness of the actions, and the lessons learned from relatively similar past crises are among the most relevant factors influencing the effectiveness of the fight against COVID-19 (Delis et al., 2021; Haug, 2021; Martínez-Córdoba et al., 2021; Wang, 2021). For instance, in evaluating the effectiveness of governments in mitigating the effects of COVID-19, Delis et al. (2021) have identified as particularly important some cultural characteristics such as low power distance and high patience and found that the main drivers of efficiency are the quality of institutions, high public spending in health, and economic equality. Along these lines, Martínez-Córdoba et al. (2021) highlighted that a greater compliance with the rule of law significantly enhance efficiency. After all, as Koyama (2021) suggests, it is a short-term trade-off between public health and freedom; if this trade-off is attempted to be implemented in the long run, it will not work. Apart from these various determinants, some studies (Akroyd et al., 2020; Wang, 2021) also found that the level or urgency in providing responses is key to prepare for post-pandemic recovery, as well as to cope with the negative impacts emerging from the initial response phase and to elaborate long-term reforms. Furthermore, Haug et al. (2021) point out that the effectiveness of individual non-pharmaceutical interventions (NPIs) is heavily influenced by governance, as most previously mentioned studies highlight, but also by the local colours and context.
Overall, the literature (Mobin et al., 2021; Welfens, 2020) clearly underlines that traditional mechanisms are not enough to manage and respond to the unprecedented challenges of global pandemics. In this regard, the governments’ responses should consist in collaborative governance, through ‘whole of government’ and ‘whole of society’ approaches (Akroyd et al., 2020). Although the studies measuring the efficiency of the governments’ responses and frameworks available in the literature are diverse, with many varied results, as OECD (2022) highlights, the more than two years of the pandemics have brought governments to similar conclusions concerning the global health crisis responses’ efficiency, such as: the general preparedness was insufficient; even if governments’ efforts to curb the negative impact of the pandemic on various sectors have been consistent, they should carefully monitor the long-term budgetary costs; and last, but not least, trust requires transparency, achieved through constant effective communication and especially by involving specific stakeholders and the general public in risk-related decision-making.
Although the first wave has hit harder the more developed Western countries, they were more prepared to handle the second wave, having a forward-thinking approach by investing in key strategic sectors at the proper territorial levels, whereas the Eastern states proved to be more vulnerable to this wave of pandemic crisis due to a varied palette of factors which are to be uncovered through the analysis. Subsequently, when it comes to the European states, the literature is lacking in-depth studies that offer a clear comparative analysis between them or an impact analysis to highlight potential patterns, differences and outcomes in terms of policy responses and crisis management. Such cross-comparison is relevant since the crisis induced an unprecedented increased concentration of power in governments’ hands, which is particularly problematic in the young democracies in the East.
As several waves unfolded, with their specific surges and recovery phases, most European countries have come to understand that, despite the accumulated experience in mitigating and coping with the adverse effects of the pandemic crisis, it is still too early to properly assess the impact on economy, society and public health. However, there are some notable traits that could be outlined when it comes to the differences between the Eastern and the Western European countries. In the following sections we will detail the aspects that have created a gap between these two groups of states.
Methodological Approach
The current paper aims to analyse the governmental measures to the COVID-19 pandemic in Europe, in order to identify those types of actions that have enhanced the countries’ ability to better withstand and cope with its severe negative effects. Addressing this crisis should be done in an integrative manner, so that the most relevant answers to the challenges that arise could be found, especially in the deeply affected areas of activity. At the same time, good governance of public health should be the central concern of the authorities (Zhao et al., 2021). Starting from these, our analysis was performed by taking into account two periods: the first period, known as the lockdown (March 1, 2020 – June 1, 2020) and the second period of relaxation with restrictions being lifted (June 1, 2020 – September 1, 2020). Although these two periods are similar in length (3 months), the climate can also play a decisive role in explaining the differences between European countries if we consider that high temperatures do not favor the spread of the virus as much as in the cold season; instead, the second period coincides with the summer holidays, which could mean more channels of virus transmission. However, the measures related to the two periods are diversified, which may underline a possible East–West polarization in this direction. To increase the comparability between the effectiveness of the actions taken by various governments, several countries in Europe, which are not part of the EU (Switzerland, Norway, the United Kingdom, Turkey, Russia, North Macedonia, Montenegro) and the six countries belonging to the EU’s Eastern Partnership (the Eastern neighbors: Armenia, Azerbaijan, Belarus, Georgia, the Republic of Moldova, Ukraine) were added in the research. Considering the latter, it is interesting to see whether there is convergence or similar behavior in the implementation of certain types of measures or, on the contrary, if there is a specificity induced by various factors. In addition, it is relevant to account for the conditions between the historical past, path dependence and the answers offered by countries in the fight against COVID-19. Thus, the variables included in this study were grouped into four multi-dimensional components, covering the medical, socio-economic, institutional and cultural spheres. Based on these factors, an equation in which the latent variable is the capacity to cope with COVID-19 shock was designed which, in the end, will outline a specific hierarchy of the analysed countries in terms of combating COVID-19.
Therefore, mirroring the different economic systems in relation to the indicators considered in our research can help in identifying the gaps in order to outline the most appropriate measures that need to be taken by national governments. In fact, the main purpose was to study the elements likely to be correlated with ensuring a climate conducive to striving the COVID-19 pandemic by European governments, more precisely, to find which of the analysed factors contribute the most to diminishing the adverse effects of this health crisis, determining a higher capacity to cope with it. In order to emphasize this, it is important to bring to the fore the importance of the medical sector and its endowment with adequate resources, both human and material (number of doctors, nurses, hospital beds, etc.), without which, overcoming this global pandemic would be practically impossible. These variables have been incorporated into our approach in the medical factor component.
Regarding the socio-economic aspects, variables that define, as a whole, the quality of life were included. As such, they refer to the physical conditions in which people live, the content and nature of the activities they carry out in terms of the education, goods and services they have access to, the adopted consumption patterns, the lifestyles, all of which are influenced, to a large extent, by the income level (Gini index) and the country’s economic development. A high level of quality of life is usually expressed in terms of coping with possible shocks (from the perspective of our study, the impact of SARS-CoV-2 infection). If people earns enough, they can afford a higher quality goods consumption, which will impact life expectancy; they can have access to better medical services, including online information, and they can overall pay more attention to healthcare. Instead, the unemployed, immigrants or the elderly find it difficult to afford at least one annual medical consultation, to detect possible comorbidities and, consequently, they do not have equal opportunities for high life expectancy.
Beyond this utilitarian approach, based on the level of well-being of the individual, assessed through resources, the value system as well as the cultural environment of the person should be taken into account. In the Eastern European countries, which experienced communism, based on dictatorial regime, the susceptibility to respect the rules imposed by the authorities (at least in the first wave of the pandemic) was greater. However, subsequent developments in the pandemic, including the number of deaths caused by COVID-19 and the vaccination rate, have shown the population of the former communist countries to be more reluctant to complying with government measures to combat the disease, obedience and fear gradually disappearing, to some extent, in the waves that followed. Regarding Western countries, where democracy, free will and the desire for unrestricted manifestations are key elements of the smooth running of daily activities, there it may be more difficult to accept obedience to the restrictions and rules imposed by the authorities for a longer period of time. In addition, a society marked by individualism or masculinity can shape differently the impact of the shock called COVID-19.
Coupled with all these issues, the quality of institutions, defined by government effectiveness, political stability or regulatory quality, can also make the difference between states in finding the best solutions to this health crisis and in providing prompt responses to challenges. Therefore, beyond the medical and socio-economic factors, the components that refer to the institutional arrangements, as well as the cultural aspects could influence the shock resistance of the countries alike.
Given all these, the main working hypotheses are: H1: Medical, socio-economic, institutional and cultural factors influence the dynamics of COVID-19 and create differences in the European space; H2: Government effectiveness shaped the COVID-19 death rate within the European countries in the first wave of the pandemic.
The data necessary for the analysis were collected from official sources, presented in Annex 1, and the statistical programs in which we have performed the analysis were Stata and JASP. All variables were transformed into logarithmic values.
Results and Discussion
As can be seen in Table 1, there are significant differences between Western and Eastern Europe: while the average number of COVID-19 deaths (per 1000 people) was high, at 20.797, in the first period (lockdown) for Western countries, this mean was much lower in the case of the Eastern states (2.253). For the relaxation period, the situation is reversed: in Western countries, this was 3.351, and for Eastern countries 5.069 (higher than in lockdown). Although the number of COVID-19 tests is, potentially, a variable that could have been taken into account, our analysis was mainly based on the COVID-19 deaths because, in the end, what matters for an efficient health system is its ability to save lives.
Based on the indicators included in the analysis, the descriptive statistics for the two groups of states were obtained (Table 2).
Given these different situations, our approach seeks to elucidate which of the medical, economic, institutional and cultural factors have contributed more to strengthening the capacity to cope with the shock and whether the actions of European governments have played a key role in this process. Thus, all variables have been grouped into four components (medical, socio-economic, institutional and cultural), in order to identify the main factors that explain why the COVID-19 pandemic knew various degrees of intensity at European level. In what follows, we underline the conditionalities established between their constituent elements by applying network analysis. The first two factors (medical and socio-economic) are presented in Fig. 1.
The medical factor measures the quality of the healthcare system in terms of resources and performance. High values imply a good quality of the healthcare system (marked in blue). The more intense the blue colour, the stronger the links between the variables that are part of each factor. Conversely, lower values indicate weaker or even inverse correlations between indicators, their representation being made with a red line. The performance of the health system directly and decisively influences the incidence rate of COVID-19. Health spending shows financial allocations by states for health and, therefore, it is assumed that countries with high expenditures also have improved health infrastructure, more medical staff and the ability to perform more tests to detect the coronavirus. The number of hospital beds ultimately refers to the sanitary physical capacity of the state considered to take proper care of its patients: the higher the number of beds, the more likely the country is to have an appropriate infrastructure with a direct impact on the treatment of COVID-19 patients. The number of physicians and nurses shows the human capacity of the health system in a country, this designating an important barometer to deal with health challenges: the higher their number, the lower the COVID-19 death rate. Many European countries have faced a shortage of places in intensive care units, as well as a crisis of physicians and nurses (Italy, France, Spain, etc.). In contrast, during the first wave of coronavirus, Germany was considered an example of good practice in the health system, with a high capacity to provide intensive care to COVID-19 patients (8.3 beds per 1000 inhabitants), compared to Italy, which has 3.4 beds per 1000 inhabitants, according to WHO, receiving patients from other countries – mainly from France. Medical examinations and treatment are among the most relevant aspects of health care but, in the absence of comprehensive health care costs, people have to bear their cost, which is a major problem for many Eastern European states if we were to refer to income level. Most unmet needs could be related to the price of care, the relatively long distance to a health center, long waiting lists, etc. In addition, with the outbreak of the COVID-19 pandemic, these problems have intensified amid fears among a large part of the population about the possibility of contracting the virus in hospitals. This situation was especially encountered among patients diagnosed with chronic diseases, those who required certain surgeries, but also among those who had symptoms related to the SARS-CoV-2 virus, and for many of whom home care has had adverse consequences (e.g., worsening chronic diseases or even a significant increase in mortality rates). Referring to life expectancy, this influences the incidence of COVID-19 because, in over 75% of cases, the disease occurs in people over 65 years of age; in this sense, countries with high life expectancy populations also had high mortality rates (Italy, Spain, the Netherlands). In a high-performance medical system, the appropriate treatment of the sick is carried out, diseases are eradicated and, implicitly, the life of the population is prolonged.
As for the socio-economic factor, this designates, in essence, the quality of life in a country. Although not a universally valid rule, GDP per capita can be a direct and positive influence for European states on COVID-19 disease: the higher a country’s GDP per capita, the greater its resources and the more it can intervene in better dealing with shocks. However, the following situation should also be noted: the more prosperous a country is, the more intense economic activities and human capital concentration, which can contribute to the spread of the virus more easily. Another constituent element of the socio-economic factor refers to digitalization. Lack of internet access and digital skills, as well as not owning a mobile phone, are factors that can be associated with effects such as reduced contact with physicians, medical history and profile information, and lower chances of acting in a timely manner in case of a health problem. Europe operates below its digital potential, according to the Digital Economy and Society Index (DESI), and it is for this reason that governments should support actions for a good management of the transition to digitization, access to capital and opening up data flows. The size of digital public services consists of several variables, some of which refer strictly to the medical component: the percentage of people who have used online health and care services without having to go to a hospital (the indicator of e-health services); the extent to which general practitioners use electronic networks to exchange medical data with other medical and professional service providers (the indicator of medical data exchange); and the extent to which practitioners use electronic networks to transfer prescriptions to pharmacists (electronic prescription indicator). Electronic services reduce transaction costs and, in the context of the current pandemic, prove to be all the more useful by encouraging people to use them. It should be noted that in some chapters of the digital economy, the countries of Central and Eastern Europe (“digital challengers”) are convergent with Old Europe (“digital front-runners”), some of them, such as Estonia, have a percentage of digital public services over 90%, being included in the category of digital front-runners. For example, in the case of households with internet access, the difference is of only four years between the two parts of Europe (East and West), and in the case of households with different access to the network, it is the same. This shows that there is no significant gap between European states from the point of view of digital infrastructure. However, a deeper analysis of DESI indicates differences between European states in terms of connectivity, digital skills, internet use, integration into digital technology and public digital services. In strong connection with digitalization, the main prerequisite to make governments more resilient in the face of potential future crises is their ability to take full advantage of technology and really deliver on contactless governance (McKinsey, 2020; Cheval et al., 2020), not only putting government services online, but also involving citizens in the online sphere. Thus, large-scale digitization can be a way to respond efficiently to possible further health shocks, by conducting online daily actions, work-related tasks, the relationship with public administration, as well as activities in the medical and educational sectors. Such digital activities allow a significant reduction in exposure and limit the spread of the coronavirus.
The integration of the “unemployment” indicator in the study highlights the number of people looking for a job and we considered that, for people who do not have a stable job, the financial situation is serious, being prone to COVID-19 infection. In the absence of proper income, the unemployed will tend to take more risks for employment and will not comply with the social distance measures imposed. Closely related to this, the Gini ratio shows the degree of inequity in a society, and the higher the value of the indicator for a country, the greater the inequities. However, the pronounced inequalities between the members of the society also influence COVID-19 incidence in the sense that disadvantaged people are more exposed to the risk of disease. Beyond these variables, population density as well as the migration phenomenon can shape COVID-19 transmission speed.
The literature (Briggs et al., 2021; Clark et al., 2021; Martinez-Bravo & Sanz, 2021) emphasizes that this pandemic has induced a series of blockages in the economy and social damage, including mental health problems, unemployment, domestic violence, accentuation of inequalities and, among vulnerable groups, isolation has led to even greater losses. The lack of jobs and the impossibility of having access to subsistence resources practically meant deepening the gap between the rich and the poor. The economic costs resulting from the adoption of different coronavirus strategies have varied from country to country, depending on the number of cases recorded. Intensive care units have a limited number of beds, ventilators, these facilities being, as a rule, lower in developing countries, a situation that hinders the quality of SARS-CoV-2 virus control (Caparrós & Finus, 2020).
In addition to the two components exposed, we considered it appropriate to include institutional and cultural factors in the analysis as well (Fig. 2). The institutional capacity of governments (reflected in government effectiveness, political stability and regulatory quality) could be a determining factor for overcoming, in good conditions, the difficult situation caused by COVID-19, in the sense that the more efficient governments are and the faster they take strict measures, the lower the multiplication rate of COVID-19. The cultural factors associated with individualism could also play a role in the COVID-19 trasmission: the more individualistic a population, the more singular and disparate its actions will be, while in the case of a collectivist-thinking population, the measures are ordered by the State and adopted quickly by the population. In shaping the efficiency of governance systems, a significant contribution is given by trust in public institutions, which is gained over time, based on values, principles and norms that are respected at all levels of society, including when they are under threat and pressure from interest groups. When it comes to health systems, gaining interpersonal and institutional trust, especially in times of crisis, means, in particular, ensuring the optimal functioning of the flow of services offered, the increased credibility of the profile entities and also the establishment of an interface in the relations of national governments with their citizens. This last aspect refers to the constant cooperation that would be required between the bodies working in the field of health and governments which, as it was found during this health crisis, have the responsibility to inform the public, on a large scale, about the policies that need to be applied in the context of the occurrence and application of COVID-19 vaccines. With regard to the way in which informal institutions shape the receptivity to the messages of the authorities in the fight against COVID-19, it was noted that culture plays a crucial role (Airhihenbuwa et al., 2020; Colleoni et al., 2022). Belonging to certain values influences the behavior of individuals, including the degree of acceptance of government measures for combating COVID-19 and, for this reason, the ex-communist regime can be cited as a cause of disparities created between Eastern and Western Europe.
Culture, through its values in each state and people’s perceptions of measures to combat COVID-19, can influence the epidemiological evolution. Thus, it also matters in the context of vaccines’ administration which, thanks to the scientific communities, governments and pharmaceutical companies, were distributed, at the end of 2020, in order to provide high protection against disease and virus infections. Although the vaccination campaign has started and is ongoing throughout Europe and the world, the uncertainties and worries about the future continue to dominate the debates and discussions (Bertelsman Shiftung, 2021). Nevertheless, with several versions of the vaccine on the market, the crisis is far from being over. In this regard, the impact cannot be properly assessed as the crisis is still unfolding; however, given the diversity of measures and vulnerabilities among the countries and regions of Europe, it is highly expected that, once the crisis is over, the economic and social divergence become much greater (Hainbach & Redeker, 2020; Sapir, 2020). However, perceptions on vaccination, which is essentially the only way to eliminate the pandemic, are very varied at international and European level, with cultural issues having strong influences on its acceptance. According to Lazarus et al. (2021), who applied a survey in 19 countries worldwide (N = 13.426 people), it is found that 71.5% of respondents said that they would be very likely to use a COVID-19 vaccine, while 48.1% reported that they would accept it only if employers recommended them to do so. Then, while the acceptance rate reaches around 90% in China, the percentage is around 55% in Russia. The research also emphasizes that there is an association between the degree of trust in the information obtained from government sources and the acceptance of vaccination, both on their own initiative and on the advice of the employer. In addition, a Eurofound study (2021) regarding the intention to vaccinate concluded that there is hesitation in the application of the COVID-19 vaccine, with a gender difference (29% men and 25% women), this being linked with a weaker trust in the authorities and the government. Another research at EU27 level (Ahrendt et al., 2021) was applied online, in three stages, from April 2020 to March 2021, as follows: stage 9 April – 1 May 2020, related to the lockdown (N = 63.354); stage 22 June – 27 July 2020, when there was a gradual elimination of restrictions (N = 24.123); stage 15 February – 30 March 2021, correlated with the start of vaccination programs (N = 46.800). In close conection with the topic addressed in this paper, it is interesting to highlight, briefly, the perceptions of respondents regarding vaccination. Therefore, it was showed that there is an East–West polarization: there are countries with higher rates of people that declared their intention to vaccinate, over 70% (Denmark, Ireland, Malta, Portugal, Finland), below 50% (Bulgaria, Slovenia, France), while the EU average was 64%. What is more, there are other differences, such as between the rural and urban population, the former being more reluctant when it comes to vaccination (31% would not agree to vaccination), compared to people in urban areas (22%). Also, those who mostly use social media to get information are skeptical about getting vaccinated (40%), while those that use press, television or radio are reluctant to vaccinate up to 18%. This is why channels play an important role, especially when it comes to credible information.
Cumulating all four factors, we find that the highest conditionality exists between the medical and the socio-economic component: 0.79, on a scale from 0 to 1, where 1 denotes the perfect relation (Fig. 3). The infrastructure and human resources from hospitals are dependent on the macroeconomic climate of a country and are less influenced by institutional and cultural aspects. Institutional arrangements, on the other hand, are important for ensuring favourable premises for economic development and, for this reason, there is a 30% determinism between the socio-economic and the institutional components.
If we were to refer to the two periods included in the analysis (lockdown vs. post-lockdown), the situation in Eastern and Western Europe is presented in Table 3.
There are major differences between the two regions under analysis, East and West. For the government effectiveness indicator, the values for the East are negative and for the West, positive, while the political stability indicator shows negative values for both regions, for the two periods. At the same time, Table 4 shows the proportions by which each variable contributes to the COVID-19 death rate. As can be seen, there are gaps between institutional arrangements. Thus, for the East, during the lockdown, government effectiveness had a value of 0.933, so that during the relaxation period it droped to 0.804. The evolution of government effectiveness influence is reversed in the West: it started in the lockdown period from 0.824 and then rose to 0.841 (a value that was anyway higher than the value for Eastern countries). For regulatory quality, in the East, the initial contribution was 0.831, and then it decreased to 0.769. In the West, the indicator’s value was higher, over 0.86 in both periods. The political stability indicator shows significantly different values for the two regions: for the East, over 0.80 and, for the West, over 0.59.
In addition to the above, Annex 2 presents the principal components analysis, which highlights the number of factors for decomposition on the eigenvalue, the proportions of indicators in terms of explanatory of variances being captured. At the same time, in Annex 3, the confirmatory factor analysis is applied. Our preliminary research showed the main drivers for the incidence of COVID-19 in the analysed states, with the specification that these factors are at macro level. Being macro factors and not registering a high variation in time, the response to the COVID-19 crisis presupposes concrete actions of the governments taken on the short term. However, government interventions can explain the strong differences between countries, especially concerning the rapid implementation of public health policies. The European hierarchy in connection with the government effectiveness and COVID-19 deaths in the East and West of Europe for the two periods (lockdown and relaxation period) is outlined in Fig. 4.
The pressure on the medical system has meant that the number of deaths in Belgium between March 9 and May 17, 2020 was 37% higher than the average, which means about 8.100 deaths in addition to the usual level. Belgium, a country with a significant mortality rate due to COVID-19, has been the subject of a research (Decoster et al., 2021) before and during the first wave of the pandemic and the main conclusion of the study was that in March – May 2020, the excess of mortality is found especially among those aged 65 and over and with lower incomes. Here, there were different measures from one region to another, in the period after the total lockdown. As such, in the fall of 2020, this country ranked second in the world in terms of COVID-19 death rate relative to the population, after the small state of San Marino. The same problems were encountered in other states such as Spain, Italy, the United Kingdom, France, the Netherlands, Ireland. The situation in the Lombardy region of Italy was also resounding as in March 2020, it recorded between 10 and 18.500 more deaths than the 2015–2019 average (Depalo, 2021).
Regarding the Eastern European countries, they have managed the outbreak in spring 2020 quite well, considering that governments had a month in advance to prepare (the first cases of COVID-19 infection appeared in the West) and take the necessary precautions and restrictive measures to better contain the virus, coupled with the experience and know-how provided by the EU countries that were first affected (such as Italy or Spain). Subsequently, the total death rates in the Eastern bloc have been far lower than in larger, richer Western countries (Adam, 2022), which may seem surprising considering that, on the one hand, health systems and infrastructures are more underfunded, understaffed and, overall, less prepared for coping with pandemic situations and, on the other hand, Eastern governments have less capacity to design and implement public policies. However, there are explanations which can be found in the channels of transmissions of infectious diseases: international trade, tourist flows, foreign students, migration and transport, all these being more pronounced in developed countries. Due to COVID-19, most nations imposed restrictions or even banned social and economic gatherings and also international trade. In the first phase of the pandemic, many countries had problems regarding equipment supply, including the medical one, from China, which made them focus more on locally produced necessary goods which meant an additional loss for the countries that did not have enough resources.
A study analyzing a sample of 138 countries between March 24 and April 21, 2020 (Antonietti et al., 2021) points out that both the diffusion rate and the COVID-19 death rate are higher in countries with higher GDP/capita levels because world trade, human flows and international openness facilitate the spread of the virus; on the other hand, those countries that have better medical infrastructure have a decrease in mortality. Another research (Bretschger et al., 2020), applied on OECD countries, associates other factors with high numbers of cases of SARS-CoV-2 infection and mortality, such as pollution, obesity, and herd immunity. In the initial phase of the pandemic, the countries that experienced the first infections with this virus experienced significantly higher mortality rates, which resulted from the lack of information on the evolution of the coronavirus and expertise in the proper management of such a situation. In addition, the unprepared takeover of the European medical system has meant an insufficient capacity to meet the existing needs. In any case, the first wave was perhaps the most devastating, both in terms of the unpredictability of coronavirus evolution and of socio-economic uncertainty.
Nevertheless, the next waves hit all countries at the same time and governments across the EU found it extremely difficult to reintroduce restrictions after months of relaxation. Despite their initial success, the current situation in Eastern Europe outlines their governments’ unsuccess to provide economic support to their populations, especially to vulnerable individuals and firms. Compared to Western Europe, that offers furlough schemes and universal benefits to the population and economic sectors affected by the crisis, the Eastern governments failed to provide similar support. Across Europe, the general public no longer supports restrictive measures. Since in the Eastern part of the continent the majority of governments are led by populists, they are particularly sensitive to negative public opinion, which will put additional pressure on adopting austere measures, rising the dangers of social unrest.
Taking into account the four multi-dimensional components of our analysis, the capacity of the European countries to cope with the COVID-19 shock is emphasized in Fig. 5.
It is observed, therefore, that Luxembourg, Switzerland, Norway, Ireland, Iceland, and Denmark register values over 0.5. These states have realized the importance of vital issues in the fight against the COVID-19 pandemic. In these times of health crisis, although it seems that the role of public authorities has diminished, the opposite phenomenon is manifested: they are at the center of the decision-making system, exercising a strong coordination between different stakeholders, transparency and trust being two key issues in this direction (OECD, 2020e). Thus, the main mission of public authorities in these moments is to ensure good governance and communication between various actors, the ultimate goal being the optimal overcoming of the health crisis by all participants.
In the following section, some of the actions taken by European governments and the lessons learned from the first wave of the COVID-19 pandemic will be highlighted.
Lessons Learnt in order to Cope more Effectively with Future Shocks
From the experience of what we have witnessed so far in Europe regarding the COVID-19 pandemic, public health strategies should be continuously adapted to the epidemiological situation in each state. The ongoing health crisis gives us some of the toughest lessons in human history, which calls for adapting social and cultural life to the new normality, by wearing a mask, keeping social distance, washing and disinfecting hands (Basher & Haque, 2021). Although these measures should be strongly supported by governments and citizens, from an economic point of view, a total lockdown for a longer period of time would affect economic activities. On the other hand, in the context of high mortality rates as a result of large-scale relaxation in Europe, significant negative effects on growth could be generated (König & Winkler, 2021).
European policies in terms of response to the COVID-19 pandemic have ranged from the cancellation of public events and closure of schools to total lockdown. Countries with stronger democracies, especially those with high government efficiency, characterized by sound public services and coherent strategies, resorted to such drastic measures later and for shorter periods of time, the population not being open to their acceptance, probably as a consequence of the historical past which did not provide them with similar restrictive experiences. Instead, oppressive political regimes have instilled in society fears and obedience to central power, which explains, to some extent, the vision toward such directives. In addition, countries with a higher level of trust in health services may have slower acceptability responses among their citizens, based on the positive results generated over time by their efficient medical system, this referring, inter alia, to the treatment of patients in optimal conditions. On the contrary, in the case of states where trust in health institutions is low, there is a tendency to try to avoid hospitalization as much as possible, so as not to risk aggravation of the situation by contact with other possible bacteria, nasocomial infections, etc. Furthermore, indicators such as low number of beds, lack of resources, insufficient medical staff can significantly shape human behavior, implicitly the decision to comply more strictly with government measures. At the EU level, in the first wave of the pandemic, countries with relatively lower government efficiency, freedom and societal trust, acted more quickly, unlike better-functioning states. However, this statement should not be generalized, as the SARS-CoV-2 infection had different intensities, with the first outbreaks in Europe recorded in the South and West of the continent, which allowed the East a period of reaction and finding action plans against this virus.
In a severe crisis situation, lockdowns, mass testing for both symptomatic and asymptomatic individuals, as well as vaccinations, are key elements of an effective health policy (Gries & Welfens, 2021). Considering health as a public good (Lucchese & Pianta, 2020), all countries should make consistent efforts to provide equal access for citizens to basic health services, and the international community should demonstrate maximum solidarity in these critical times. In addition, constant cooperation at all levels of society can be a step forward in controlling the epidemiological evolution of SARS-CoV-2, along with ensuring decision-making transparency and removing false news about coronavirus. Although EU policies are in line with the context created by this pandemic, it is up to national and local authorities to better identify internal particularities and act accordingly. Good governance can generate the premises for a proper management of the pandemic, the post-shock effects being felt depending on government effectiveness. Considering that we are facing a health crisis, with unpredictable evolutions of the virus, which can even worsen the situation by the emergence of more serious strains, governments need to work on strategies for pessimistic scenarios to avoid escalating blockages in the medical system. In this direction, the vision of international medical organizations (e.g., the WHO) which provides relevant information on the epidemiological evolution of SARS-CoV-2, which allow the shaping of control measures, should not be neglected.
The dynamics of the spread of the virus should be constantly in the attention of specialists in the development of policies to fight COVID-19, and the monitoring and evaluation of the effectiveness of the implemented measures should be done in due time, so as not to cause even greater problems in the health systems (Bonacini et al., 2021). In combating any shock, the ability to anticipate its occurrence has a special relevance. Thus, if governments do not come with anticipatory measures to prevent possible large-scale disasters in the future, the post-shock action will mean much higher losses. Similarly, in the case of health crises, the capacity to take action before them would result in greater resilience.
Governments should continue to elaborate measures and strategies that revolve around rethinking health and education systems in particular, by continuing the path of accelerated digitalization. To better deal with the epidemic, governments should focus their energy and resources on medical staff training/online sessions to discuss protocols and situations encountered in different hospitals, acquiring the necessary hospital equipment, government spending on health, information campaigns, transparency of the medical system, more involvement of state institutions in handling the health crisis, and having a more coherent strategic vision.
Overall, governments should concentrate their efforts on ensuring that all citizens have access to basic public services, focusing on the formulation and implementation of articulated and transparent policies, independent of political pressures, so that regulations be qualitative and non-discriminatory. Referring to public authorities, they should, firstly, prepare a communication mechanism with the citizens in order to overcome informational asymmetry; secondly, public authorities have the role to ensure cooperation with the other factors involved: experts in the field of health, physicians, supply companies, civil servants, private companies, volunteers and, in some cases, even the external environment, for improving the decision-making process, identifying problems, assessing risks and taking appropriate decisions.
Conclusions
The corona-pandemic has led to the largest global recession since World War II, with the EU as a whole experiencing significant losses, South European countries being among the hardest hit by the crisis in the first wave (Claeys et al., 2021). Since the onset of this health crisis, there have been many facets of this unprecedented global challenge with different responses from governments, depending on the degree of spread of the virus. Having to face increasing numbers of deaths, governments have opted for special measures, such as quarantine, social distancing and, in extreme cases, closure of schools, companies, going as far as total lockdown.
In Europe, the governmental responses highlighted a West–East divide, with differences between the lockdown period and relaxation period during the first wave of the pandemic. Based on the results obtained in our research, the possible factors for the existing cleavage between East and West regarding the COVID-19 death rate could be the following: a lower standard of living (this necessarily leads to a series of deficiencies, which could include fewer possibilities for holidays abroad and a lower mobility of the population, in general); the communist autocratic legacy (in the case of Eastern countries, this eminently autocratic legacy made it easier to bear and without much resistance from the population, which was already common, the imposition of draconian measures of isolation and social distancing – these would have been very difficult to be applied in countries with a strong democracy and which often criticize the arbitrary actions of the authorities); rapid adoption of social distance measures: while in Western countries the average time of imposition of measures was 26 days, in the East, the average time was 8 days; respect for the authorities; lower share of the older population; lower rate of immigrants, etc. In general, while cultural factors are more difficult to change over a short period of time, the macroeconomic climate and the medical factors can be shaped through institutions. The research shows that socio-demographic factors are important in explaining the different incidence rates of COVID-19 in European countries. Overall, medical, socio-economic, and institutional factors influence the dynamics of COVID-19 and create differences in the European space, the first hypothesis (H1) being confirmed.
The governmental capacity to respond to all issues related to this health crisis has proved to be effective to some extent in several states, while in others, the strategic vision has been doomed to failure, the governance systems proving their fragility. The vulnerabilities accumulated over the decades have essentially meant either indolence of some governments in terms of investments in health systems or human capital, or non-consideration of this sector as a major priority. The government effectiveness, even if it can strongly contribute to the development trajectory of a state, in the case of its association with COVID-19 death rate it is found that it can shape this indicator but not significantly, other medical or economic factors influencing it more (age: population over 65, life expectancy, income inequality, etc.), thus partially confirming the second hypothesis (H2).
In order to resist to such a shock, an integrative effort is needed from the side of decision-making actors, based on the smart planning of the actions to be undertaken, so as to ensure a strong resilience capacity of countries, in a sustainable way, for coping more effectively with future shocks. The previous negative experiences, as for instance, SARS crisis in 2002/2003, H1N1 flu virus in 2009, should have been important lessons for resetting the European governance systems, by applying transformative policies by taking into account the resources-needs relationship.
When examining the connection between governance and a crisis such as the COVID-19 pandemic, there is no need to start from the premise that there is a globally agreed institutional model able to respond adequately to this, but there are only certain ways of efficiently combining the functions of institutions according to countries’ specificities, so that the final outcome would result in fewer damages. Consequently, policies should be designed in a place-based sensitivity approach, either on the basis of already existing institutions, if they have proved their usefulness, or by resorting to their replacement through adequate changes of their functions, thus transforming and making them stronger to better withstand shocks. In this regard, governments can propose and implement sound policies by intentionally preparing for managing a shock, provided that the weaknesses of the system have been thoroughly analysed beforehand.
This health crisis has contracted the European economy and the EU has come to its aid through the Next Generation EU program, which gives Member States the opportunity to recover and strengthen their resilience capacity through the implementation of projects designed to ensure greater resistance to future shocks in key areas (Gentiloni, 2020). Along with these, by optimizing the resources-needs balance in the healthcare systems, it is necessary to anticipate future challenges so that states are prepared to respond to them, by minimizing the adverse effects as much as possible.
Last, but not least, the scenario of mass vaccination in all countries of the world could create the premises for moving forward and improving the current situation, thus unblocking economic activities. Despite all the challenges brought about by the COVID-19 shock, the large-scale vaccination still remains the best solution for overcoming the current crisis.
In a future study, we intend to extend the analysis by taking into account the following waves of the COVID-19 pandemic, which would allow clearer evidence of its multidimensional effects in Europe, an aspect that could not be covered in detail in this research, the data being at an early stage. At the same time, more variables such as contagious rates, tests, vaccination and recovery rates will be considered.
References
Adam, D. (2022). The pandemic’s true death toll: Millions more than official counts. Nature, 601, 312–315. https://doi.org/10.1038/d41586-022-00104-8
Ahrendt, D., Mascherini, M., Nivakoski, S., & Sándo, E. (2021). Living, working and COVID-19 (update April 2021): Mental health and trust decline across EU as pandemic enters another year. Eurofound & Publications Office of the European Union.
Airhihenbuwa, C. O., Iwelunmor, J., Munodawafa, D., Ford, C. L., Oni, T., Agyemang, C., Mota, C., Ikuomola, O. B., Simbayi, L., Fallah, M. P., Qian, Z., Makinwa, B., Niang, C., & Okosun, I. (2020). Culture matters in communicating the global response to COVID-19. Preventing Chronic Disease, 17, E60. https://doi.org/10.5888/pcd17.200245
Akroyd, S., Harrington, P., & Nastase, A. (2020). COVID-19 rapid literature review: governance and state capability. Oxford Policy Management, retrieved from: https://www.opml.co.uk/files/Publications/A2241-maintains/maintains-covid19-governance-and-state-capability-rapid-lit-review-final-1-.pdf?noredirect=1.
Ali, I., & Alharbi, O. M. (2020). COVID-19: Disease, management, treatment, and social impact. The Science of the Total Environment, 728, 138861. https://doi.org/10.1016/j.scitotenv.2020.138861
Amdaoud, M., Arcuri, G., & Levratto, N. (2021). Are regions equal in adversity? A spatial analysis of spread and dynamics of COVID-19 in Europe. The European Journal of Health Economics, 22, 629–642. https://doi.org/10.1007/s10198-021-01280-6
Antonietti, R., Falbo, P., & Fontini, F. (2021). The wealth of nations and the first wave of COVID-19 diffusion. Italian Economic Journal, 1-23. https://doi.org/10.1007/s40797-021-00174-z
Arnold, C. (2018). Pandemic 1918: Eyewitness accounts from the greatest medical Holocaust in modern history. St. Martin’s Griffin & Macmillan Publishers Ltd.
Barry, M. J. (2005). The great influenza: The epic story of the deadliest plague in history. Penguin Books.
Basher, S. A., & Haque, A. K. E. (2021). Public policy lessons from the COVID-19 outbreak: How to deal with it in the post-pandemic world? Journal of Social and Economic Development., 23, 234–247. https://doi.org/10.1007/s40847-020-00118-w
Batabyal, A. A., & Beladi, H. (2022). Health interventions in a poor region and resilience in the presence of a pandemic. Applied Spatial Analysis and Policy. 1-17. https://doi.org/10.1007/s12061-022-09440-8
Béné, C., Newsham, A., Davies, M., Ulrichs, M., & Godfrey-Wood, R. (2014). Review article: Resilience, poverty and development. International Development, 26(5), 598–623. https://doi.org/10.1002/jid.2992
Bertelsman Shiftung. (2021). Major differences in the conditions for successful COVID-19 crisis management, retrieved from: https://www.bertelsmann-stiftung.de/en/publications/publication/did/major-differences-in-the-conditions-for-successful-COVID-19-crisis-management-all.
Bonacini, L., Gallo, G., & Patriarca, F. (2021). Identifying policy challenges of COVID-19 in hardly reliable data and judging the success of lockdown measures. Journal of Population Economics, 34, 275–301. https://doi.org/10.1007/s00148-020-00799-x
Bretschger, L., Grieg, E., Welfens, P. J. J., & Xiong, T. (2020). COVID-19 infections and fatalities developments: Empirical evidence for OECD countries and newly industrialized economies. International Economics and Economic Policy, 17, 801–847. https://doi.org/10.1007/s10368-020-00487-x
Briggs, D., Telford, L., Lloyd, A., Ellis, A., & Kotzé, J. (2021), Lockdown. Social Harm in the COVID-19 era. Springer Nature Switzerland: Palgrave Macmillan – Cham. https://doi.org/10.1007/978-3-030-88825-1
Cabrera-Barona, P., Blaschke, T., & Gaona, G. (2018). Deprivation, healthcare accessibility and satisfaction: Geographical context and scale implications. Applied Spatial Analysis and Policy., 11, 313–332. https://doi.org/10.1007/s12061-017-9221-y
Caparrós, A., & Finus, M. (2020). The Corona-pandemic: A game-theoretic perspective on regional and global governance. Environmental and Resource Economics, 76(4), 913–927. https://doi.org/10.1007/s10640-020-00475-4
Celi, G., Guarascio, D., & Simonazzi, A. (2020). A fragile and divided European Union meets COVID-19: Further disintegration or ‘Hamiltonian moment’? Journal of Industrial and Business Economics, 47(3), 411–424. https://doi.org/10.1007/s40812-020-00165-8
Cheval, S., Adamescu, C. M., Georgiadis, T., Herrnegger, M., Piticar, A., & Legates, D. R. (2020). Observed and potential impacts of the COVID-19 pandemic on the environment. International Journal of Environmental Research and Public Health, 17(11), 4140. https://doi.org/10.3390/ijerph17114140 1-25.
Claeys, G., Darvas, Z., Demertzis, M., & Wolff, B. G. (2021). The great COVID-19 divergence: Managing a sustainable and equitable recovery in the EU. Intereconomics, 56, 211–219. https://doi.org/10.1007/s10272-021-0983-8
Clark, A. E., D’Ambrosio, C., & Lepinteur, A. (2021). The fall in income inequality during COVID-19 in four European countries. Journal of Economic Inequality, 19, 489–507. https://doi.org/10.1007/s10888-021-09499-2
Colleoni, E., Romenti, S., Valentini, C., Badham, M., Choi, S. I., Kim, S., & Jin, Y. (2022). Does culture matter? Measuring cross-country perceptions of CSR communication campaigns about COVID-19. Sustainability, 14, 889. https://doi.org/10.3390/su14020889
Decoster, A., Minten, T., & Spinnewijn, J. (2021). The income gradient in mortality during the COVID-19 crisis: Evidence from Belgium. The Journal of Economic Inequality, 19, 551–570. https://doi.org/10.1007/s10888-021-09505-7
Delis, M., Iosifidi, M., & Tasiou, M. (2021). Efficiency of government policy during the COVID-19 pandemic. MPRA. Paper No. 107292, retrieved from: https://mpra.ub.uni-muenchen.de/107292/1/MPRA_paper_107292.pdf.
Depalo, D. (2021). True COVID-19 mortality rates from administrative data. Journal of Population Economics, 34(1), 253–274. https://doi.org/10.1007/s00148-020-00801-6
ECB (2020). Forecasting the Covid-19 recession and recovery: lessons from the financial crisis, ECB Working Papers Series. September 2020, retrieved from: https://www.ecb.europa.eu/pub/pdf/scpwps/ecb.wp2468~068eec9e3e.en.pdf?d8cce11983462f445460c1608083ef4a.
ECDPC. (2020). European Centre for Disease Prevention and Control, retrieved from: https://www.ecdc.europa.eu/en.
Eurofound. (2021). Over a quarter of adults in EU indicate they are unlikely to take COVID-19 vaccine, retrived from https://www.mynewsdesk.com/eurofound/news/over-a-quarter-of-adults-in-eu-indicate-they-are-unlikely-to-take-covid-19-vaccine-427227.
Eurostat. (2020). Economy and finance - GDP and main components, retrieved from: https://ec.europa.eu/eurostat/databrowser/view/NAMQ_10_GDP__custom_77309/bookmark/table?lang=en&bookmarkId=b74febcd-e664-4f22-9c93-2ef510fe371f.
Fong, M. W., Gao, H., Wong, J. Y., Xiao, J., Shiu, E. Y. C., & Ryu, S. (2020). Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-social distancing measures. Emerging Infectious Diseases, 26(5), 976–984. https://doi.org/10.3201/eid2605.190995
Gentiloni, P. (2020). The EU’s pandemic response: Tackling COVID-19, building the future. Intereconomics, 55, 342–343. https://doi.org/10.1007/s10272-020-0926-9
Gries, T., & Welfens, P. J. J. (2021). Testing as an approach to control the Corona epidemic dynamics and avoid lockdowns. International Economics and Economic Policy, 18, 1–24. https://doi.org/10.1007/s10368-021-00495-5
Gualde, N. (2016). Les épidémies racontées par la littérature (The epidemics told by the literature). L’Harmattan.
Hainbach, N. (2020). Europe’s future – policy brief: how resilient are European countries and regions?, Bertelsmann Stiftung, retrieved from: https://www.bertelsmannstiftung.de/fileadmin/files/BSt/Publikationen/GrauePublikationen/200727_Corona_resilience_Policy_Brief_FINAL.pdf.
Hainbach, N., & Redeker, N. (2020). Flattening the recession curve-comparing initial fiscal responses to the Corona crisis across the EU, Policy Paper for Hertie School and Jacques Delors Centre, and Bertelsmann Foundation, retrieved from: http://aei.pitt.edu/102701/1/20200409_Flattening_the_Curve_Redeker_Hainbach.pdf.
Han, E., Tan, M. M. J., Turk, E., Sridhar, D., Leung, G. M., Shibuya, K., Asgari, N., Oh, J., García-Basteiro, A. L., Hanefeld, J., Cook, A. R., Hsu, L. Y., Teo, Y. Y., Heymann, D., Clark, H., McKee, M., & Legido-Quigley, H. (2020). Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet, 396(10261), 1525–1534. https://doi.org/10.1016/S0140-6736(20)32007-9
Harapan, H., Itoh, N., Yufika, A., Winardi, W., Keam, K., Te, H., Megawati, D., Hayati, Z., Wagner, A. L., & Mudatsir, M. (2020). Coronavirus disease 2019 (COVID-19): A literature review. Journal of Infection and Public Health, 13(5), 667–673. https://doi.org/10.1016/j.jiph.2020.03.019
Harris, R., & Brunsdon, C. (2021). Measuring the exposure of Black, Asian and other ethnic groups to COVID-infected neighbourhoods in English towns and cities. Applied Spatial Analysis and Policy. 1-26. https://doi.org/10.1007/s12061-021-09400-8
Haug, N., Geyrhofer, L., Londei, A., Dervic, E., Desvars-Larrive, A., Loreto, V., Pinior, B., Thurner, S., & Klimek, P. (2021). Ranking the effectiveness of worldwide COVID-19 government interventions. Nature Human Behaviour, 4, 1303–1312. https://doi.org/10.1038/s41562-020-01009-0
Himmler, S., van Exel, J., & Brouwer, W. (2022). Did the COVID-19 pandemic change the willingness to pay for an early warning system for infectious diseases in Europe? The European Journal of Health Economics, 23, 81–94. https://doi.org/10.1007/s10198-021-01353-6
IMF. (2020). World economic outlook. A long and difficult ascent, retrieved from: https://www.imf.org/en/Publications/WEO/Issues/2020/09/30/world-economic-outlook-october-2020.
König, M., & Winkler, A. (2021). COVID-19: Lockdowns, fatality rates and GDP growth. Evidence for the first three quarters of 2020. Intereconomics, 56, 32–39. https://doi.org/10.1007/s10272-021-0948-y
Korosteleva, E. (2018). Paradigmatic or critical? Resilience as a new turn in EU governance for the neighbourhood. Journal of International Relations and Development, 23, 682–700. https://doi.org/10.1057/s41268-018-0155-z
Koyama, M. (2021). Epidemic disease and the state: Is there a tradeoff between public health and liberty? Public Choice. https://doi.org/10.1007/s11127-021-00944-4
Kummitha, R. K. R. (2020). Smart technologies for fighting pandemics: The techno- and human- driven approaches in controlling the virus transmission. Government Information Quarterly, 37(3), 101481. https://doi.org/10.1016/j.giq.2020.101481
Lazarus, J. V., Ratzan, S. C., Palayew, A., Gostin, L. O., Larson, H. J., Rabin, K., Kimball, S., & El-Mohandes, A. (2021). A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine, 27(2), 225–228. https://doi.org/10.1038/s41591-020-1124-9
Lucchese, M., & Pianta, M. (2020). The coming coronavirus crisis: What can we learn? Intereconomics, 55, 98–104. https://doi.org/10.1007/s10272-020-0878-0
Martinez-Bravo, M., & Sanz, C. (2021). Inequality and psychological well-being in times of COVID-19: Evidence from Spain. Series, 12, 489–548. https://doi.org/10.1007/s13209-021-00255-3
Martínez-Córdoba, P. J., Benito, B., & García-Sánchez, I. M. (2021). Efficiency in the governance of the COVID-19 pandemic: Political and territorial factors. Globalization and Health, 17(1). https://doi.org/10.1186/s12992-021-00759-4
Mazza, P.I., & Mavri, M. (2020). Is this the wright time to talk about cloud regions? The contribution of COVID-19 to concepts of regional development, retrieved from https://ersa.org/wp-content/uploads/2020/07/Note_MazzaMavri.pdf.
McCoy, D. (2020). What exactly is the government’s coronavirus strategy?, Queen Mary University of London, retrieved from: https://www.qmul.ac.uk/media/news/2020/pr/whatexactly-is-the-governments-coronavirus-strategy.html.
McKinsey. (2020). Rethinking resilience: ten priorities for governments. McKinsey & Company Policy Report. November 2020, retrieved from: https://www.mckinsey.com/~/media/mckinsey/industries/public%20and%20social%20sector/our%20insights/rethinking%20resilience%20ten%20priorities%20for%20governments/rethinking-resilience-ten%20priorities-for-governments_f.pdf
McMillen, C. W. (2013). Epidemic diseases and their effects on history, Oxford Bibliographies. retrieved from: https://www.oxfordbibliographies.com/view/document/obo-9780199743292/obo-9780199743292-0155.xml. https://doi.org/10.1093/OBO/9780199743292-0155
Memish, Z. A., Perlman, S., Van Kerkhove, M. D., & Zumla, A. (2020). Middle East respiratory syndrome. Lancet, 395(10229), 1063–1077. https://doi.org/10.1016/S0140-6736(19)33221-0
Mobin, M. A., Mahi, M., Hassan, M. K., Habib, M., Akter, S., & Hassan, T. (2021). An analysis of COVID-19 and WHO global research roadmap: knowledge mapping and future research agenda. Eurasian Economic Review, 1-22. https://doi.org/10.1007/s40822-021-00193-2
OECD. (2020a). The territorial impact of COVID-19: managing the crisis across levels of government, retrieved from: http://www.oecd.org/coronavirus/policy-responses/the-territorial-impact-of-COVID-19-managing-the-crisis-across-levels-of-government-d3e314e1/.
OECD. (2020b). Government support and the COVID-19 pandemic, retrieved from: http://www.oecd.org/coronavirus/policy-responses/government-support-and-the-COVID-19-pandemic-cb8ca170/.
OECD. (2020c). The COVID-19 crisis in the Western Balkans. Economic impact, policy responses, and short-term sustainable solutions, retrived from: http://www.oecd.org/south-east-europe/COVID-19-Crisis-Response-Western-Balkans.pdf.
OECD. (2020d). Policy Responses to Coronavirus (COVID-19). A systemic resilience approach to dealing with COVID-19 and future shocks, April 2020d, retrieved from: https://www.oecd.org/coronavirus/policy-responses/a-systemic-resilience-approach-to-dealing-with-COVID-19-and-future-shocks-36a5bdfb/.
OECD. (2020e). Transparency, communication and trust: The role of public communication in responding to the wave of disinformation about the new Coronavirus. OECD Policy Responses to Coronavirus (COVID-19). OECD Publishing, Paris. https://doi.org/10.1787/bef7ad6e-en.
OECD. (2022). Policy responses to coronavirus (COVID-19): first lessons from government evaluations of COVID-19 responses. A synthesis, retrieved from: https://www.oecd.org/coronavirus/policy-responses/first-lessons-from-government-evaluations-of-covid-19-responses-a-synthesis-483507d6/.
Outka, E. (2020). Viral modernism: The influenza pandemic and interwar literature. Columbia University Press.
Panteli, D., & Maier, C. B. (2021). Regulating the health workforce in Europe: implications of the COVID-19 pandemic. Human Resources for Health, 19, 80. https://doi.org/10.1186/s12960-021-00624-w
Ryu, S., Gao, H., Wong, J. Y., Shiu, E. Y. C., Xiao, J., Fong, M. W., & Cowling, B. J. (2020). Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings—International travel-related measures. Emerging Infectious Diseases, 26(5), 961–966. https://doi.org/10.3201/eid2605.190993
Sapir, A. (2020). ‘Why has COVID-19 hit different European Union economies so differently?’. Policy Contribution 2020/18, Bruegel, retrieved from: https://www.bruegel.org/wp-content/uploads/2020/09/PC-18-2020-22092020-final.pdf.
Spinney, L. (2018). Pale Rider: The Spanish Flu of 1918 and How It Changed the World. Public Affairs (Perseus Books).
Tocci, N. (2020). The COVID-19 global inflection point and Europe’s predicament. Asia Europe Journal, 18, 227–229. https://doi.org/10.1007/s10308-020-00573-4
Tooze, A., & Schularick, M. (2020). The shock of coronavirus could split Europe—unless nations share the burden. The Guardian, 25 March, retrived from: https://amp.theguardian.com/commentisfree/2020/mar/25/shock-coronavirus-split-europe-nations-share-burden.
Walker, S., & Smith, H. (2020). Why has Eastern Europe suffered less from coronavirus than the West?, The Guardian, 5 May, retrieved from: https://www.theguardian.com/world/2020/may/05/why-has-eastern-europe-suffered-less-from-coronavirus-than-the-west.
Wang, Y. (2021). Analysis of the effectiveness of COVID-19 response policies. Wharton Research Scholars, 213. Retrieved from: https://repository.upenn.edu/wharton_research_scholars/213
Welfens, P. J. J. (2020). Macroeconomic and health care aspects of the coronavirus epidemic: EU, US and global perspectives. International Economics and Economic Policy, 17, 295–362. https://doi.org/10.1007/s10368-020-00465-3
WHO. (2020b). World Health Organization Director-General’s opening remarks at the media briefing on COVID-19, 3 March 2020b, retrieved from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---3-march-2020b.
WHO. (2020a). World Health Organisation, WHO rapid response team concludes mission to Italy for COVID-19 response, retrieved from: https://www.euro.who.int/en/countries/italy/news/news/2020a/3/who-rapid-response-team-concludes-mission-to-italy-for-COVID-19-response.
Wiiw. (2020). The wiiw forecasts for Central, East and Southeast Europe”, WIIW, The Vienna Institute for International Economic Studies, 6 May.
Worldometer (2022). COVID-19 coronavirus pandemic. Retrieved from: https://www.worldometers.info/coronavirus/
Yamamoto, N., & Bauer, G. (2020). Apparent difference in fatalities between Central Europe and East Asia due to SARS-COV-2 and COVID-19: Four hypotheses for possible explanation. Medical Hypotheses, 144, 110160. https://doi.org/10.1016/j.mehy.2020.110160
Zhao, X. B. S., Wong, H. C. J., Lowe, C., Monaco, E., & Corbett, J. (eds.) (2021). COVID-19 pandemic, crisis responses and the changing world. Perspectives in Humanities and Social Sciences. Springer. https://doi.org/10.1007/978-981-16-2430-8
Acknowledgements
This research has been conducted with the support of the project PN-III-P4-ID-PCCF-2016-0166 (ReGrowEU), financed by the Ministry of Research and Innovation, CNCS—UEFISCDI and project no. 621262-EPP-1-2020-1-RO-EPPJMO-MODULE ‘EU Interdisciplinary Studies: Widening Knowledge for a more Resilient Union’, co-financed by European Commission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors have no conflicts of interest to disclose.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conficts of Interest/Competing Interests
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ţigănaşu, R., Simionov, L. & Lupu, D. European Governments’ Responses to the COVID-19 Pandemic during the First Wave: Resetting Governance Systems to Cope More Effectively with Future Shocks. Appl. Spatial Analysis 16, 1129–1167 (2023). https://doi.org/10.1007/s12061-022-09481-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12061-022-09481-z