Abstract
Background
Nasal glucagon (NG) 3 mg is approved in Japan to treat hypoglycemia in pediatric patients with diabetes, but an NG clinical study has not been performed in Japanese children because of practical and ethical concerns.
Objective
The aim of this study is to support the dose rationale for NG 3 mg in Japanese pediatric patients with diabetes using modeling and simulation.
Methods
We used a pharmacokinetic/pharmacodynamic bridging approach to extrapolate the available clinical data to Japanese pediatric patients. Population pharmacokinetic/pharmacodynamic modeling was performed using data from seven clinical studies, including five studies in non-Japanese adults, one study in Japanese adults, and one study in non-Japanese pediatric patients. Simulation was then used to estimate glucagon exposure and glucose response after NG 3-mg administration for three age categories of Japanese pediatric patients: 4 to < 8, 8 to < 12, and 12 to < 18 years. Treatment success was defined as an increase in blood glucose to ≥ 70 or ≥ 20 mg/dL from nadir within 30 min after administration of NG 3 mg. Safety was assessed in relation to the predicted maximum glucagon concentration of NG 3 mg using NG clinical trial data and published data on intravenous and intramuscular glucagon.
Results
The data showed a rapid and robust glucose response following NG 3 mg in Japanese and non-Japanese adults and non-Japanese pediatric patients, with some differences in glucagon exposure observed across studies. The pharmacokinetic/pharmacodynamic model described the observed clinical data well, and simulations indicated that > 99% of hypoglycemic Japanese pediatric patients in all three age groups would achieve treatment success. Predicted glucose responses to NG 3 mg in Japanese pediatric patients were comparable to those of intramuscular glucagon. Maximum concentration was not associated with the occurrence and severity of common adverse events (nausea, vomiting, and headache) in NG clinical studies. Furthermore, the predicted maximum concentration in Japanese pediatric patients, despite being higher than the observed maximum concentration in NG clinical studies, was substantially lower than the observed maximum concentration of 1 mg of intravenous glucagon, without serious safety issues.
Conclusions
This analysis suggests NG 3 mg has robust efficacy without serious safety concerns in Japanese pediatric patients with diabetes.
Similar content being viewed by others
Nasal glucagon (NG) 3 mg is approved in Japan to treat hypoglycemia in pediatric patients with diabetes, but an NG clinical study has not been performed in Japanese children. |
In this paper, we present the dose rationale for NG 3 mg in Japanese pediatric patients, based on prior clinical study data from adult patients and non-Japanese pediatric patients, and evaluate the safety and efficacy of NG 3 mg in Japanese pediatric patients by modeling and simulation of the predicted glucagon exposure/glucose response. |
This analysis suggested robust efficacy for NG 3 mg as rescue treatment for hypoglycemia in Japanese pediatric patients, with no serious safety concerns; regulatory approval has been obtained for NG 3 mg for this use without age restriction in Japan. |
1 Introduction
The incidence of diabetes mellitus is growing in Japan, driven predominantly by an increase in the number of patients with type 2 diabetes (T2D), with approximately 13.5% of the population reported to have T2D or impaired glucose tolerance [1]. Although the incidence is lower in Japanese pediatric patients, the National Diabetes Survey between 1997 and 2007 describes the incidence rate for T2D in children as 6.73 and 0.75 per 100,000 person-years for junior high and elementary school students, respectively [2]. Type 1 diabetes (T1D) has an incidence rate among Japanese children aged 0–19 years of 3.94 (male) to 5.22 (female) per 100,000 person-years [3].
Hypoglycemia is a common complication in the management of T1D and T2D [4, 5]. Severe hypoglycemia, defined as the presence of hypoglycemia symptoms requiring assistance from another person to treat [6], can result in reduced cognitive function, unconsciousness, and seizures if untreated [7]. Children with diabetes are at particular risk from severe hypoglycemia, which is associated with serious neurological complications, such as permanent brain damage, structural abnormalities, and cognitive dysfunction, and is the cause of death in 4–10% of children and adolescents with T1D [8]. The incidence of severe hypoglycemia has declined over recent decades but remains a common complication in children with T1D [9].
Nasal glucagon (NG) is a nasally administered, single-use, drug-device combination containing glucagon dry powder [10]. Nasal glucagon is absorbed from the nasal cavity and does not require reconstitution, injection, or patient inhalation, thereby offering an appealing alternative to injectable glucagon for rescue treatment in patients experiencing severe hypoglycemia. The global clinical development program for NG characterized the efficacy, pharmacokinetics, pharmacodynamics, and safety of NG doses with a range from 0.5 to 6 mg, showing NG 3 mg was efficacious, well tolerated, and non-inferior to intramuscular glucagon (IMG) 1 mg [11,12,13,14,15]. Based on these data, the 3-mg dose was selected for worldwide registration. The real-world effectiveness of NG 3 mg has been demonstrated in two open-label, phase III trials in adults [16] and youths [17] with T1D.
Some differences in patient characteristics, diabetic pathophysiology, and response to glucose-lowering medications have been reported in Japanese adult [18,19,20,21] and pediatric [22,23,24] patient populations compared with non-Japanese populations. Currently, NG has not been clinically studied in Japanese children. While ideally the potential for ethnic or country-specific differences would be explored in pediatric populations in clinical trials during drug development, there are many practical impediments to conducting pediatric clinical trials in Japan, such as limitations on infrastructure, experience, and patient recruitment [25]. The necessary induction of hypoglycemia and procurement of multiple blood samples are added ethical burdens in pediatric populations.
Considering these practical concerns and to reduce the burden on pediatric patients, the current study has used a pharmacokinetic/pharmacodynamic (PK/PD) modeling and simulation approach to investigate the safety and efficacy of NG in Japanese pediatric patients. The primary objective of the current investigation was to evaluate the dose rationale for NG 3 mg in Japanese pediatric patients. In a PK/PD bridging approach, results were first extrapolated from clinical studies on Japanese adult patients and non-Japanese adult and pediatric patients. We then evaluated the efficacy and safety of an NG 3-mg dose in Japanese pediatric patients using a population PK/PD analysis of pooled clinical trial data, building upon prior modeling in non-Japanese patients by the inclusion of clinical trial data from Japanese adults.
2 Methods
Three main elements underpinned the dose rationale and its further assessment: (1) comparison of NG PK/PD data from Japanese and non-Japanese clinical studies; (2) modeling and simulation based on the clinical data to estimate glucagon exposure and glucose response in Japanese pediatric patients following NG 3-mg administration; and (3) assessment of safety in relation to the predicted maximum glucagon concentration (Cmax) of NG 3 mg using NG clinical data and published data on intravenous (IV) and injectable glucagon.
2.1 Comparison of NG 3-mg Pharmacokinetics and Pharmacodynamics Across Studies
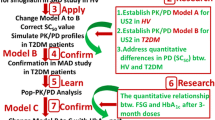
Figure 1 depicts the strategy employed for the assessment of NG clinical trial data used in the Japanese pediatric dose rationale. In brief, four main studies were considered during the dose rationale, including one study of Japanese adult patients, two studies of non-Japanese adult patients, and one study of non-Japanese pediatric patients (Fig. 1). All four studies were of similar design, with hypoglycemia induced by IV insulin administration and treated with either a single dose of NG 3 mg or IMG 1 mg (0.5 mg for body weight < 25 kg) in a crossover design [12,13,14,15] (Table 1). Nasal glucagon 3-mg exposure (pharmacokinetics) and glucose response (pharmacodynamics) were assessed in serial blood samples and based on a change from baseline (pre-dose) in glucagon and glucose concentrations, respectively, which were measured using validated methods [12,13,14,15]. The PK and PD parameters were computed by non-compartmental methods and compared across studies using IMG 1-mg data as the common reference between studies. Comparisons were made between: (1) Japanese and non-Japanese adult patients; (2) commercial and clinical trial products; and (3) non-Japanese adult patients and pediatric patients, as depicted in Fig. 1.
Schematic of nasal glucagon dose rationale for Japanese pediatric patients. The Japanese pediatric dose rationale was extrapolated from four main studies, including three studies in non-Japanese and Japanese adult patients and one study in non-Japanese pediatric patients. In all four studies, experimentally induced hypoglycemia was treated with either a single dose of nasal glucagon 3 mg or intramuscular glucagon 1 mg (0.5 mg for body weight < 25 kg) in a crossover design [12,13,14,15]. NCT clinical trial registration, United States National Library of Medicine; ClinicalTrials.gov
2.2 Development of the PK and PD Models
The PK/PD model development based on data from the global NG clinical development program has been described previously [26]. The global PK/PD model included data from five clinical studies in non-Japanese adults (including the global pivotal adult study and clinical bridging and confirmatory study with the commercial product) and one clinical study in non-Japanese pediatric patients. The current study used a similar strategy for model development as James et al. [26] but based the model on data from the six studies in the original model plus the pivotal Japanese adult study (Table 1). In brief, population PK/PD modeling was performed using a nonlinear mixed-effects modeling program (NONMEM) Version 7.4.2 (ICON Development Solutions, Hanover, MD) [27]. A sequential modeling approach was used for the development of the PK/PD model, which was followed by a model evaluation consistent with best practices, as detailed in the Electronic Supplementary Material (ESM). For the PK model, a one-compartment model was used to describe the glucagon concentration data. A base model was first constructed and evaluated via a bootstrap analysis, visual predictive checks [28], and goodness-of-fit plots. Next, potential covariates were assessed for their impact on PK parameters and were incorporated into the full model based on forward selection and backward deletion strategies (ESM). The same model development and validation processes used for pharmacokinetics were adopted for the PD model (ESM).
2.3 Simulations Based on Models
The final population PK and PD models characterizing NG exposure and response in non-Japanese children and Japanese adults were used to simulate glucagon exposure and plasma glucose response in Japanese pediatric patients administered NG 3 mg and IMG 1 mg (0.5 mg for body weight < 25 kg). Plasma glucose profiles for NG 3 mg in Japanese pediatric patients were predicted from 1000 patients for each of three age categories: 4 to < 8, 8 to < 12, and 12 to < 18 years, including all sources of variability in the models. Simulations were performed using R (RxODE). Glucagon exposure and blood glucose response were simulated for patients administered NG 3 mg and various glucose baseline values to evaluate whether the 3-mg adult dose is applicable to pediatric patients. Treatment success criteria were derived from a randomized crossover non-inferiority trial comparing NG 3 mg to IMG (1 mg) in adults with T1D [13]. Treatment success was defined as blood glucose increased to ≥ 70 or by ≥ 20 mg/dL from the plasma glucose nadir within 30 min of receiving glucagon, with no further interventions to raise blood glucose levels. The treatment success criteria are in accordance with the treatment goal to either achieve normoglycemia or raise blood glucose to a level above which the recovery of cognitive function would allow further treatment with oral carbohydrates [13]. The simulation was performed under the following assumptions:
-
(1)
the PK difference between Japanese adults and children is mainly caused by their body weight difference;
-
(2)
the PD response characterized in non-Japanese children (Study 4, Table 1) is translatable to Japanese children;
-
(3)
the PD response in adult Japanese patients (Study 7, Table 1) is translatable to Japanese children. Body weight distributions in ages 4 to < 18 years were based on “The National Health and Nutrition Survey in Japan, 2017” [29].
2.4 Safety Analysis
An exploratory assessment of the impact of Cmax on the safety and tolerability of NG was conducted in adult and pediatric patients enrolled in NG clinical studies. Common adverse events (nausea, vomiting, and headache) reported in NG clinical studies were tabulated, and event frequency and severity against Cmax were summarized in box plots. Median Cmax for glucagon was calculated with the 5th and 95th percentiles. In addition, the published data of injectable and IV glucagon were used to evaluate the impact of the predicted high glucagon exposure, outside the NG clinical trial program, on safety in pediatric patients [30,31,32,33].
3 Results
3.1 Comparison of PK and PD Data from NG Clinical Studies
Following administration of the NG 3-mg commercial drug product, rapid absorption and elimination of the study drug were observed in Japanese adult patients with T1D and T2D (ESM). The peak of plasma glucagon was greater after NG 3 mg than after IMG 1 mg, whereas NG 3 mg produced a similar glucose response to IMG 1 mg for the first 60 min post-dose. Comparison of Japanese and non-Japanese adult patients receiving the commercial NG 3-mg product showed Japanese adults had higher glucagon exposure (Cmax = 9520 pg/mL) compared with non-Japanese adults (Cmax = 6130 pg/mL), whereas there were no clear ethnic differences in glucose response (Japanese: blood glucose (BG)max = 165 mg/dL; ΔBGmax = 113 mg/dL; non-Japanese: BGmax = 192 mg/dL; ΔBGmax = 132 mg/dL). Glucagon exposure parameters following IMG 1 mg were comparable between these two study populations (ESM). Product formulation comparisons in non-Japanese adults showed that while glucose response was similar between commercial and clinical trial products, the exposure with the commercial product (Cmax = 6130 pg/mL) was higher than with the clinical trial product (Cmax = 3130 pg/mL). Furthermore, a higher glucagon Cmax was observed for NG 3 mg relative to IMG 1 mg in non-Japanese adults receiving a commercial product whereas a lower glucagon Cmax was observed for NG 3 mg compared to IMG 1 mg in non-Japanese adults receiving the clinical trial product (ESM). Of those who received the clinical trial product, PK and PD parameters in non-Japanese pediatric patients were similar to those in non-Japanese adults. In each age group (4 to < 8, 8 to < 12, and 12 to < 17 years), NG 3 mg rapidly produced a maximal blood glucose increase, similar to that of weight-based IMG doses (0.5 or 1 mg; ESM).
3.2 PK and PD Modeling Results
The population PK/PD dataset included 8076 glucagon and 8950 glucose concentrations collected from 337 patients in the seven studies listed in Table 1. Patient demographics are shown in the ESM.
For the final base PK model, standard allometric scaling exponents were applied to clearance and volume. The final base model included estimated relative bioavailability of NG to IMG/subcutaneous glucagon, rate of absorption, clearance, volume of distribution, and baseline glucagon concentration and a proportional residual error term. A small time lag (estimated to be approximately 4 min) was incorporated in NG absorption to account for the delay compared with absorption of injectable glucagon. Inter-occasion variability was also incorporated on absorption and bioavailability. After applying the body weight effect on clearance and volume, no other factors were identified as significant covariates on absorption and bioavailability.
Overall, the study in Japanese adults (Study 7) found a similar absorption rate and 28% higher relative bioavailability to injectable glucagon as compared to those of the global clinical bridging study (Study 6). In studies that utilized the commercial drug product (Studies 6 and 7) or a clinical trial drug product with similar formulation to the commercial product (Study 3), bioavailability was higher (relative bioavailability = 27% in Studies 3 and 6; 55% in Study 7) relative to injectable glucagon as compared to studies with the clinical trial drug product (relative bioavailability = 15%).
For PD modeling, an indirect response model was used to describe the relationship between glucagon plasma concentration (Cg) and changes in glucose (Glu), where Kin and Kout,t were the production rate and elimination rate of Glu, respectively (Eq 1):
Based on the known pharmacology of glucagon, it was assumed Cg increases Kin. Emax (stimulation maximum) is the maximum effect that glucagon can achieve upon Kin whereas EC50 is the Cg that results in a 50% Emax increase of Kin.
Insulin was administered to patients to lower blood glucose prior to administration of glucagon. To account empirically for carryover of the insulin effect in the absence of insulin PK measurements, an exponential reduction of this effect on glucose Kout was implemented (Eq. 2):
where Kout,t is the elimination rate constant of glucose at time, t; Kout,ss is the (steady-state) elimination rate constant in the absence of insulin induction; k is the rate of decay of the insulin effect (Inseff, which refers to the carryover of insulin effect from prior insulin administration to lower blood glucose before glucagon treatment); and t is time after the glucagon dose. For the final PK and PD models, goodness-of-fit plots show that the models fit the data well (ESM).
3.3 Simulation Results for Japanese Pediatric Patients
Figure 2 shows the simulated time course from 0 to 90 min post-dose for glucagon exposure and glucose response in Japanese pediatric patients with a median baseline blood glucose of 40 mg/dL. Predicted maximum blood glucose levels across the three age groups were similar between NG 3 mg and IMG (BGmax: NG 3 mg, approximately 170–180 mg/dL; IMG [weight-based dosing], 166–176 mg/dL; ESM) and within the range of observed values from NG clinical studies (ESM). Simulations indicated > 99% of hypoglycemic Japanese pediatric patients in all three age groups would achieve treatment success within 30 min after administration of NG 3 mg (Table 2). However, in all pediatric age categories, the predicted Cmax and area under the concentration curve from time 0 to 1.5 h were much higher for NG 3 mg (Cmax: 4 to < 8 years: 28,900 pg/mL; 8 to < 12 years: 20,500 pg/mL; 12 to < 18 years: 14,100 pg/mL) than for IMG (Cmax: 4 to < 8 years: 5160 pg/mL; 8 to < 12 years: 6240 pg/mL; 12 to < 18 years: 4660 pg/mL; ESM). Predicted exposure data for NG 3 mg in Japanese pediatric patients were higher than the observed data from NG clinical studies in Japanese adult patients and non-Japanese adult and pediatric patients (ESM).
Plots of median glucagon exposure and glucose response over time by pediatric age category. Simulation results are shown for Japanese patients a 4 to < 8 years of age; b 8 to < 12 years of age; and c 12 to < 18 years of age. Predicted median glucagon exposure (top panel) and glucose response (bottom panel) over time are shown for nasal glucagon (NG) 3 mg (red) and intramuscular glucagon (IMG) [0.5 or 1.0 mg, based on body weight; blue] at baseline of 40 mg/dL with a commercially representative drug product. min minutes
3.4 Safety
Given the higher predicted Cmax values for NG 3 mg than IMG in all pediatric age categories (Fig. 2), the impact of glucagon exposure on safety after NG 3 mg was explored. Figure 3 shows the predicted mean glucagon exposure over time for NG 3 mg in Japanese pediatric patients relative to published values for IV glucagon [31]. For each of the age categories, the predicted Cmax in Japanese pediatric patients was substantially lower (< 1/5) than that observed following either 0.5 or 1 mg IV glucagon (Fig. 3). The clinical literature for injectable and IV glucagon shows IV dosing has an acceptable safety profile, similar to other routes of glucagon administration [30,31,32,33].
Predicted mean glucagon exposure over time for nasal glucagon (NG) 3 mg in pediatric Japanese patients. Simulation results are shown by age group of patients treated with NG 3 mg (commercially representative drug product). Dashed lines indicate mean maximum concentration (Cmax) of 0.5 and 1.0 mg intravenous (IV) glucagon, respectively. Data from reference [31]. min minutes
Safety in Japanese pediatric patients following administration of NG 3 mg was further investigated by examining the relationship between Cmax and adverse events in the NG clinical studies. No association between glucagon Cmax and common adverse events, such as nausea, vomiting, and headache, was apparent in Japanese adult patients after NG 3 mg (Fig. 4). Safety data from other NG clinical studies also revealed that the predicted Cmax was not associated with the frequency or severity of common adverse events (data not shown). Notably, there were no specific safety concerns in non-Japanese pediatric patients after administration of NG 3 mg [14].
Box plots of glucagon maximum concentration (Cmax) versus adverse event severity. a Nausea, b vomiting, and c headache in adult Japanese patients treated with nasal glucagon 3 mg. Data from Reference [12]
4 Discussion
In this paper, we have presented the dose rationale for Japanese pediatric patients. The PK/PD bridging analysis of published NG clinical studies established that a single dose of NG 3 mg produces a rapid and robust glucose response, similar to that of IMG 1 mg. No clear differences in glucose response and efficacy were found between Japanese and non-Japanese adult patients although Japanese patients had higher glucagon exposure following the commercial NG 3-mg product compared with non-Japanese patients. Similarly, while glucose response and efficacy results were comparable between both the clinical trial and commercial product formulations, a higher Cmax was observed for the commercial product.
Glucose response and efficacy were similar between NG 3 mg and IMG 1 mg in Japanese adult and non-Japanese adult and pediatric patients. The NG clinical data also indicate NG is well tolerated and has similar safety profiles to IMG, although a higher proportion of patients receiving NG experienced nasal and ocular adverse events, which were considered related to the administration route [12,13,14,15]. Collectively, the NG clinical data from Japanese adult, non-Japanese adult, and non-Japanese pediatric studies indicate NG 3 mg results in treatment success that is similar to IMG in hypoglycemic patients with diabetes, with no significant safety concerns [12,13,14,15]. However, it should be noted that some variability in glucagon exposure was observed during the NG clinical trial development program. Notably, Studies 3, 6, and 7 had higher Cmax after NG 3-mg administration compared with the other studies, which may be attributed to differences in product formulation. Additionally, product formulation was re-optimized for the commercial product following the original development for the clinical trial product, which may have contributed to higher inter-study PK variability. Finally, variable deposition and absorption are well-recognized issues for the PK assessment of nasally administered drugs [34], and differences in nasal absorption bioavailability may account for some of the variability in PK data noted between studies using the same drug product formulation (e.g., Studies 6 and 7) and for the higher variability in Cmax of NG relative to injectable glucagon, which was observed in many of the studies.
In light of the variability in glucagon exposure among studies, safety and efficacy in Japanese pediatric patients were further evaluated by modeling and simulation of the predicted glucagon exposure/glucose response. The PK/PD simulations showed the predicted plasma glucose profiles for NG 3 mg in Japanese pediatric patients were comparable to IMG 0.5 or 1 mg in all age groups. However, the predicted Cmax of NG 3 mg in Japanese pediatric patients was high compared to that of IMG and higher than the observed concentrations in the NG clinical development program. A literature search revealed that the predicted Cmax for NG 3 mg in Japanese pediatric patients, although substantially higher than the predicted Cmax for IMG 1 mg (ESM), was substantially lower than the observed Cmax of 0.5 and 1 mg IV glucagon in a previous study [31]. Further investigation of the safety and tolerability of higher glucagon exposure in the NG clinical studies suggests no trend to increase the incidence, severity, or types of adverse events observed in NG-treated patients with glucagon Cmax. This finding is supported by Study 7, conducted in Japanese adults, wherein treatment-emergent adverse events other than administration route were comparable between IMG and NG, although NG had a higher Cmax than IMG. These assessments suggest there are no significant safety concerns in Japanese pediatric patients with potentially higher exposure following NG 3-mg administration.
Hypoglycemia is one of the most frequent acute complications of diabetes in patients treated with insulin and/or anti-diabetic drugs and, when severe, can lead to life-threatening disorders [4, 5]. The goal of glucagon rescue treatment for hypoglycemia is to restore blood glucose rapidly to the level where a patient whose life is threatened by severe hypoglycemia regains sufficient cognitive function to ingest carbohydrates safely. Therefore, a potential treatment for severe hypoglycemia must produce a rapid and robust glucose response in patients while being safe and tolerated. Of relevance to this, the final PK/PD models predicted that, in hypoglycemic pediatric patients aged 4 to < 18 years with baseline glucose of 40 mg/dL, more than 99% of patients would experience treatment success within 30 min of NG 3-mg administration. Collectively, the current modeling and simulation data support the safe and effective use of NG 3 mg in Japanese pediatric patients.
Although its efficacy is well established as a rescue treatment for severe hypoglycemia, glucagon is both under-prescribed by pediatricians and physicians [35] and under-utilized by patients [36] in Japan. Recent studies in Japan and elsewhere suggest the major barrier to wider usage is that injectable glucagon requires multiple steps to prepare and administer. Notably, over two-thirds of parents of pediatric patients with diabetes had difficulty administering injectable glucagon in a simulated administration study [37]. Further, simulated administration of NG and IMG by caregivers and untrained third parties in Japan showed both the speed and accuracy of administration were significantly greater with NG than IMG, with the majority of participants reporting the NG device was easier to use [38]. Thus, the ready-to-use formulation and ease of administration of NG offer major advantages over injectable glucagon, particularly for the treatment of severe hypoglycemia in pediatric patients.
As an NG pediatric trial is not feasible in Japan, the PK/PD bridging approach used in the current study enabled evaluation of the safety and efficacy of NG 3 mg in Japanese pediatric patients based on modeling of the available clinical trial data to support our NG 3-mg dose rationale. However, our study has limitations that should be considered when interpreting the results. First, only one clinical study on NG 3 mg in pediatric patients has been completed, which was conducted on a limited number of non-Japanese patients and used the product formulated for clinical trial, not commercial use. Given the inter-study variability in PK data, Japanese pediatric data are still desirable to rule out potential ethnic differences in efficacy and safety in pediatric patients, although the likelihood of any differences is low. Additionally, with only one available pediatric study, we could not validate the model with an external dataset. Second, NG-treated patients had more adverse events that were considered administration route related, and these were not evaluated in the model. Ideally, we would have evaluated spontaneous events following NG 3-mg treatment in Japanese pediatric patients in real-world circumstances, but this was not feasible given the extended period needed to collect sufficient spontaneous event data. Accumulation of such real-world evidence is expected in the future.
5 Conclusions
Although our PK/PD bridging approach with modeling and simulation suggests Japanese pediatric patients may have higher glucagon exposure following NG 3-mg administration, the data collectively support a rapid and robust glucose response after NG 3 mg with acceptable safety and tolerability. Thus, we conclude NG 3 mg is appropriate as a rescue treatment for hypoglycemia for both Japanese adult and pediatric patients.
References
Neville SE, Boye KS, Montgomery WS, Iwamoto K, Okamura M, Hayes RP. Diabetes in Japan: a review of disease burden and approaches to treatment. Diabetes Metab Res Rev. 2009;25:705–16. https://doi.org/10.1002/dmrr.1012.
Morimoto A, Nishimura R, Tajima N. Trends in the epidemiology of patients with diabetes in Japan. JMAJ. 2010;53:36–40.
Nishioka Y, Noda T, Okada S, Myojin T, Kubo S, Higashino T, et al. Incidence and seasonality of type 1 diabetes: a population-based 3-year cohort study using the national database in Japan. BMJ Open Diabetes Res Care. 2020;8: e001262. https://doi.org/10.1136/bmjdrc-2020-001262.
Kedia N. Treatment of severe diabetic hypoglycemia with glucagon: an underutilized therapeutic approach. Diabetes Metab Syndr Obes. 2011;4:337–46. https://doi.org/10.2147/DMSO.S20633.
Shafiee G, Mohajeri-Tehrani M, Pajouhi M, Larijani B. The importance of hypoglycemia in diabetic patients. J Diabetes Metab Disord. 2012;11:17. https://doi.org/10.1186/2251-6581-11-17.
Namba M, Iwakura T, Nishimura R, Akazawa K, Matsuhisa M, Atsumi Y, et al. The current status of treatment-related severe hypoglycemia in Japanese patients with diabetes mellitus: a report from the committee on a survey of severe hypoglycemia in the Japan Diabetes Society. J Diabetes Investig. 2018;9:64256. https://doi.org/10.1111/jdi.12790.
Villani M, de Courten B, Zoungas S. Emergency treatment of hypoglycaemia: a guideline and evidence review. Diabet Med. 2017;34:1205–11. https://doi.org/10.1111/dme.13379.
Urakami T. Severe hypoglycemia: is it still a threat for children and adolescents with type 1 diabetes? Front Endocrinol (Lausanne). 2020;11:609. https://doi.org/10.3389/fendo.2020.00609.
Cherubini V, Rabbone I, Lombardo F, Mossetto G, Orsini Federici M, Nicolucci A. Incidence of severe hypoglycemia and possible associated factors in pediatric patients with type 1 diabetes in the real-life, post-diabetes control and complications trial setting: a systematic review. Pediatr Diabetes. 2019;20:678–92. https://doi.org/10.1111/pedi.12876.
Pontiroli AE. Intranasal glucagon: a promising approach for treatment of severe hypoglycemia. J Diabetes Sci Technol. 2015;9:38–43. https://doi.org/10.1177/1932296814557518.
Guzman CB, Dulude H, Piche C, Rufiange M, Sadoune AA, Rampakakis E, et al. Effects of common cold and concomitant administration of nasal decongestant on the pharmacokinetics and pharmacodynamics of nasal glucagon in otherwise healthy participants: a randomized clinical trial. Diabetes Obes Metab. 2018;20:646–53. https://doi.org/10.1111/dom.13134.
Matsuhisa M, Takita Y, Nasu R, Nagai Y, Ohwaki K, Nagashima H. Nasal glucagon as a viable alternative for treating insulin-induced hypoglycaemia in Japanese patients with type 1 or type 2 diabetes: a phase 3 randomized crossover study. Diabetes Obes Metab. 2020;22:1167–75. https://doi.org/10.1111/dom.14019.
Rickels MR, Ruedy KJ, Foster NC, Piche CA, Dulude H, Sherr JL, et al. Intranasal glucagon for treatment of insulin-induced hypoglycemia in adults with type 1 diabetes: a randomized crossover noninferiority study. Diabetes Care. 2016;39:264–70. https://doi.org/10.2337/dc15-1498.
Sherr JL, Ruedy KJ, Foster NC, Piche CA, Dulude H, Rickels MR, et al. Glucagon nasal powder: a promising alternative to intramuscular glucagon in youth with type 1 diabetes. Diabetes Care. 2016;39:555–62. https://doi.org/10.2337/dc15-1606.
Suico JG, Hovelmann U, Zhang S, Shen T, Bergman B, Sherr J, et al. Glucagon administration by nasal and intramuscular routes in adults with type 1 diabetes during insulin-induced hypoglycaemia: a randomised, open-label, crossover study. Diabetes Ther. 2020;11:1591–603. https://doi.org/10.1007/s13300-020-00845-7.
Seaquist ER, Dulude H, Zhang XM, Rabasa-Lhoret R, Tsoukas GM, Conway JR, et al. Prospective study evaluating the use of nasal glucagon for the treatment of moderate to severe hypoglycaemia in adults with type 1 diabetes in a real-world setting. Diabetes Obes Metab. 2018;20:1316–20. https://doi.org/10.1111/dom.13278.
Deeb LC, Dulude H, Guzman CB, Zhang S, Reiner BJ, Piche CA, et al. A phase 3 multicenter, open-label, prospective study designed to evaluate the effectiveness and ease of use of nasal glucagon in the treatment of moderate and severe hypoglycemia in children and adolescents with type 1 diabetes in the home or school setting. Pediatr Diabetes. 2018;19:1007–13. https://doi.org/10.1111/pedi.12668.
Ikezaki H, Ai M, Schaefer EJ, Otokozawa S, Asztalos BF, Nakajima K, et al. Ethnic differences in glucose homeostasis markers between the Kyushu-Okinawa population study and the Framingham Offspring Study. Sci Rep. 2016;6:36725. https://doi.org/10.1038/srep36725.
Kodama K, Tojjar D, Yamada S, Toda K, Patel CJ, Butte AJ. Ethnic differences in the relationship between insulin sensitivity and insulin response: a systematic review and meta-analysis. Diabetes Care. 2013;36:1789–96. https://doi.org/10.2337/dc12-1235.
Ma RC, Chan JC. Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Ann NY Acad Sci. 2013;1281:64–91. https://doi.org/10.1111/nyas.12098.
Moller JB, Pedersen M, Tanaka H, Ohsugi M, Overgaard RV, Lynge J, et al. Body composition is the main determinant for the difference in type 2 diabetes pathophysiology between Japanese and Caucasians. Diabetes Care. 2014;37:796–804. https://doi.org/10.2337/dc13-0598.
James S, Maniam J, Cheung PT, Urakami T, von Oettingen J, Likitmaskul S, Ogle G. Epidemiology and phenotypes of diabetes in children and adolescents in non-European-origin populations in or from Western Pacific region. World J Clin Pediatr. 2022;11:173–95. https://doi.org/10.5409/wjcp.v11.i2.173.
Urakami T. Pediatric type 2 diabetes in Japan: similarities and differences from type 2 diabetes in other pediatric populations. Curr Diab Rep. 2018;18:29. https://doi.org/10.1007/s11892-018-0999-z.
Urakami T. New insights into the pharmacological treatment of pediatric patients with type 2 diabetes. Clin Pediatr Endocrinol. 2018;27:1–8. https://doi.org/10.1297/cpe.27.1.
Saitou H, Nakatani D, Myoui A, Kubota T, Ozono K. Pediatric drug development in Japan: current issues and perspectives. Clin Pediatr Endocrinol. 2020;29:1–7. https://doi.org/10.1297/cpe.29.1.
James DE, Chigutsa E, Chien J, Shen T. Population pharmacokinetics and pharmacodynamics of nasal glucagon in healthy subjects and patients with type 1 or type 2 diabetes. American Society for Clinical Pharmacology and Therapeutics. Abstract PIV-027. Available from: https://ascpt.Onlinelibrary.Wiley.Com/doi/10.1002/cpt.2167. Accessed 13 Mar 2023.
Beal S, Sheiner LB, Boeckmann A, Bauer RJ. NONMEM user’s guides (1989–2013). Ellicott City: Icon Development Solutions; 2013.
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO. Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. AAPS J. 2011;13:143–51. https://doi.org/10.1208/s12248-011-9255-z.
Ministry of Health, Labour and Welfare. The National Health and Nutrition Survey in Japan, 2017.
Dillman JR, Smith EA, Khalatbari S, Strouse PJ. IV glucagon use in pediatric MR enterography: effect on image quality, length of examination, and patient tolerance. AJR Am J Roentgenol. 2013;201:185–9. https://doi.org/10.2214/AJR.12.9787.
Graf CJ, Woodworth JR, Seger ME, Holcombe JH, Bowsher RR, Lynch R. Pharmacokinetic and glucodynamic comparisons of recombinant and animal-source glucagon after IV, IM, and SC injection in healthy volunteers. J Pharm Sci. 1999;88:991–5. https://doi.org/10.1021/js99007p.
Greenbaum CJ, Mandrup-Poulsen T, McGee PF, Battelino T, Haastert B, Ludvigsson J, Type 1 Diabetes Trial Net Research Group; European C-Peptide Trial Study Group, et al. Mixed-meal tolerance test versus glucagon stimulation test for the assessment of beta-cell function in therapeutic trials in type 1 diabetes. Diabetes Care. 2008;31:1966–71. https://doi.org/10.2337/dc07-2451.
Namba M, Hanafusa T, Kono N, Tarui S. Clinical evaluation of biosynthetic glucagon treatment for recovery from hypoglycemia developed in diabetic patients. The GL-G Hypoglycemia Study Group. Diabetes Res Clin Pract. 1993;19:133–8. https://doi.org/10.1016/0168-8227(93)90106-f.
Rygg A, Hindle M, Longest PW. Linking suspension nasal spray drug deposition patterns to pharmacokinetic profiles: a proof-of-concept study using computational fluid dynamics. J Pharm Sci. 2016;105:1995–2004. https://doi.org/10.1016/j.xphs.2016.03.033.
Matsumoto M, Awano H, Hirota Y, Nagai M, Bo R, Matsuoka A, et al. The prescription rates of glucagon for hypoglycemia by pediatricians and physicians are low in Japan. Endocrine. 2019;64:233–8. https://doi.org/10.1007/s12020-018-1793-z.
Murata T, Okazaki K, Yanagisawa K, Yamada K, Kuribayashi N, Totsuka Y, et al. Glucagon underutilized among type 1 diabetes mellitus patients in Japan. Diabetes Technol Ther. 2013;15:748–50. https://doi.org/10.1089/dia.2012.0290.
Harris G, Diment A, Sulway M, Wilkinson M. Glucagon administration: underevaluated and undertaught. Pract Diabetes Int. 2001;18:22–5. https://doi.org/10.1002/pdi.138.
Aranishi T, Nagai Y, Takita Y, Zhang S, Nishimura R. Usability of nasal glucagon device: partially randomized caregiver and third-party user experience trial with simulated administration at a Japanese site. Diabetes Ther. 2020;11:197–211. https://doi.org/10.1007/s13300-019-00711-1.
Acknowledgements
We thank all participants, their caregivers, investigators, and study site staff who were involved in the included studies. This study was sponsored by Eli Lilly and Company. Medical writing support (Kaye L. Stenvers, PhD and Elizabeth Flate, PhD) and editing support (Christopher J. Glaser, Antonia Baldo, and Dana Schamberger, MA, USA) were provided by Syneos Health and funded by Eli Lilly Japan K.K.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Eli Lilly and Company, IN, USA. The preparation of this manuscript and the open access publishing fee were sponsored by Eli Lilly Japan K.K.
Conflict of interest
RN and YN are employees of Eli Lilly Japan K.K. and minor stock shareholders of Eli Lilly and Company. DEJ, EC, and PG are employees and minor stock shareholders of Eli Lilly and Company.
Ethics approval
The clinical studies cited herein were approved by an institutional review board at each site and were conducted in accordance with the Declaration of Helsinki and the International Council for Harmonisation Good Clinical Practice guidelines.
Consent to participate
Patients provided written informed consent prior to participation in the clinical studies cited herein.
Consent for publication
Not applicable.
Availability of data and material
Eli Lilly and Company provides access to all individual participant data collected during the trial, after anonymization, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and European Union and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms, will be provided in a secure data-sharing environment. For details on submitting a request, see the instructions provided at http://www.vivli.org.
Code availability
Not applicable.
Author contributions
All authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this manuscript to be published.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nasu, R., James, D.E., Chigutsa, E. et al. Dose Rationale of Nasal Glucagon in Japanese Pediatric Patients with Diabetes Using Pharmacokinetic/Pharmacodynamic Modeling and Simulation. Pediatr Drugs 25, 377–387 (2023). https://doi.org/10.1007/s40272-023-00565-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-023-00565-y