Abstract
Valvular heart disease affects 30% of the new-borns with congenital heart disease. Valve replacement of semilunar valves by mechanical, bioprosthetic or donor allograft valves is the main treatment approach. However, none of the replacements provides a viable valve that can grow and/or adapt with the growth of the child leading to re-operation throughout life. In this study, we review the impact of donor valve preservation on moving towards a more viable valve alternative for valve replacements in children or young adults.
Similar content being viewed by others
Background
To treat valvular heart disease, around 50,000 semilunar valve replacements are performed each year in both adult and pediatric patients in Europe (Mylotte et al. 2013), (Butchart et al. 2005). Anomalies of the aortic or pulmonary valve that require valvular replacement occur in 30% of new-borns with congenital heart disease (Alkashkari et al. 2018). These anomalies can result in valve stenosis (restricted blood flow through the cuspal opening) or valve regurgitation (incomplete valve closure and blood backflow) (O’Donnell and Yutz 2020). Valve stenosis or regurgitation can lead to increased cardiac workload, ventricular dysfunction and congestive heart failure (Mrsic et al. 2018).
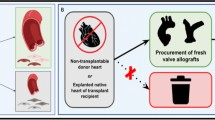
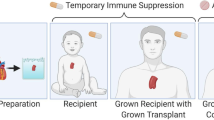
To prevent progression towards heart failure in patients with congenital semilunar heart valve defects, there are several options to replace the diseased valve, albeit these are mainly fit for the adult population. These include: mechanical valves, bioprosthetic valves, pulmonary autograft in combination with an allograft valve (Ross procedure) and allograft valves. For the regurgitating aortic valve, autologous pericardium tissue has been attempted and deemed successful in multiple cases for valve reconstruction in adults (Amabile, et al. 2022) and young adults(Odim et al. 2005). For the mitral valve, valve reconstruction is more often performed than valve replacement (in 75.4% of the cases in the Netherlands) (Siregar et al. 2014). In neonates and children, repair of semilunar valves using autologous tissue is the preferred option over replacement (Hammer et al. 2017). Unfortunately, surgical repair of semilunar valves is often not possible or has to be followed by valve replacement (Hawkins et al. 2007). In children, durability of the available valve substitutes is the main concern as valve size and performance are directly related to growth of the heart resulting in patient valve mismatch. Although still debated, the Ross procedure, placement of the pulmonary autograft in the aortic position and an allograft valve in the pulmonary position, is considered the preferred valve replacement in children (Etnel et al. 2016; Takkenberg et al. 2005). The pulmonary autograft is vital, the right size, has optimal hemodynamic properties and has the potential to grow in diameter with the growing heart. Furthermore, in contrast to mechanical or bioprosthetic valves, the pulmonary autograft and allograft offer good hemodynamic performance, decreased risk of endocarditis and do not require the use of anticoagulation (Lupinetti et al. 2003; Nappi et al. 2018). Additionally, a study comparing mechanical valve replacement versus human tissue allografts showed children with allograft valves have longer survival and freedom from valve-related complications compared to children after mechanical valve placement in the aortic position (Lupinetti et al. 1999). Nevertheless, early failures of allograft valves within less than 10 years have been attributed to structural degeneration, immunologic responses and loss of cellular viability and valve growth capacity (Takkenberg et al. 2002), (Junnil et al. 2021). Autograft failure due to dilation of the valve instead of growth due to the increased mechanical stress at the aortic position compared to the pulmonary position has been reported (Etnel et al. 2018). To increase the duration of storage and increase the availability of donor valves, cryopreservation protocols were developed for tissue banking of valve allografts (Jashari 2021). Cryopreservation of valves initially showed no significant structural deterioration compared to fresh valves (Burkert et al. 2021; Witten et al. 2021). However, extensive investigation of matrix composition and cell survival after implantation revealed loss of structural organization of collagen within the valve layers and cellular damage which could predispose the valves for early structural failure (Schenke-Layland et al 2007), Schenke-Layland et al. 2006). Improving the current method of valve allograft preservation in tissue banks to better maintain valve structural integrity, function, and viability would greatly benefit allograft valve durability and limit the need for re-intervention in children with congenital heart valve defects. The ultimate goal should be to preserve vitality of the allograft, i.e., including cell viability, so that it maintains the ability to grow and remodel when implanted in the heart of a child.
In this review, we discuss current methods, problems and optimizations of semilunar valve preservation to move towards a more viable donor valve alternative for transplantation in children.
Hallmarks of heart valve preservation—What needs to be preserved?
Heart valves open and close over 3 billion times during a lifetime to maintain unidirectional blood flow from the heart to the lungs and to the rest of the body (Schoen 2011). To achieve this, semilunar heart valves are organized in three structural layers with different extracellular matrix (ECM) compositions: the collagen-rich fibrosa, proteoglycan-rich spongiosa and elastin-rich ventricularis layer (Valk et al. 2018) (Fig. 1A). The presence of valvular endothelial cells (VECs) and interstitial cells (VICs) maintains integrity of the valves and enables valve growth and remodelling during life. The guiding principles of heart valve preservation are to maintain function, shape and viability of the heart valve. To achieve this, the components of the valve (i.e. the cells, ECM and the structural organization) need to be preserved.
Effect of tissue processing and preservation on heart valve allograft durability. A Schematic representation of healthy vital heart valve with growth capacity. B Schematic representation of heart valve allograft after harvesting and preservation (either short-term preservation at 4 °C or long-term cryopreservation) showing loss of the structural differences of the three valve layers, elastin fragmentation, collagen disruption, and loss of VECs and VICs. C Schematic representation of cryopreserved heart valve allograft after transplantation showing infiltration of immune cells, a low number of host interstitial cells, and complete loss of the endothelial layer. VEC, valvular endothelial cell; VIC, valvular interstitial cell
The role of valvular endothelial cells
VECs line the valvular surface that is in contact with circulating blood. Their function relates to shear stress and maintaining the non-thrombogenic surface of each side of the valve that is exposed to distinct hemodynamic profiles (Schoen 2008; Ayoub et al. 2017). Additionally, communication between VECs and VICs located in the structurally distinct valvular layers mediates valvular flexibility. VECs as the mechanical sensor of the valve respond to changes in shear stress and flow and to nerve innervation (El-Hamamsy et al. 2009; Marron et al. 1996). Despite the prominent role of VECs in valve function, analysis of allograft valves showed little to no intact VECs on the surface of the valves prior to transplantation (Kamp et al. 1981), (Pfitzner et al. 2018) and of explanted failed allograft valves (Koolbergen, et al. 1998; Hawkins et al. 2003) (Fig. 1B, C). It has been proposed that the methods used to preserve and sterilize allograft valves cause loss of the valvular endothelium (Fabian, et al. 2022; Krs et al. 2004). Increasing the abundance and viability of VECs is considered an important step to increase durability of valve allografts after transplantation. However, the presence of donor VECs on the outer layers of the leaflet that are exposed to blood flow (leaflet surface) also contribute to allograft immunogenicity and immune-related graft rejection has been observed in neonates and infants (Hawkins et al. 2003; Rajani et al. 1998). Whether increasing the survival of VECs on the leaflet would be beneficial for valve performance by protecting the valve or would increase immunogenicity remains unclear. There is evidence that VECs could induce immune reactivity due the expression of immunogenic epitopes (αGal and human leukocyte antigen (HLA) proteins) (Johnson et al. 1997), (Farivar et al. 2003b), (Simon et al. 1998). However, the already observed immune reactivity to preserved valves is not related to VECs as they contain little to no remaining VECs. If immunogenicity of VECs could be prevented, improving viability and integrity of the VEC layer would be an important factor to improve allograft integration and durability.
The role of valvular interstitial cells
Single cell analysis of valve cellular phenotypes in post-natal development till day 30 in mice indicates VEC subpopulations remain stable while VICs undergo changes in gene expression and cell function (Hulin et al. 2019). The dynamic behaviour of VICs is necessary to maintain the structural integrity of the valve during life by regulating protein synthesis and enzymatic degradation of the ECM (Ayoub et al. 2017). By secreting cytokines, growth factors, ECM components and matrix metalloproteases (MMPs) as well as their inhibitors, VICs control the structural characteristics of the three separate valve layers. While VECs are primarily localized at the leaflet surface, VICs can be found dispersed in all valve layers (Bertipaglia et al. 2003; Rabkin-Aikawa et al. 2004a). VIC characteristics change during homeostasis, development and valve disease when they adopt a smooth muscle cell, myofibroblast or osteoblast-like phenotype to enable matrix degradation and remodeling. To illustrate, VICs are responsive to vasoactive agents by increasing collagen synthesis to mediate sustained mechanical properties of the valve during variable blood pressure. Valve layer specific alterations within VICs with changing physiological pressure were found to be induced within 75 ms to mediate a resilient dynamic valve function (Huang et al. 2007). While VICs are pivotal in the functioning of healthy valves, the highly variable nature of VICs has been considered a contributing factor to structural deterioration of allograft valves as activated VICs can contribute to valve calcification (Rabkin-Aikawa et al. 2004a; Rabkin-Aikawa et al. 2004b). Changes in ECM stiffness as a result of allograft valves processing and preservation can in turn alter the VIC phenotype via the PI3/AKT elasticity sensitive pathway (Stassen et al. 2017), (Wang et al. 2013). The combination of loss of cellularity of allograft valves and a change in the phenotype of the remaining VICs could result in valve failure. Moreover, the pulmonary autograft can cause VIC activation as a result of the altered mechanical environment at the aortic position as opposed to the pulmonary position (Rabkin-Aikawa et al. 2004a). Additionally, sex- and age-related differences in gene expression by VICs have been reported to contribute to VIC plasticity (McCoy et al. 2012; Aikawa et al. 2006). Analysis of age-dependent differences in cryopreserved heart valves show more cells in younger valves and an increased collagen cross-linking and valve stiffness in older valves (Geemen, et al. 2016). In neonates, valves contain a higher VIC density and more activated VICs compared to adults (Aikawa et al. 2006). The presence and phenotype of VICs in neonatal heart valves enables valve growth, emphasizing the importance of preserving VICs and the VIC phenotype when transplanting allograft valves in young children (Rabkin-Aikawa et al. 2004a; Anstine et al. 2016).
The role of the valvular extracellular matrix
The composition and organization of the valvular ECM regulated by the valvular cells enables valve deformation while maintaining the structurally distinct valve layers. The three layers of the valve, the fibrosa, spongiosa and ventricularis, function independently to absorb and adapt hemodynamic force and achieve complete valve closure during each cardiac cycle (Valk et al. 2018; Kodigepalli et al. 2020). Collagen, as the main stress bearing component of the valve, provides stiffness and strength while proteoglycans stabilize and elastin mediates flexibility and recoil by permitting deformation and reformation. Remodelling of the valve ECM as a consequence of altered mechanical loading (Pant et al. 2018) or post-natal valve stratification (Hulin et al. 2019) is mediated by VECs and VICs and essential to maintain valve function throughout the millions of cycles during life of valve opening and closing (Kodigepalli et al. 2020). The valvular ECM has been the base for valve tissue engineering approaches and loss of valve ECM integrity in allograft valves negatively impacts durability (Schenke-Layland et al. 2006; Fabian, et al. 2022). The loss of cellularity of allograft valves have led to the notion that allograft valves, as they are currently preserved, function as natural scaffolds to serve as a template for cellular attachment of circulating endogenous cells (Mendelson and Schoen 2006). Comparison of the pulmonary autograft and the pulmonary allograft showed loss of the three-laminar valvular structure in the pulmonary allograft alone (Rabkin-Aikawa et al. 2004b). A significantly lower collagen content was found in pulmonary allografts with progressive collagen hyalinization and loss of cellularity. A loss of elastin fibres in the ventricular layer was observed before implantation due to preservation conditions (Schenke-Layland et al. 2006). Progressive loss of the differential phenotype of the valvular layers after implantation in combination with cellular loss majorly contributes to structural valve detoriation and valve failure (Brockbank et al. 2012).
Classic preservation methods
Preservation at 4 °C of “fresh” valves
For heart transplantations, hearts are preserved at 4 °C in preservation or saline solution in an ice container after which the heart is transplanted within four hours of circulatory death (Copeland et al. 2020). To optimally preserve hearts multiple preservation solutions are used ranging in composition. Additives like gluconate, acetate, lidocaine, albumin, insulin, THAM, heparin, procaine, methylprednisolone, and citrate–phosphate-dextrose have been frequently used for myocardial preservation and to minimize the adverse effects of ischemia (Demmy et al. 1997). Similarly, allograft heart valves were initially preserved at 4 °C in preservation solution for a variable duration ranging from days to weeks (Takkenberg et al. 2002; Lang et al. 1994). The composition of the preservation solution to preserve allograft heart valves varies between studies (i.e. DMEM or RPMI-1640 media supplemented with foetal calf serum or HEPES (Lang et al. 1994; Gerson et al. 2009)) although most studies do not report the preservation solutions used. It is important to note that valves preserved via this method are named “fresh valves” in literature (Schenke-Layland et al. 2006; Fabian, et al. 2022; Koolbergen et al. 2002), (O’Brien et al. 1987) despite the frequently observed loss of valve viability and loss of valve functionality compared to valves directly after extraction (Burkert et al. 2008). Therefore, we believe that preservation at 4 °C for periods up to 95 days is unlikely to reflect the functionality and viability of fresh valves.
Cryopreserved valves
The limited availability of donor organs and the short time-window between organ removal and transplantation has pushed the transplantation field to develop alternative methods that enable long-term organ preservation. By slowly decreasing temperature in combination with agents that prevent crystallization, tissues can be cryopreserved for multiple years at ~ − 135 °C using liquid nitrogen (Lisy et al. 2017). Preservation solutions for cryopreservation contain nutrient media, foetal calf serum and dimethyl sulfoxide (DMSO) or glycerol to prevent ice crystallization (Table 1). Cryopreservation aims to inhibit cellular metabolism to prevent the activation of biological and chemical processes that cause ex vivo tissue degradation and cell death (Taylor et al. 2019). After long-term storage, cryopreserved tissue can be quickly thawed and washed to remove cryoprotective agents (e.g., DMSO/glycerol) before transplantation. Using freezing containers that control the rate of freezing by lowering the temperature with 1 °C per minute accompanied by DMSO-containing nutrient media is now the main method of cryopreservation to preserve human allograft heart valves (Angell et al. 1989), (Mirabet et al. 2008).
Preservation type and valve durability
The impact of preservation method in valve performance and freedom from reoperation has been studied extensively. In Table 1, different preservation techniques as studied in previous studies are compared in relation to reported valve performance and cellular viability. Currently, cryopreservation below − 80 °C using DMSO-containing preservation solution is the main method for valve preservation as it was believed to increase cellular viability and improve valve performance (O’Brien et al. 1987; O’Brien et al. 1991). However, contradictory results have been published on whether cryopreservation causes superior valve durability compared to fresh valves with studies indicating improved performance of cryopreserved allograft valves (O’Brien et al. 1991; O’Brien et al. 1995) and studies observing no differences (Lang et al. 1994; Koolbergen et al. 2002; O’Brien et al. 2001) or decreased valve structural integrity (Burkert et al. 2008). Interestingly, multiple studies analysing performance of allograft valves do not report the storage conditions including storage media or storage duration which can substantially affect valve performance (Table 1).
Even though cryopreservation in DMSO-containing preservation solution is now considered the golden standard for valve allograft preservation, a study on 1022 aortic valve replacements showed no difference between structural valve detoriation in fresh and cryopreserved valves (although duration of storage is not reported) (O’Brien et al. 2001). Of note, the difference between cryopreservation and cold static storage at 4 °C might be insignificant if cryopreservation is preceded with a long period of storage at 4 °C. To illustrate, this was reported to be the case in a recent study with a period of up to 28 days of storage at 4 °C before cryopreservation (Fabian, et al. 2022). Despite the inconsistencies in literature regarding differences in cryopreserved or fresh valves, it is important to note that neither short-term cold static storage at 4 °C nor cryopreservation leads to the implantation of viable valves with growth potential. Especially in implantations that require valves with a smaller diameter, the absence of allograft growth potential due to valve non-viability remains a big predictor of early valve failure.
Reasons of valve failure after preservation
Both valves preserved at 4 °C and cryopreserved allograft valves that were explanted due to stenosis, valvular leakage, or non-cardiac death showed limited cellularity within 1 year after implantation which is likely to have negatively impacted the valves ability to adapt, hemodynamic properties and structural integrity (Koolbergen et al. 2002). Additionally, within this first year after transplantation, the three-layered structure of the valve was lost, which was not observed in pulmonary autografts (Rabkin-Aikawa et al. 2004b). It is important to note, the only available information on allograft histology after implantation comes from failed allografts which biases the reported results. Loss of the valvular tri-laminar structure in pulmonary allografts is likely to be related to valve preservation, ex vivo processing, the surgical procedure and immune reactivity. Multiple steps of our current methods of valve preservation contribute to the loss of cellularity and ECM integrity.
Ischemia
The loss of valve allograft cellularity has been attributed to ischemia after harvesting and the process of valve harvesting, cryopreservation and thawing (Mitchell et al. 1998). The shift from the provision of oxygenated blood to the valves in vivo to the absence of oxygenation after circulatory death and valve harvesting leads to a period of ischemia. Arresting metabolic activity through immersion in liquid nitrogen is believed to end this period of ischemia (Messier et al. 1992). A massive loss of VECs has been observed in both fresh and cryopreserved valves as a result of valve extraction, handling and loss of oxygenated blood flow (Pfitzner et al. 2018). Controversies remain on the degree of valve viability following cryopreservation and implantation. Overall cellular viability of cryopreserved donor allograft valves has been described to exceed 50% when the period between circulatory death and cryopreservation is less than 48 h (Niwaya et al. 1995; Yap and Yii 2004). Of note, this period is often longer and it remains to be seen whether the remaining viable cells can have a beneficial function after transplantation. Longer ischemia before preservation decreased valve cellularity (Lang et al. 1994; Yap and Yii 2004). Specifically, warm ischemia time (20–24 °C) has been considered a critical determinant of cellular viability of valve allografts where 37% cellular damage was observed within 2 h after isolation, increasing to 73% after 6 h (Crescenzo et al. 1992). 24 h of warm ischemia alone was found not to cause cellular ATP depletion while the combination of ischemia with cryopreservation did (Messier et al. 1992). Of note, it remains difficult to directly link cellular viability to maintained interstitial and endothelial cell phenotype and cellular function after implantation. Additionally, heart valves in complete heart transplantations showed less structural deterioration than allograft heart valves, understandably explained by decreased ischemia and the absence of cryopreservation or long term storage during heart transplantations (Mitchell et al. 1998).
Interstitial ice formation in cryopreserved valves
During the process of cryopreservation, intercellular ice formation increases solute concentration causing cellular dehydration as water leaves the cells due to osmosis (Elliott et al. 2017). After rewarming, the cells hydrate and the DMSO leaves the cells during washing with DMSO-free solution (Pegg 2010). While commonly used agents DMSO and glycerol can efficiently protect cells from ice formation during the process of cryopreservation if the cooling rate is controlled (Brockbank et al. 2015), ice formation in the intercellular area causes damage to the tissue ECM. Both fragmentation of ECM components and loss of the laminar organization have been associated with the process of ice crystal formation during cryopreservation (Schenke-Layland et al. 2006; Shaddy et al. 1996). In 2000, Brockbank et al. observed interstitial ice formation in 75% of the cryopreserved heart valve leaflets while using anti-crystallization agents DMSO or glycerol (Pegg 2010). The formation of intercellular ice crystals was found to primarily induce damage of the valve ECM with smaller crystals in the ventricularis than in either the spongiosa or fibrosa layer (Brockbank et al. 2012; Shaddy et al. 1996). Especially ice crystal formation in the spongiosa layer was observed causing loss of valve structural integrity in the middle of the valve. Furthermore, an observed decrease in second harmonic field signals in multiphoton imaging, indicated a loss of the native structural organization of the collagen fibres in cryopreserved valves (Shaddy et al. 1996). In order to prevent tissue damage as a result of ice formation, ice-free cryopreservation methods have been developed, so called vitrification. Here, the presence of high concentrations of cryoprotectants that interact with and replace water prevent water molecules to nucleate to form ice during cooling (Shaddy and Hawkins 2002). In contrast to cryopreservation, vitrified tissue did not show damage to the ECM indicating the correlation between ice crystal formation and damage to the tissue ECM (Welters et al. 2001).
Immunological responses
Whether immunological responses are responsible for valve allograft failure remains elusive although calcification of allografts does suggest a role of the immune system in valve failure. A previous study comparing the structural viability and integrity of cryopreserved allograft valves at different durations after implantation showed that prior to implantation the valvular three-laminar structure was still visible with only slight loss of collagen and cellular autolysis (Mitchell et al. 1998). However, even after a short period of 1–8 days of implantation, the valve showed progressive loss of the three-laminar valve structure and the number of remaining VICs and VECs. Infiltration of inflammatory cells, including neutrophils, macrophages, and T-lymphocytes was reported to be scarce within years after implantation as measured in 16 explanted aorta valves of which 5 were explanted from patients younger than 10 years of age (Mitchell et al. 1998). On the contrary, other studies report the formation of HLA type 1 and 2 antibodies within 12 months after valve transplantation (Hawkins et al. 2003). Additionally, a study measuring HLA-antibody production 3 months after valve allograft implantation at the aortic position in children reported a strong increase in circulating HLA antibodies (Shaddy et al. 1996). Furthermore, analysis of failed homograft valves in 5 children, all failed within 8 months of implantation, showed thickened valve leaflets, interstitial cell activation and foci of T- and B-lymphocytes while 7 valves explanted from adults showed structural deterioration and calcification without inflammation (Rajani et al. 1998). It remains unclear whether the immunologic response plays a role in the increased failure of allograft valves in children compared to adults (Hawkins et al. 2003; Shaddy et al. 1996), (Welters et al. 2001) (Smith et al 1995). However, a mismatch in HLA and blood group (ABO) has been associated with accelerated allograft failure in children (Baskett et al. 2003), (Yankah et al 1987). The advantage of allograft cellular viability and the disadvantage of immunogenicity require consideration when attempting to develop a better valve alternative.
Optimizing heart valve preservation
Preservation solutions for cryopreservation
With the described problems of allograft heart valves preservation, there might be solutions to avoid these (Table 2). The use of additional cryoprotective agents, aside from the currently used DMSO and glycerol, have been proposed to either increase post-freezing cellular viability or increase preservation of the valvular ECM. Agents that could decrease ischemic injury, cryoinjury, or prevent endothelial cell damage have been studied (Taylor et al. 2019). These include agents that actively suppress the metabolic rate (Lesnefsky et al. 2004), (Burwell et al. 2009), apoptosis inhibitors (Ha et al. 2016), (Baust et al. 2000), (Zhang et al. 2009), prevention of cryoinjury (Amir et al. 2003), and trophic factors that improve post-thawing recovery (McAnulty et al. 2002; Ostrózka-Cieślik and Dolińska 2020). To protect against ice crystal formation during the freezing and thawing process which causes cellular damage, attempts have been made to learn from protective mechanisms of freeze-tolerant animals (Tas et al. 2021). Antifreeze proteins (AFPs) that bind ice can generate a thermal hysteresis gap by lowering the freeze temperature or can inhibit ice recrystallization to prevent the maturation of small ice crystals into larger ones (Tas et al. 2021; Olijve et al. 2016). Certain polymers, such as poly (vinyl alcohol) and sugars, emulate these traits and have been exploited to lower the amount of DMSO and glycerol for cryopreservation of e.g. red blood cells (Voets 2017). AFPs have been found to enable preservation of rat heart tissue at − 1 °C without loss of viability and myocyte structure (Amir et al. 2003). Rat livers could be preserved at − 4 °C with glycerol and AFPs which decreased structural damage and increased hepatic function (bile production) compared to glycerol alone (Rubinsky et al. 1994). Preservation at even lower temperatures as used during cryopreservation using antifreeze proteins has failed so far in maintaining tissue viability (Wang et al. 1994).
Vitrification
The discovery of ice-crystal formation in cryopreserved heart valves despite the presence of cryoprotective agents such as DMSO led to the development of ice-free cryopreservation methods (Brockbank et al. 2015). Vitrification uses high concentrations of cryoprotectant solution to induce amorphous solidification rather than crystallization and subsequently restrict ice formation (Brockbank et al. 2011; Song et al. 2000). Rat heart valve vitrification using small volumes of a vitrification solution (VS) (VS55) showed no formation of ice crystals with light microscopy, maintained 80% cell viability immediately after thawing and showed decreased calcification following transplantation compared to cryopreserved valves (Brockbank et al. 2015). Rapid cooling and warming of vitrified cryopreserved valve tissue was essential to prevent ice-crystal formation (Lisy et al. 2017). Multiphoton-autofluorescence imaging showed well-maintained ECM in the vitrified cryopreserved heart valves while standard frozen cryopreservation displayed ECM alteration and freezing artefacts. Vitrified sheep heart valves showed no immune cell infiltration after being explanted while cellular viability was maintained (Brockbank et al. 2012; Lisy et al. 2017). It remains unclear whether endothelial or interstitial cells are maintained during vitrification (Lisy et al. 2017).
Vitrification in the presence of AFPs and bioinspired mimics of AFPs has been previously investigated. The use of polyvinyl alcohol (PVA) as an additive in DMSO-free vitrification-based cryopreservation showed improved viability of umbilical cord blood-derived mesenchymal stem cells (Voets 2017). Additionally, using fish-derived AFPs in vitrification-based cryopreservation of matured murine oocytes showed an improvement in cellular structure and function compared to vitrification alone (Voets 2017). Additional use of biocompatible silk fibroin could further prevent devitrification-induced recrystallization/growth of ice during the thawing process (Fan et al. 2022) and potentially improve valve viability and structural integrity. Vitrification is considered a promising approach to improve preservation of heart valves and currently various vitrification solutions are being analysed in anticipation of future clinical trials.
Preservation solutions for maintaining fresh valves
During heart transplantations, preservation solutions are used to maintain cellular viability. Multiple solutions are used for the preservation of hearts for transplantation with a wide variety of composition. Comparison of multiple preservation solutions currently used for pediatric heart transplants (Saline, University of Wisconsin (UW) solution, Celsior, Custodiol) showed no differential effect on patient 1-year survival (Shaw et al. 2020). However, it has also been described that the wide variety of components used in preservation solutions make it hard to determine the exact effect of each component. Furthermore, in vitro culture, VICs and VECs require distinct media composition (heparin supplementation) for the maintenance of cell phenotype which might complicate the preservation of these cells in fresh valves. Of note, cells do respond differently when embedded within their own 3-dimensional ECM environment as opposed to 2-dimensional culture on plastic. Optimising the composition of preservation solutions to increase tissue viability and structural integrity could be studied to enable preservation of fresh vital valves.
Temperature and perfusion
Regulating storage temperature could be a way to preserve viable valves. As native heart valves are preserved in the human body, they can be preserved for a lifetime at 37 °C and in the presence of oxygenated blood perfusion. Possibly, compared to cryopreservation, heart valves could be better stored at higher sub-zero temperatures (Taylor et al. 2019). However, warm ischemic storage at 20–24 °C was found to increase heart valve cellular damage (Crescenzo et al. 1992). Maintaining porcine heart valves at higher sub-zero temperatures under non-ischemic conditions has been recently attempted and shows preserved ECM integrity and cell phenotype (Konduri et al. 2005). This could be a promising approach to improve the preservation of human heart valves for transplantation. Secondly, to decrease ischemia, perfusion with oxygenated solution might be helpful. Normothermic or hypothermic perfusion has been found beneficial in the ex vivo maintenance of the heart (Fleck et al. 2021), liver (Brockmann et al. 2009), lungs (Takahashi et al. 2021) and kidneys (O’Neill et al. 2020) suggesting it could yield beneficial effects in the preservation of heart valves. Ex vivo perfusion of the explanted heart at 37 °C (normothermic perfusion) has been found to be beneficial when the heart is transplanted in children with congenital heart defects that require more complex surgeries to prevent a substantial period of cold ischemic time that could damage the organ (Fleck et al. 2021). Next to normothermic perfusion, hypothermic perfusion at 4 °C has been implemented clinically for kidney and liver transplantations where it shows higher graft success than static storage at 4 °C (O’Neill et al. 2020). Conditioning of organs outside of the human body using perfusion systems increases the time window for transplantation and minimizes organ ischemia (Brockmann et al. 2009). However, it does require the availability of organ perfusion systems and the rapid development of the necessary expertise at clinical centres. For heart valves, perfusion would mean introducing dynamic flow of oxygen and nutrient-rich media through the valves as valves do not contain vessels where blood would flow through as seen in perfusion of vascularised organs. In addition, dynamic flow through the valves might also increase the integrity of the tissue by mimicking the natural mechanical environment of the valve (Hildebrand et al. 2004). Research into the potential of ex vivo organ culture of heart valves at physiological conditions showed promising results on biological characteristics of porcine heart valves after 48 h of ex vivo culture under dynamic conditions (Konduri et al. 2005). Furthermore, bioreactor based culture of mitral valves in the presence of flow showed improved ECM maintenance compared to mitral valves under static culture conditions (Barzilla et al. 2010). Optimising flow conditions including temperature, flow speed, volume and pulsatility could simulate valve maintenance as in vivo conditions. In the development of tissue engineered heart valves (TEHVs), bioreactor based pulsatile flow systems have been used to culture and mechanically condition TEHVs (Sanders et al. 2016). The presence of flow mimics physiological conditions and stimulates the formation of collagen networks while the mechanical stress at different locations of the valve leaflet influences collagen ultrastructure (Balguid et al. 2008). Culturing heart valves under physiological flow conditions might allow for better preservation of valve ECM ultrastructure and keep the valves conditioned to maintain complete valve opening and closing and withstand shear stress. Furthermore, introducing shear stress in valve preservation would be a method to increase the preservation of VECs as it has been found to protect VEC integrity (Schoen 2008).
Alternatives for preservation of living human valves
Next to attempts to improve the preservation of viable heart valve allografts, other approaches to improve allograft valve performance are being investigated. The immunogenicity of heart valves as a result of cells or cellular debris led to the development of valve decellularization approaches. Both xenogeneic and human decellularized valves are being studied as valve alternatives. The lower reoperation rate after transplantation of human decellularized allografts as a result of decreased antigenicity is likely to lead to fast implementation of decellularized allografts in clinical practice (Neumann et al. 2013). Currently, clinical trials in adults are showing promising results on performance of human decellularized heart valves over standard cryopreserved valves (Waqanivavalagi et al. 2020). Even though human decellularized allograft valves are increasingly being used, the issue of cryopreservation-induced damage of the ECM remains. Additionally, the process of decellularization induces valvular damage reducing the concentrations of GAGs and disruption of elastin and collagen depending on the decellularization method used (VeDepo et al. 2017). Clinical implementation of xenogeneic decellularized allograft remains far away as a recent clinical trial in pediatric patients showed rapid valve failure and early mortality within a year after transplantation by eliciting strong immune reactivity (Simon et al. 2003).
Even though the decellularized valve alternative partly overcomes the issue of reoperation due to immune activation and structural valve degeneration, it does not solve the problem of reoperation due to valve outgrowth. Repopulation of the allograft scaffold with circulating host cells was believed to potentially lead to allograft valve vitality. The presence of host fibroblasts cells in the allograft scaffold after implantation in sheep or pigs has previously been observed (Heever 2021; Dohmen et al. 2006). However, repopulation with endothelial cells has not been observed yet, (although there are some reports of in vivo endothelialisation of TEHVs (Motta et al. 2020)), and the numbers of interstitial cells in the scaffolds remain less than in native valves. To further improve the decellularized valve alternative and achieve vital valve tissue ECM remodeling, ex vivo recellularization approaches are also being investigated (Dohmen et al. 2006; Dainese et al. 2012).
Conclusions
Current preservation approaches used in clinical practice before the transplantation of allograft heart valves is far from ideal for pediatric patients as valve viability is lost. Studies analysing the performance of allograft heart valves often do not report important parameters that influence valve viability and structural integrity such as length of preservation, ischemic period and preservation solution and cellularity when implanted. The connection between cell viability and immunogenicity requires delicate finetuning to mediate valve growth and prevent immune mediated valve deterioration.
Advances in cellularisation approaches, perfusion techniques, bioreactors and cryobiology can aid in developing a better valve alternative for children. Specifically valve growth potential dependent on valve viability is essential in preventing the need for reintervention in children.
Data availability
Not applicable.
Abbreviations
- VEC:
-
Valvular endothelial cell
- VIC:
-
Valvular interstitial cell
- ECM:
-
Extracellular matrix
- HLA:
-
Human leukocyte antigen
- MMP:
-
Matrix metalloproteases
- AFP:
-
Antifreeze proteins
- VS:
-
Vitrification solution
- PVA:
-
Polyvinyl alcohol
- DMSO:
-
Dimethyl sulfoxide
- TEHV:
-
Tissue engineered heart valves
References
Aikawa E et al (2006) Human semilunar cardiac valve remodeling by activated cells from fetus to adult: Implications for postnatal adaptation, pathology, and tissue engineering. Circulation 113(10):1344–1352
Alkashkari W, Alsubei A, Hijazi ZM (2018) Transcatheter pulmonary valve replacement: current state of art. Curr Cardiol Rep 20(4):1–13
Amabile A et al. (2022) Standardized aortic valve neocuspidization for treatment of aortic valve diseases. Ann Thorac Surg p 1–10
Amir G, Rubinsky B, Kassif Y, Horowitz L, Smolinsky AK, Lavee J (2003) Preservation of myocyte structure and mitochondrial integrity in subzero cryopreservation of mammalian hearts for transplantation using antifreeze proteins–an electron microscopy study. Eur J Cardio-Thoracic Surg 24(2):292–297
Angell WW, Oury JH, Lamberti JJ, Koziol J (1989) Durability of the viable aortic allograft. J Thorac Cardiovasc Surg 98(1):48–56
Anstine LJ, Bobba C, Ghadiali S, Lincoln J (2016) Growth and maturation of heart valves leads to changes in endothelial cell distribution, impaired function, decreased metabolism and reduced cell proliferation. J Mol Cell Cardiol 100:72–82
Ayoub S, Ferrari G, Gorman RC, Gorman JH, Schoen FJ, Sacks MS (2017) Heart valve biomechanics and underlying mechanobiology. Compr Physiol 176(12):139–148
Balguid A et al (2008) Stress related collagen ultrastructure in human aortic valves-implications for tissue engineering. J Biomech 41(12):2612–2617
Barzilla JE, McKenney AS, Cowan AE, Durst CA, Grande-Allen KJ (2010) Design and validation of a novel splashing bioreactor system for use in mitral valve organ culture. Ann Biomed Eng 38(11):3280–3294
Baskett RJF et al (2003) Human leukocyte antigen-DR and ABO mismatch are associated with accelerated homograft valve failure in children: implications for therapeutic interventions. J Thorac Cardiovasc Surg 126(1):232–238
Baust JM, Van Buskirk R, Baust JG (2000) Cell viability improves following inhibition of cryopreservation-induced apoptosis. Vitr Cell Dev Biol Anim 36(4):262–270
Bertipaglia B et al (2003) Cell characterization of porcine aortic valve and decellularized leaflets repopulated with aortic valve interstitial cells: the VESALIO Project (vitalitate exornatum succedaneum aorticum labore ingenioso obtenibitur). Ann Thorac Surg 75(4):1274–1282
Brockbank K, Lightfoot F, Song Y, Taylor M (2000) Interstitial ice formation in cryopreserved homografts: a possible cause of tissue deterioration and calcification in vivo. J Heart Valve Dis 9(2):200–2006
Brockbank KGM, Wright GJ, Yao H, Greene ED, Chen ZZ, Schenke-Layland K (2011) Allogeneic heart valve storage above the glass transition at −80°C. Ann Thorac Surg 91(6):1829–1835
Brockbank KGM et al (2012) Ice-free cryopreservation of heart valve allografts: better extracellular matrix preservation in vivo and preclinical results. Cell Tissue Bank 13(4):663–671
Brockbank KGM, Chen Z, Greene ED, Campbell LH (2015) Vitrification of heart valve tissues. Methods Mol Biol 1257:399–421
Brockmann J et al (2009) Normothermic perfusion: a new paradigm for organ preservation. Ann Surg 250(1):1–6
Burkert J et al (2008) Cryopreserved semilunar heart valve allografts: leaflet surface damage in scanning electron microscopy. Zentralbl Chir 133:1–7
Burkert J et al (2021) The time has come to extend the expiration limit of cryopreserved allograft heart valves. Cell Tissue Bank 22(2):161–184
Burwell LS, Nadtochiy SM, Brookes PS (2009) Cardioprotection by metabolic shut-down and gradual wake-up. J Mol Cell Cardiol 46(6):804–810
Butchart EG et al (2005) Recommendations for the management of patients after heart valve surgery. Eur Heart J 26(22):2463–2471
Copeland H et al (2020) Donor heart and lung procurement: a consensus statement. J Hear Lung Transplant 39(6):501–517
Crescenzo DG et al (1992) Donor heart valves: Electron microscopic and morphometric assessment of cellular injury induced by warm ischemia. J Thorac Cardiovasc Surg 103(2):253–258
Dainese L et al (2012) Heart valve engineering: decellularized aortic homograft seeded with human cardiac stromal cells. J Heart Valve Dis 21(1):125–134
Demmy TL, Biddle JS, Bennett LE, Walls JT, Schmaltz RA, Curtis JJ (1997) Organ preservation solutions in heart transplantation-patterns of usage and related survival. Transplantation 63(2):262–269
Dohmen PM et al (2006) Is there a possibility for a glutaraldehyde-free porcine heart valve to grow? Eur Surg Res 38(1):54–61
El-Hamamsy I, Yacoub M, Chester A (2009) Neuronal regulation of aortic valve cusps. Curr Vasc Pharmacol 7(1):40–46
Elliott GD, Wang S, Fuller BJ (2017) Cryoprotectants: a review of the actions and applications of cryoprotective solutes that modulate cell recovery from ultra-low temperatures. Cryobiology 76:74–91
Etnel JRG et al (2016) Outcome after aortic valve replacement in children: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 151(1):143-152.e3
Etnel JRG et al (2018) The ross procedure: a systematic review, meta-analysis, and microsimulation. Circ Cardiovasc Qual Outcomes 11(12):e004748
Fabian O et al (2022) Structural integrity and cellular viability of cryopreserved allograft heart valves in right ventricular outflow tract reconstruction: correlation of histopathological changes with donor characteristics and preservation times. Brazilian J Cardiovasc Surg 37:639–647
Fan Q et al (2022) Strong hydration ability of silk fibroin suppresses formation and recrystallization of ice crystals during cryopreservation. Biomacromol 23(2):478–486
Farivar RS, Filsoufi F, Adams DH (2003a) Mechanisms of Galα1-3Galβ1-4GlcNAc-R (αGal) expression on porcine valve endothelial cells. J Thorac Cardiovasc Surg 125(2):306–314
Farivar RS, Cohn LH, Soltesz EG, Mihaljevic T, Rawn JD, Byrne JG (2003b) Transcriptional profiling and growth kinetics of endothelium reveals differences between cells derived from porcine aorta versus aortic valve. Eur J Cardio-Thoracic Surg 24(4):527–534
Fleck TPK et al (2021) Ex vivo allograft perfusion for complex pediatric heart transplant recipients. Ann Thorac Surg 112(4):1275–1280
Gerson CJ, Goldstein S, Heacox AE (2009) Retained structural integrity of collagen and elastin within cryopreserved human heart valve tissue as detected by two-photon laser scanning confocal microscopy. Cryobiology 59(2):171–179
Ha SJ et al (2016) Effect of antioxidants and apoptosis inhibitors on cryopreservation of murine germ cells enriched for spermatogonial stem cells. PLoS ONE 11(8):1–16
Hammer PE, Roberts EG, Emani SM, del Nido PJ (2017) Surgical reconstruction of semilunar valves in the growing child: should we mimic the venous valve? a simulation study. J Thorac Cardiovasc Surg 153(2):389–396
Hawkins JA et al (2003) Immunogenicity of decellularized cryopreserved allografts in pediatric cardiac surgery: Comparison with standard cryopreserved allografts. J Thorac Cardiovasc Surg 126(1):247–252
Hawkins JA et al (2007) Intermediate-term results of repair for aortic, neoaortic, and truncal valve insufficiency in children. J Thorac Cardiovasc Surg 133(5):1311–1317
Hildebrand DK, Wu ZJ, Mayer JE, Sacks MS (2004) Design and hydrodynamic evaluation of a novel pulsatile bioreactor for biologically active heart valves. Ann Biomed Eng 32(8):1039–1049
Huang HYS, Liao J, Sacks MS (2007) In-situ deformation of the aortic valve interstitial cell nucleus under diastolic loading. J Biomech Eng 129(6):880–889
Hulin A et al (2019) Maturation of heart valve cell populations during postnatal remodeling. Dev 146(12):1–12
Jashari R (2021) Transplantation of cryopreserved human heart valves in Europe: 30 years of banking in Brussels and future perspectives. Cell Tissue Bank 22(4):519–537
Johnson DL, Rose ML, Yacoub MH (1997) Immunogenicity of human heart valve endothelial cells and fibroblasts. Transplant Proc 29(1–2):984–985
Junnil P et al (2021) Long-term course after pediatric right ventricular outflow tract reconstruction. Asian Cardiovasc Thorac Ann 29(6):483–489
Kodigepalli KM et al (2020) Biology and biomechanics of the heart valve extracellular matrix. J Cardiovasc Dev Dis 7(4):1–22
Konduri S, Xing Y, Warnock JN, He Z, Yoganathan AP (2005) Normal physiological conditions maintain the biological characteristics of porcine aortic heart valves: an ex vivo organ culture study. Ann Biomed Eng 33(9):1158–1166
Koolbergen DR et al (1998) Tissue chimerism in human cryopreserved homograft valve explants demonstrated by in situ hybridization. Ann Thorac Surg 66(6):225–232
Koolbergen DR et al (2002) The pathology of fresh and cryopreserved homograft heart valves: an analysis of forty explanted homograft valves. J Thorac Cardiovasc Surg 124(4):689–697
Krs O, Slížová D, Burkert J, Špatenka J, Hottmar P (2004) Impact of processing on surface structure of human cardiac valve allografts. Acta Medica Cordoba 47(2):97–99
Lang SJ, Giordano MS, Cardon-Cardo C, Summers BD, Stalano-Coico L, Hajjar DP (1994) Biochemical and cellular characterization of cardiac valve tissue after cryopreservation or antibiotic preservation. J Thorac Cardiovasc Surg 108(1):63–67
Lesnefsky EJ, Chen Q, Moghaddas S, Hassan MO, Tandler B, Hoppel CL (2004) Blockade of electron transport during ischemia protects cardiac mitochondria. J Biol Chem 279(46):47961–47967
Lisy M, Kalender G, Schenke-Layland K, Brockbank KGM, Biermann A, Stock UA (2017) Allograft heart valves: current aspects and future applications. Biopreserv Biobank 15(2):148–157
Lupinetti FM et al (1999) Intermediate-term results in pediatric aortic valve replacement. Ann Thorac Surg 68(2):521–525
Lupinetti FM et al (2003) Comparison of autograft and allograft aortic valve replacement in children. J Thorac Cardiovasc Surg 126(1):240–245
Marron K et al (1996) Innervation of human atrioventricular and arterial valves.pdf. Circulation 94:368–375
McAnulty JF, Reid TW, Waller KR, Murphy CJ (2002) Successful six-day kidney preservation using trophic factor supplemented media and simple cold storage. Am J Transplant 2(8):712–718
McCoy CM, Nicholas DQ, Masters KS (2012) Sex-related differences in gene expression by porcine aortic valvular interstitial cells. PLoS ONE 7:e39980
Mendelson K, Schoen FJ (2006) Heart valve tissue engineering: concepts, approaches, progress, and challenges. Ann Biomed Eng 34(12):1799–1819
Messier RH et al (1992) High energy phosphate depletion in leaflet matrix cells during processing of cryopreserved cardiac valves. J Surg Res 52(5):483–488
Mirabet V et al (2008) Long-term storage in liquid nitrogen does not affect cell viability in cardiac valve allografts. Cryobiology 57(2):113–121
Mitchell RN, Jonas RA, Schoen FJ (1998) Pathology of explanted cryopreserved allograft heart valves: comparison with aortic valves from orthotopic heart transplants. J Thorac Cardiovasc Surg 115(1):118–127
Motta SE et al (2020) Geometry influences inflammatory host cell response and remodeling in tissue-engineered heart valves in-vivo. Sci Rep 10(1):1–14
Mrsic Z, Hopkins SP, Antevil JL, Mullenix PS (2018) Valvular Heart Disease. Prim Care Clin off Pract 45(1):81–94
Mylotte D et al (2013) Transcatheter aortic valve replacement in Europe: adoption trends and factors influencing device utilization. J Am Coll Cardiol 62(3):210–219
Nappi F et al (2018) Long-term outcome of cryopreserved allograft for aortic valve replacement. J Thorac Cardiovasc Surg 156(4):1357-1365.e6
Neumann A, Cebotari S, Tudorache I, Haverich A, Sarikouch S (2013) Heart valve engineering: decellularized allograft matrices in clinical practice. Biomed Tech 58(5):453–456
Niwaya K, Sakaguchi H, Kawachi K, Kitamura S (1995) Effect of warm ischemia and cryopreservation on cell viability of human allograft valves. Ann Thorac Surg 60(2):S114–S117
O’Brien MF, Stafford EG, Gardner MAH, Pohlner PG, McGiffin DC (1987) A comparison of aortic valve replacement with viable cryopreserved and fresh allograft valves, with a note on chromosomal studies. J Thorac Cardiovasc Surg 94(6):812–823
O’Brien MF et al (1991) Allograft aortic valve replacement: long-term comparative clinical analysis of the viable cryopreserved and antibiotic 4°C stored valves. J Card Surg 6(4 SUPPL.):534–543
O’Brien MF et al (1995) Allograft aortic valve replacement: long-term follow-up. Ann Thorac Surg 60(2):S65–S70
O’Brien M et al (2001) The homograft aortic valve: a 29-year, 99.3% follow up of 1,022 valve replacements. J Heart Valve Dis 10(3):334–344
O’Donnell A, Yutz KE (2020) Mechanisms of heart valve development and disease. Development 147(13):183020
O’Neill S et al (2020) Novel organ perfusion and preservation strategies in transplantation-where are we going in the united kingdom? Transplantation 104(9):1813–1824
Odim J, Laks H, Allada V, Child J, Wilson S, Gjertson D (2005) Results of aortic valve-sparing and restoration with autologous pericardial leaflet extensions in congenital heart disease. Ann Thorac Surg 80(2):647–654
Olijve LLC et al (2016) Blocking rapid ice crystal growth through nonbasal plane adsorption of antifreeze proteins. Proc Natl Acad Sci U S A 113(14):3740–3745
Ostrózka-Cieślik A, Dolińska B (2020) The role of hormones and trophic factors as components of preservation solutions in protection of renal function before transplantation: A review of the literature Molecules 25(9)
Pant AD, Thomas VS, Black AL, Verba T, Lesicko JG, Amini R (2018) Pressure-induced microstructural changes in porcine tricuspid valve leaflets. Acta Biomater 67:248–258
Pegg DE (2020) The relevance of ice crystal formation for the cryopreservation of tissues and organs. Cryobiology 93:3–11
Pfitzner R et al (2018) Influence of cryopreservation on structural, chemical, and immunoenzymatic properties of aortic valve allografts. Transplant Proc 50(7):2195–2198
Rabkin-Aikawa E, Farber M, Aikawa M, Schoen FJ (2004a) Dynamic and reversible changes of interstitial cell phenotype during remodeling of cardiac valves. J Heart Valve Dis 13(5):841–847
Rabkin-Aikawa E et al (2004b) Clinical pulmonary autograft valves: pathologic evidence of adaptive remodeling in the aortic site. J Thorac Cardiovasc Surg 128(4):552–561
Rajani B, Mee RB, Ratliff NB (1998) Evidence for rejection of homograft cardiac valves in infants. J Thorac Cardiovasc Surg 115(1):111–117
Rubinsky B, Arav A, Hong JS, Lee CY (1994) Freezing of mammalian livers with glycerol and antifreeze proteins. Biochem Biophys Res Commun 200(2):732–741
Sanders B et al (2016) Improved geometry of decellularized tissue engineered heart valves to prevent leaflet retraction. Ann Biomed Eng 44(4):1061–1071
Schenke-Layland K et al (2006) Impact of cryopreservation on extracellular matrix structures of heart valve leaflets. Ann Thorac Surg 81(3):918–926
Schenke-Layland K et al (2007) Optimized preservation of extracellular matrix in cardiac tissues: implications for long-term graft durability. Ann Thorac Surg 83:1641–1650
Schoen FJ (2008) Evolving concepts of cardiac valve dynamics: the continuum of development, functional structure, pathobiology, and tissue engineering. Circulation 118(18):1864–1880
Schoen FJ (2011) Heart valve tissue engineering: quo vadis? Curr Opin Biotechnol 22(5):698–705
Shaddy RE, Hawkins JA (2002) Immunology and failure of valved allografts in children. Ann Thorac Surg 74(4):1271–1275
Shaddy RE et al (1996) Prospective analysis of HLA immunogenicity of cryopreserved valved allografts used in pediatric heart surgery. Circulation 94(5):1063–1067
Shaw TB et al (2020) Does pediatric heart transplant survival differ with various cardiac preservation solutions? Clin Transplant 34(12):1–7
Simon A, Wilhelmi M, Steinhoff G, Harringer W, Brucke P, Haverich A (1998) Cardiac valve endothelial cells: Relevance in the long-term function of biologic valve prostheses. J Thorac Cardiovasc Surg 116(4):609–616
Simon P et al (2003) Early failure of the tissue engineered porcine heart valve SYNERGRAFT™ in pediatric patients. Eur J Cardio-Thoracic Surg 23(6):1002–1006
Siregar S et al (2014) Trends and outcomes of valve surgery: 16-year results of Netherlands cardiac surgery national database. Eur J Cardio-Thoracic Surg 46(3):386–397
Smith JD, Ogino H, Hunt D, Laylor RM, Rose ML, Yacoub MH (1995) Humoral immune response to human aortic valve homografts. Ann Thorac Surg 60(2):S127–S130
Song YC, Khirabadi BS, Lightfoot F, Brockbank KGM, Taylor MJ (2000) Vitreous cryopreservation maintains the function of vascular grafts. Nat Biotechnol 18(3):296–299
Stassen OMJA, Muylaert DEP, Bouten CVC, Hjortnaes J (2017) Current challenges in translating tissue-engineered heart valves. Curr Treat Options Cardiovasc Med 19(9):1–13
Takahashi M et al (2021) Strategies to prolong homeostasis of ex vivo perfused lungs. J Thorac Cardiovasc Surg 161(6):1963–1973
Takkenberg JJM, Van Herwerden LA, Eijkemans MJC, Bekkers JA, Bogers AJJC (2002) Evolution of allograft aortic valve replacement over 13 years: results of 275 procedures. Eur J Cardio-Thoracic Surg 21(4):683–691
Takkenberg JJM, Kappetein AP, Van Herwerden LA, Witsenburg M, Van Osch-Gevers L, Bogers JJC (2005) Pediatric autograft aortic root replacement: a prospective follow-up study. Ann Thorac Surg 80(5):1628–1633
Tas RP, Sampaio-Pinto V, Wennekes T, Laake LW, Voets IK (2021) From the freezer to the clinic. EMBO Rep 22(3):1–7
Taylor MJ, Weegman BP, Baicu SC, Giwa SE (2019) New approaches to cryopreservation of cells, tissues, and organs. Transfus Med Hemotherapy 46(3):197–215
van den Heever JJ et al (2021) Comparison of the function and structural integrity of cryopreserved pulmonary homografts versus decellularized pulmonary homografts after 180 days implantation in the juvenile ovine model. Cell Tissue Bank 23(2):347–366
van der Kamp AWM, Visser WJ, van Dongen JM, Nauta J, Galjaard H (1981) Preservation of aortic heart valves with maintenance of cell viability. J Surg Res 30(1):47–56
van der Valk DC et al (2018) Engineering a 3d-bioprinted model of human heart valve disease using nanoindentation-based biomechanics. Nanomaterials 8(5):1–21
Van Geemen D et al (2016) Age-dependent changes in geometry, tissue composition and mechanical properties of fetal to adult cryopreserved human heart valves. PLoS ONE 11(2):e0149020
VeDepo MC, Detamore MS, Hopkins RA, Converse GL (2017) Recellularization of decellularized heart valves: Progress toward the tissue-engineered heart valve. J Tissue Eng 8
Voets IK (2017) From ice-binding proteins to bio-inspired antifreeze materials. Soft Matter 13(28):4808–4823
Wang T, Zhu Q, Yang X, Layne JR, Devries AL (1994) Antifreeze glycoproteins from antarctic notothenioid fishes fail to protect the rat cardiac explant during hypothermic and freezing preservation. Cryobiology 31(2):185–192
Wang H, Tibbitt MW, Langer SJ, Leinwand LA, Anseth KS (2013) Hydrogels preserve native phenotypes of valvular fibroblasts through an elasticity-regulated PI3K/AKT pathway. Proc Natl Acad Sci U S A 110(48):19336–19341
Waqanivavalagi SWFR, Bhat S, Ground MB, Milsom PF, Cornish J (2020) Clinical performance of decellularized heart valves versus standard tissue conduits: a systematic review and meta-analysis. J Cardiothorac Surg 15(1):1–13
Welters MJP, Oei FBS, Vaessen LMB, Stegmann APA, Bogers AJJC, Weimar W (2001) Increased numbers of circulating donor-specific T helper lymphocytes after human heart valve transplantation. Clin Exp Immunol 124(3):353–358
Witten JC et al (2021) Performance and durability of cryopreserved allograft aortic valve replacements. Ann Thorac Surg 111(6):1893–1900
Yankah AC et al (1987) Transplantation of aortic and pulmonary allografts, enhanced viability of endothelial cells by cryopreservation, importance of histocompatibility. J Card Surg 2(1 Suppl):209–220
Yap CH, Yii M (2004) Factors influencing late allograft valve failure. Scand Cardiovasc J 38(6):325–333
Zhang JM, Li LX, Yang YX, Liu XL, Wan XP (2009) Is caspase inhibition a valid therapeutic strategy in cryopreservation of ovarian tissue? J Assist Reprod Genet 26(7):415–420
Acknowledgements
Not applicable
Funding
M.C.P. is supported by the research grant of Hartekind as part of the OUTREACH Netherlands Heart Institute grant.
Author information
Authors and Affiliations
Contributions
MCP designed the work, performed data analysis and interpretation, prepared the figures and the tables and wrote the manuscript. BPTK and CVCB contributed to article design and article revision. IKV and AvdB revised the article. MJG contributed to design of the article and revision of article. AvW contributed to conception and design of the work, revision of article, and provided financial support. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethics approval
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peters, M.C., Kruithof, B.P.T., Bouten, C.V.C. et al. Preservation of human heart valves for replacement in children with heart valve disease: past, present and future. Cell Tissue Bank 25, 67–85 (2024). https://doi.org/10.1007/s10561-023-10076-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-023-10076-2