Abstract
The purpose of this work was to obtain genus-specific monoclonal antibodies against the Legionella spp. recombinant PAL protein, which will subsequently allow to use them as a basis for the development of new express tests for pathogenic legionella detection. A short three-week immunization protocol for Wistar rats was used to generate rat–mouse heterohybridomas producing antibodies against PAL. Mouse myeloma cell line Sp2/0-Ag14 served as the fusion partner. Hybridization was performed using two methods: PEG-mediated fusion and electrofusion. Subsequent screening was performed by indirect solid-phase ELISA against the target protein rPAL. Specificity analysis was performed by dot-blot using a panel of lysates obtained from 39 pure cultures of different strains, which included closely related and heterologous microorganisms among others. No difference in the efficiency of stable hybridoma clones production by the two indicated cell-fusion methods was detected. Twelve clones producing specific rat monoclonal antibodies were obtained based on the screening results. The obtained rat monoclonal antibodies are highly specific towards the PAL protein of L. pneumophila of different serological groups and other pathogenic legionella and are good candidates to be used as the components of diagnostic test systems for the detection of pathogenic representatives of the Legionella genus.
Similar content being viewed by others
INTRODUCTION
According to different sources, Legionnaires’ pneumonia constitutes from 0.5 to 16% of all cases of all lower respiratory tract infections [1]. The members of the genus Legionella are stable in the environment and are able to colonize aquatic systems, including artificial ones. Being facultative intracellular parasites, L. pneumophila bacteria carry considerable risks of severe illness, especially in immunocompromised patients, elderly people, and people with concomitant respiratory diseases and risk factors [2]. A significant proportion of pneumonia cases in the Russian Federation, including lethal cases, have unknown etiology, which may be due to the use of inadequate diagnostic methods [3]. Nevertheless, the identification of the etiological agent in pneumonia, especially in the case of severe course, is essential for choosing an effective antibiotic therapy and treatment strategy, with fluoroquinolones and macrolides being the only drugs of choice with proven efficacy against the Legionella genus [2, 4].
Currently, it is recommended that all patients diagnosed with pneumonia undergo a microbiological examination of their respiratory-tract secretions, causative-agent DNA detection, and monitoring of specific immunoglobulins over time, as well as rapid tests for pneumococcal and legionella antigenuria. However, a bacteriological test with isolation and identification of the pathogen culture takes 4–5 days on average, while a negative result for urinary legionella antigen and legionella DNA does not exclude legionellosis, since these tests are only validated for legionella belonging to serological group 1. In addition, an increase in the anti-legionella antibody titers is observed no earlier than 3 weeks after the infection [5]. The main etiological agent of Legionnaires’ pneumonia is indeed L. pneumophila (up to 90% of cases), and this group is prevailed by legionella belonging to serological group I (at least 80% of cases [6]). The representatives of other L. pneumophila serological groups are considered to be pathogenic for human beings as well. The disease is also caused by L. micdadei, L. longbeacheae, L. dumoffii, L. bozemanii, and several other pathogens [7].
Peptidoglycan-associated lipoprotein (PAL) is an outer-membrane protein of Gram-negative bacteria, which, among other things, is responsible for the bacterial pathogenesis. The PAL protein is specific to the Legionella spp. genus and can be used for both legionella detection and immunoprevention [8]. PAL can be detected in the urine of patients with Legionnaires’ pneumonia by immunochemical methods starting at days 2–3 from the manifestation of the disease. Such tests do not require the accumulation of bacteriological material and can be performed rather quickly, within a few hours [9, 10].
The aim of the present work was to obtain genus-specific rat monoclonal antibodies (MAbs) against the recombinant L. pneumophila PAL protein, which may later be used as a basis for developing new rapid tests for detection of pathogenic Legionella in urine samples from patients with suspected legionellosis disease.
MATERIALS AND METHODS
Production of Recombinant L. pheumophila PAL Protein
The production of an expression construct, expression of the recombinant PAL protein (rPAL) in Escherichia coli cells, its isolation and purification were described in previous works [11, 12].
Rat Immunization Protocol and Animal Selection for Splenocyte Production
The complete Freund’s adjuvant (Sigma-Aldrich, United States) mixed with the PAL protein (initial concentration 1 mg/mL) in a volume-to-volume ratio of 1 : 1 was used as an antigenic emulsion to immunize the laboratory animals. A dose of 150 μg of protein was used to immunize a single animal. The antigen was injected intramuscularly into the tailbase area of young Wistar-line female rats (Scientific Center for Biomedical Technologies of the Federal Medical and Biological Agency, Andreevka Branch, Andreevka, Russia). A booster dose containing the same amount of antigen without the adjuvant was introduced 3 weeks after. The specific activity of the anti-rPAL class G immunoglobulins contained in the serum of immunized animals was measured by indirect solid-phase enzyme immunoassay (ELISA). For this purpose, blood was collected for the analysis from the retro-orbital sinus of rats not earlier than 2 weeks after the first immunization and 2 days after the second one. Rat serum was tested against rPAL immobilized in the wells of the immunological plate (1 μg/well). Immunoglobulin binding to the antigen was detected using goat antibodies against a whole rat IgG molecule conjugated to horseradish peroxidase. The interaction was visualized using chromogenic reagent tetramethylbenzidine (TMB; Thermo Fisher Scientific, United States) and the optical density in the wells of the plate was recorded using a microplate spectrophotometer at a wavelength of 450 nm. Serum dilution with an optical density twice as high as in the negative control well were considered the threshold titer. Optical-density records in the negative control were not higher than 0.15. Animals with the highest titers of specific antibodies were euthanized on the third day after the second immunization, and the spleen was removed.
Obtaining MAb-Producing Hybridomas
Rat splenocytes were obtained by rubbing the spleen over a 100-μm nylon sieve (Fisherbrand, United States) with further separation of the lymphocytic fraction in a Ficoll-Paque PLUS (GE Healthcare, United Kingdom) density gradient. The murine myeloma cell line Sp2/0-Ag14 (ATCC, United States) was used as a fusion partner. Hybridization was performed using two methods, the classical Kohler and Milstein technique involving PEG–DMSO solution as a fusion agent [13] and electrofusion using a BTX ECM2001 apparatus (Harvard Apparatus, United States) and Model 453 microslides (BTX, United States) in BTXpress Cytofusion Medium C (BTX, United States). In both cases, splenocyte and Sp2/0-Ag14 myeloma cells were used in a 3 : 1 ratio. Equal amounts of cells were used in both methods.
Electrofusion was carried out as follows: pre-electroporation cell dielectrophoresis was performed at a voltage of 50 V for 30 s, followed by two rectangular pulses of 500 V each for 30 μs (electroporation), followed by postelectroporation dielectrophoresis at 50 V for 30 s, with subsequent decay to zero in 9 s. After electrofusion, microslides were left to rest for 30 min at room temperature.
After fusion, cells were cultured in 96-well plates without a feeder layer in DMEM medium (Sigma, United States) supplemented with 20% fetal bovine serum (HyClone, GE Healthcare, United States), 2 mM L-glutamine (PanEco, Russia), 100 μg/mL gentamicin (PanEco, Russia), and 1× hypoxanthine-aminopterin-thymidine (HAT) solution (Gibco, Thermo Fisher, United States). Selection on HAT medium was carried out for 3 weeks with medium replacement as it became acidic.
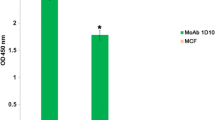
Screening of MAb-Producing Hybrodimas
Screening of cultural liquids from the wells of plates containing hybrid cells was carried out by ELISA against rPAL, starting from the tenth day after hybridization. To perform the screening, 100 μL of culture liquid was taken from each tested well containing hybridomas and transferred into the wells of the plate containing rPAL protein immobilized on their surface. Subsequent procedures were carried out as described above. Each well containing prospective hybrid cells was screened three times. Hybridomas from the wells demonstrating stable or improving results in ELISA were cloned using the limiting-dilutions technique. The monoclonal nature of hybridomas in the culture-plate wells was monitored visually using a microscope. Production of anti-rPAL class G antibodies was controlled using ELISA as described above. Cloning was performed at least than two replicates for each MAb producer. Producer clones with consistently high optical density in ELISA and that were morphologically homogeneous were selected in each case. All the obtained clones were cultured with scaling, and the strains of the obtained hybrids were cryopreserved. The number of stable MAb-producing clones obtained by rat splenocyte fusion with the murine myeloma line was estimated in the case of each of the two methods.
Measuring Specific Antibody Activity
The activity of the obtained MAbs was measured in a dot-blot immunoassay. The assay panel included the original target protein, as well as L. pneumophila strains belonging to different serological groups and other Legionella genus representatives, in addition to strains of Gram-negative bacteria the PAL protein of which was highly similar to that produced by Legionella (according to the UniProt database), pneumonia causative agents and bacteria causing urinary-tract infections (see Table 1). All strains were obtained from the State Collection of Pathogenic Microorganisms of the State Scientific Center for Applied Microbiology and Biotechnology. Suspensions of microorganisms, initially prepared at a concentration of 109 microbial cells (mc)/mL, were inactivated by boiling. Antigens were applied to a Hybond ECL nitrocellulose membrane (GE Healthcare, United Kingdom) using a Bio-Dot microfiltration system (Bio-Rad, United States) in an amount of 1 μg/spot (for protein antigen) or 106 mc/spot (for inactivated bacterial suspensions). Membranes were blocked with nonfat lactose-free milk. The membranes were then incubated in cultural liquids obtained by culturing cloned MAb-producing hybridomas in a monolayer. The binding of MAbs from the cultural liquid with the targets on the membrane was detected using goat antibodies against a whole rat IgG molecule conjugated to horseradish peroxidase. Binding was visualized with diaminobenzidine solution with added nickel and cobalt chlorides (all from Sigma, United States).
RESULTS AND DISCUSSION
Choosing a rat model to produce antibodies against rPAL has several advantages. First, the rat immune system is more responsive to simple protein antigens than the mouse system. Second, despite the lower efficiency of cell fusion, obtained hybridomas remain stable for years and rather rarely need to be cloned again [14].
Rats were immunized using a short protocol on the assumption that, between weeks 2 and 3 after the first injection, the production of specific class G antibodies is at the highest level [15]. Anti-rPAL antibody titers in different animals ranged from 1 : 4000 to 1 : 32 000 2 weeks after immunization and from 1 : 8000 to 1 : 256 000 after 3 weeks. Finally, three hyperimmune rats with antibody titers of at least 1 : 128 000 were selected out of six animals.
Hybridization efficiency using different fusion methods at the initial stage was assessed on the basis of the number of ELISA-positive wells containing hybridomas 10 days after fusion. The overall efficiency of electrofusion was 9.17%, while that of the PEG-DMSO fusion technique was 16.46% [15]. After cloning, the number of obtained stable producer clones was estimated. As a result, 12 stable individual hybridoma clones were obtained, with five of them having been produced using electrofusion and seven using the Kohler and Milstein method. These results cannot be processed using statistical methods, due to the fact that insufficient number of animals was involved in the experiment.
All the obtained rat MAbs are highly specific towards the target rPAL protein and interact with varying degrees of intensity with all L. pneumophila strains used in the panel, both reference and clinical isolates, as well as with the representatives of other Legionella spp. species (see Table 1). This can be explained by the different levels of expression of the target PAL protein in different strains. MAbs tend, but in different ways, to interact with the other Legionella spp. representatives, suggesting that PAL protein has structural differences within the Legionella genus. A comparative analysis of the UniProt sequences most similar to the original PAL antigen (P26493 (PAL_LEGPN)) showed that PAL proteins share 100% identity within the species and 71.2% identity within the genus. All the obtained MAbs showed no specificity towards any bacterial strain other than Staphylococcus aureus, which is a predictable result, as this species synthesizes membrane protein A, which is recognized by all class G immunoglobulins [16]. Hence, false positives resulting from antibody interactions with S. aureus cannot be completely ruled out in any immunoassay.
Currently, only two test systems for Legionella identification using monoclonal or polyclonal antibodies are produced in Russia. The first one is an immunochromatography test based on gold-labelled antibodies against L. pneumophila 1 LPS of L. pneumophila (a L. pneumophila 1 test strip, reagent kit for rapid identification of legionellosis pathogen “L. pneumophila 1 Test strip” RZN 2013/742), and the second is a latex test system based on antibodies against the membrane protein p29 of L. pneumophila 1 (latex test system LEGIONELLA PNEUMOPHILA serotype 1 reagent kit for rapid identification of Legionella pneumophilia in a latex agglutination reaction, liquid, RZN 2013/1278 produced by the State Scientific Center for Applied Microbiology and Biotechnology, Obolensk). Immunoassay-based test systems for the detection of legionellosis antigen in urine manufactured by Alere Inc (USA) are also available, registered and used in the Russian Federation: BinaxNOW Legionella Urinary Antigen Card IC test and Binax Legionella Urinary Antigen EIA ELISA test (FSZ 2008/02110). Both test systems have been validated only for detection of the L. pneumophila serogroup 1 antigen in urine. Using the rat MAbs obtained in the present work (e.g., mabPAL 2.4 or 2.33), a diagnostic test system capable of efficiently detecting not only L. pneumophila serogroup 1, but also legionellas from other serogroups and species, can be developed. Although the vast majority of Legionnaires’ disease cases are caused by L. pneumophila 1, other serogroups and species cause no less severe pneumonias. It is important to detect a Legionella infection at an early stage, regardless of the type of legionella involved, since prolonged inefficient antibiotic therapy aggravates the disease and increases the chance of an unfavorable disease outcome.
A test system based on the obtained antibodies will detect not only the most important L. pneumophila serogroup 1, but also other Legionella species within the genus. The literature data confirm this possibility [8], but, in order to more accurately determine the specificity of the obtained MAbs towards all Legionella representatives, the collection of strains needs to be extended to further investigate the specific activity of the obtained MAbs.
CONCLUSIONS
In our opinion, both methods used to obtained hybrid rat MAb-producing cells performed very well. Although the classical PEG–DMSO-based fusion method showed a comparatively higher fusion efficiency at the initial stage (16.46% of positive production wells vs. 9.17% positive wells after electrofusion), the two methods demonstrated no significant difference in the final result expressed in the production of stable clones producing specific MAbs.
The MAbs obtained in the present work apparently have specificity towards different rPAL epitopes and, for this reason, show different detection profiles in the case of the test microorganism panel used. The combination of mabPAL_2/4 and mabPAL_2.23 can successfully detect all the Legionella genus strains used in the work, while mabPAL_6.23 may be used as a complementary test to detect only the representatives of the Legionella pneumophila species.
REFERENCES
Chuchalin, A.G., Sinopal’nikov, A.I., Tartakovskii, I.S., Karpova, T.I., Dronina, Yu.E., Sadretdinova, O.V., et al., Practical recommendations for the diagnosis and treatment of legionella infection caused by Legionella pneumophila serogroup 1, Clin. Microbiol. Antimicrob. Chemother., 2009, vol. 11, no. 1, pp. 4–13.
Chuchalin, A.G., Sinopal’nikov, A.I., Kozlov, R.S., Avdeev, S.N., Tyurin, I.E., Rudnov, V.A., et al., Klinicheskie rekomendacii. Vnebol’nichnaja pnevmonija u vzroslyh (Clinical Recommendations. Community-Acquired Pneumonia in Adults), Moscow: Ministry of Healthcare of the Russian Federation, 2019. https://rushiv.ru/vnebolnichnaya-pnevmoniya-u-vzroslyh-klinicheskie-rekomendatsii/. Accessed October 30, 2020.
Gruzdeva, O.A., Filatov, N.N., Tartakovskii, I.S., and Mar’in, G.G., Epidemiological features of legionellosis in the Russian Federation, Epidemiol. Infect. Dis., 2017, vol. 22, no. 2, pp. 86–90. https://doi.org/10.18821/1560-9529-2017-22-2-86-92
Chuchalin, A.G., Sinopal’nikov, A.I., Kozlov, R.S., Avdeev, S.N., Tyurin, I.E., Rudnov, V.A., et al., Clinical guidelines for the diagnosis, treatment, and prevention of severe community-acquired pneumonia in adults, Clin. Microbiol. Antimicrob. Chemother., 2015, vol. 17, no. 2, pp. 84–126.
SP (Sanitary and Epidemiological Regulations) no. 3.1.2.2626-10: Prevention of Legionellosis, Moscow: Federal Center of Hygiene and Epidemiology of Russian Federal Service for Surveillance on Consumer Rights Protection and Human Wellbeing, 2010.
Tartakovskii, I.S., Diagnosis and prevention of legionellosis, Poliklinika, 2015, no. 2-1, pp. 40–43.
Yeruslanov, B.V., Svetoch, E.A., and Mitsevich, I.P., Legionellosis and its laboratory diagnosis, Bacteriology, 2018, vol. 3, no. 3, pp. 58–67.
Kim, M.J., Sohn, J.W., Park, D.W., Park, S.C., and Chun, B.C., Characterization of a lipoprotein common to Legionella species as a urinary broad-spectrum antigen for diagnosis of Legionnaires’ disease, J. Clin. Microbiol., 2003, vol. 41, no. 7, pp. 2974–2979. https://doi.org/10.1128/jcm.41.7.2974-2979.2003
Jarraud, S., Descours, G., Ginevra, C., Lina, G., and Etienne, J., Identification of Legionella in clinical samples, in Legionella. Methods in Molecular Biology (Methods and Protocols), Buchrieser, C. and Hilbi, H., Eds., Totowa, NJ: Humana Press, 2012, vol. 954, pp. 27–56. https://doi.org/10.1007/978-1-62703-161-5_2.
Shimada, T., Noguchi, Y., Jackson, J.L., Miyashita, J., Hayashino, Y., Kamiya, T., et al., Systematic review and metaanalysis, Chest, 2009, vol. 136, no. 6, pp. 1576–1585. https://doi.org/10.1378/chest.08-2602
Zeninskaya, N.A., Kozyr’, A.V., Kolesnikov, A.V., Ryabko, A.K., Mar’in, M.A., Lisitskaya, L.A., et al., RF Patent 2634385, Byull. Izobret., 2017, no. 30. https://new.fips.ru/registers-doc-view/fips_servlet?DB= RUPAT&DocNumber=0002634385&TypeFile=htm. Accessed October 30, 2020.
Zeninskaya, N.A., Ryabko, A.K., Kolesnikov, A.V., Kozyr’, A.V., Marin, M.A., Firstova, V.V., et al., The preparation of recombinant peptidoglycan-associated lipoprotein (PAL) Legionella pneumophila and characterization of its immunogenic properties, Immunologiya, 2018, vol. 39, no. 1, pp. 50–55.
Kohler, G. and Milstein, C., Continuous cultures of fused cells secreting antibody of predefined specificity, Nature, 1975, vol. 256, no. 5517, pp. 495–497. https://doi.org/10.1038/256495a0
Campbell, A., Monoclonal Antibody and Immunosensor Technology—The Production and Application of Rodent and Human Monoclonal Antibodies. Laboratory Techniques in Biochemistry and Molecular Biology, Elsevier, 1991. https://doi.org/10.1016/s0075-7535(08)70055-x.
Sado, Y., Inoue, S., Tomono, Y., and Omori, H., Lymphocytes from enlarged iliac lymph nodes as fusion partners for the production of monoclonal antibodies after a single tail base immunization attempt, Acta Histochem. Cytochem., 2006, vol. 39, no. 3, pp. 89–94. https://doi.org/10.1267/ahc.06001
Hober, S., Nord, K., and Linhult, M., Protein A chromatography for antibody purification, J. Chromatogr. B, 2007, vol. 848, no. 1, pp. 40–47. https://doi.org/10.1016/j.jchromb.2006.09.030
Funding
This work was supported by the NIR 054 Program “Development of New-Generation High-Efficiency Test Systems to Detect Pathological Agents of Nosocomial Infections Based on Immune-Aptamer PCR.”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest. The authors declare that they have no conflict of interest.
All animal-experimentation protocols were approved by the State Scientific Center for Applied Microbiology and Biotechnology Bioethics Committee. All experimentation was carried out in full accordance with GOST (State Standard) 33216–2014 “Guidelines for Keeping Laboratory Animals.” No experimentation involving human beings was carried out by any of the authors.
Additional information
Translated by E. Martynova
About this article
Cite this article
Zeninskaya, N.A., Riabko, A.K., Marin, M.A. et al. Production and Characterization of Rat Monoclonal Antibodies against the PAL Antigen of Legionella spp.. Mol. Genet. Microbiol. Virol. 37, 65–70 (2022). https://doi.org/10.3103/S0891416822020082
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3103/S0891416822020082