Abstract
Stroke and perinatal asphyxia have detrimental effects on neuronal cells, causing millions of deaths worldwide each year. Since currently available therapies are insufficient, there is an urgent need for novel neuroprotective strategies to address the effects of cerebrovascular accidents. One such recent approach is based on the neuroprotective properties of estrogen receptors (ERs). However, activation of ERs by estrogens may contribute to the development of endometriosis or hormone-dependent cancers. Therefore, in this study, we utilized ospemifene, a novel selective estrogen receptor modulator (SERM) already used in dyspareunia treatment. Here, we demonstrated that posttreatment with ospemifene in primary neocortical cell cultures subjected to 18 h of hypoxia and/or ischemia followed by 6 h of reoxygenation has robust neuroprotective potential. Ospemifene partially reverses hypoxia- and ischemia-induced changes in LDH release, the degree of neurodegeneration, and metabolic activity. The mechanism of the neuroprotective actions of ospemifene involves the inhibition of apoptosis since the compound decreases caspase-3 overactivity during hypoxia and enhances mitochondrial membrane potential during ischemia. Moreover, in both models, ospemifene decreased the levels of the proapoptotic proteins BAX, FAS, FASL, and GSK3β while increasing the level of the antiapoptotic protein BCL2. Silencing of specific ERs showed that the neuroprotective actions of ospemifene are mediated mainly via ESR1 (during hypoxia and ischemia) and GPER1 (during hypoxia), which is supported by ospemifene-evoked increases in ESR1 protein levels in hypoxic and ischemic neurons. The results identify ospemifene as a promising neuroprotectant, which in the future may be used to treat injuries due to brain hypoxia/ischemia.
Similar content being viewed by others
Introduction
Among brain injuries caused by deficits in oxygen and/or glucose availability, perinatal asphyxia, and stroke can be distinguished. Perinatal asphyxia is a serious condition that affects up to 2% of all newborns born alive and may lead to death in 15–20% of them. Furthermore, prolonged hypoxia may lead to myocardiocyte dysfunction, in turn causing cardiac failure, which results in brain and peripheral organ ischemia. It is estimated that one-fourth of babies that survive these episodes suffer from hypoxic-ischemic encephalopathy (Gebregziabher et al. 2020). Currently, the most commonly used therapy is hypothermia, which has many side effects (Locci et al. 2020). For adults, over 13.7 million people worldwide suffer from stroke yearly, and for 5.5 million of them, the incident leads to death (Johnson et al. 2019). Ischemic stroke (the stroke resulting from a blood vessel clog that disables blood supply) constitutes the majority of strokes (~ 71%) (Feigin et al. 2018). Currently, the main approach to treating ischemic stroke is unblocking the clogged vessel. This treatment can be accomplished in two distinct ways: pharmacologically (utilizing recombinant tissue plasminogen activator (rtPA)) and mechanically (with surgical thrombectomy). Nonetheless, the abovementioned therapies have serious limitations and side effects; e.g., rtPA must be used at a maximum of 4.5 h from the beginning of the episode, and its usage often leads to cerebral hemorrhages, which increase the risk of death (Vivien et al. 2011). Concerning mechanical thrombectomy, the freed clog may block other arteries, such as those in the heart or lungs (Fukuta et al. 2017). Moreover, despite the restoration of blood flow, secondary cerebral ischemia/reperfusion injury may often be induced (Shichita et al. 2012).
Thus, there is an urgent need for new neuroprotective strategies for the treatment of cerebrovascular accidents. One such recent approach is based on the neuroprotective properties of estrogen receptors (ERs). Natural ligands of ERs are steroid hormones belonging to a group of estrogens. Although estrogens act as effective neuroprotectants, their excessive administration may contribute to the development of endometriosis or hormone-dependent cancers, such as ovarian or breast cancer (Patel et al. 2018a, b). Selective estrogen receptor modulators (SERMs) appear to be a much safer option. SERMs are chemical compounds that act as an ER agonist or antagonist, depending on the tissue. Hence, utilizing SERMs enables the simultaneous acquisition of estrogenic effects in desired organs and protection of other organs from estrogen excess. Previous studies have already shown that both natural SERMs (genistein, daidzein) and synthetic SERMs (raloxifene, tamoxifen, bazedoxifene, and pathway preferential estrogen-1 (PaPE-1)) can protect neurons in and/or in vivo models of cerebrovascular accidents (Kimelberg et al. 2000; Kajta et al. 2007; Wakade et al. 2008; Castelló-Ruiz et al. 2011; Kajta et al. 2013; Rzemieniec et al. 2015; Jover-Mengual et al. 2017; Khanna et al. 2017; Rzemieniec et al. 2018; Selvaraj et al. 2018; Burguete et al. 2019; Wnuk et al. 2021a). The compound tested in the current study is ospemifene, which has been approved for the treatment of dyspareunia and used in the USA since 2013 and in Europe since 2015 (Rutanen et al. 2003; Cagnacci et al. 2020). Ospemifene treatment is well tolerated and presents a good safety profile (Di Donato et al. 2019). Aside from dyspareunia, ospemifene has also been tested in the context of breast cancer therapy (Lubián López 2022). The ability of ospemifene to cross the blood–brain barrier (BBB) has not been studied so far. However, the admetSAR, a free tool for evaluating ADMET (absorption, distribution, metabolism, excretion, and toxicity properties of chemicals), predicted that ospemifene has ability to cross the blood–brain barrier with the probability of 0.7095 (DrugBank database). In addition, during stroke, the BBB is damaged (Bernardo-Castro et al. 2020). This pathology makes it possible for the substances to pass through the blood–brain barrier and to exhibit their intended neuroprotection during brain pathology.
Since ospemifene is successfully used in the pharmacotherapy of urogenital diseases, the current study was aimed at assessing for the first time the neuroprotective capacity of ospemifene in in vitro hypoxia and ischemia models.
Materials and Methods
Materials
Phosphate-buffered saline (PBS) was purchased from Biomed Lublin (Lublin, Poland). B27 and neurobasal media were obtained from Gibco (Grand Island, NY, USA). The LDH cytotoxicity detection kit was purchased from TaKaRa (Kusatsu, Japan). Enzyme-linked immunosorbent assay (ELISA) kits for BAX, BCL2, FAS, FASL, GSK3β, ESR1, ESR2, and GPER1 were purchased from Bioassay Technology Laboratory (Shanghai, China). Culture plates were obtained from TPP Techno Plastic Products AG (Trasadingen, Switzerland). L-glutamine, fetal bovine serum (FBS), dimethyl sulfoxide (DMSO), 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES), 3-[(3-cholamidopropyl)dimethylammonio]-1-propanesulfonate hydrate (CHAPS), ammonium persulfate, N,N,N′,N′-tetramethylethane-1,2-diamine (TEMED), 2-amino-2-(hydroxymethyl)-1,3-propanediol (TRIZMA base), DL-dithiothreitol, sodium deoxycholate, the protease inhibitor cocktail (ethylenediaminetetraacetic acid-free), radioimmunoprecipitation assay buffer (RIPA) buffer, ospemifene, ormeloxifene, thiazolyl blue tetrazolium bromide, protease inhibitor cocktail for mammalian tissues, and polyornithine were obtained from Sigma-Aldrich (St. Louis, MO, USA). JC-10 was purchased from Abcam (Cambridge, UK). The RNeasy Mini Kit was obtained from Qiagen (Hilden, Germany). A High-Capacity cDNA-Reverse Transcription Kit, TaqMan Gene Expression Master Mix, and TaqMan probes for specific genes encoding Bax, Bcl2, Fas, Fasl, Gsk3b, Esr1, Esr2, Gper1, Cyp19a1, and Actb were obtained from Thermo Fisher Scientific (Waltham, MA, USA). Fluoro-Jade C was purchased from Biosensis (Australia). Calcein AM and Hoechst 33342 were purchased from Molecular Probes (Eugene, OR, USA).
Methods
Primary Neocortical Cell Cultures
Primary neocortical cell cultures were established from mouse embryos (CD-1® IGS Swiss mouse, Charles River, Germany) on the 15th day of gestation as previously described (Kajta et al. 2006, 2009a, 2020). Briefly, minced cortices were incubated with 0.1% trypsin for 15 min at 37 °C. The trypsinization process was terminated using fetal bovine serum (FBS). The neuronal cells were centrifuged at 1000 RPM for 5 min and then submerged in medium containing 10% FBS. Then, the cells were seeded on poly-L-ornithine-coated (0.1 mg/ml) plates at a density of 2.0 × 105 cells per cm2 in multiwell plates. Cells were cultivated in phenol red-free neurobasal medium containing FBS, B27, L-glutamine, and penicillin‒streptomycin antibiotics for 2 days. For the following days, a medium deprived of FBS was utilized. The neuronal cell cultures were kept in a humidified incubator at 37 °C with 5% CO2 for 7 days in vitro.
All experiments were conducted according to the principles of the Three Rs in compliance with the European Union Legislation (Directive 2010/63/EU, amended by Regulation (EU) 2019.1010) and the ethical standards in the Guide for the Care and Use of Laboratory Animals (NIH).
Experimental Models of Normoxia, Hypoxia, and Ischemia
In this study, models of 18 h of normoxia, hypoxia, or ischemia followed by 6 h of reoxygenation were used. All experiments were started on the 7th day of in vitro culture.
Normoxia Model
In the normoxic model, on the day of the experiment, the medium was changed to standard medium, and the cells were incubated for 18 h. After that, the spent medium was replaced with fresh medium for the next 6 h.
Hypoxia Model
For the induction of hypoxia, the cell medium was replaced with standard medium, and the cells were placed in a prewarmed and humidified hypoxia modulator incubator chamber with 95% N2 and 5% CO2 for 18 h. The episode was followed by medium replacement with standard medium. Cells were incubated with fresh medium for 6 h.
Ischemia Model
For modeling of ischemic conditions, in contrast to hypoxic conditions, glucose-deprived neurobasal medium was utilized. Cells subjected to ischemia were also placed in the abovementioned hypoxia chamber for 18 h. After the episode, the cell medium was immediately changed to a fully supplemented medium for 6 h.
Treatment
Ospemifene (0.1–10 μM) was administered in two paradigms: cotreatment and posttreatment (Scheme 1). Ormeloxifene (1–10 μM) was administered in the posttreatment paradigm.
Cotreatment
In cotreatment, the tested compound or vehicle was administered at the beginning of the 18 h-long episode of hypoxic/ischemic damage (Scheme 1A). Then, the medium was replaced with fresh medium without the compound/vehicle.
Posttreatment
In the posttreatment paradigm, the experiment began after 18 h of hypoxia-/ischemia-induced damage. The tested compound or vehicle was administered for 6 h of reoxygenation (Scheme 1B).
Since posttreatment is much more clinically relevant than cotreatment, it was chosen for the majority of experiments.
Measurement of Lactate Dehydrogenase (LDH) Release
LDH release is a hallmark of hypoxia-/ischemia-induced cytotoxicity. For the measurement of the parameters, a cytotoxicity detection kit (TaKaRa, Kusatsu, Japan) was utilized according to the manufacturer’s protocol as previously described (Kajta et al. 2001). After the experiment from each well, cell-free supernatant was collected and then incubated with a proper reagent for 30 min at room temperature. As a result of the reaction, an appropriate amount of formazan salt was produced. The intensity of the red color was measured using the Infinite M200pro microplate reader (Tecan, Mannedorf, Switzerland) at 490 nm and analyzed in i-control software. The absorbance of blanks (no-enzyme controls) was subtracted from each value, and the obtained data were normalized to those of vehicle-treated cells. The obtained results are presented as a percent of the control ± SEM.
Apoptosis Evaluation with Measurement of Caspase-3 Activity
Caspase-3 activity is one of the main indicators of apoptotic cell death. For the analysis of caspase-3 activity, cells were first lysed with lysis buffer containing DTT (DL-dithiothreitol, Sigma-Aldrich, St. Louis, MO, USA) and then incubated at 37 °C with the colorimetric substrate Ac-DEVD-pNA (Sigma-Aldrich, St. Louis, MO, USA) as previously described (Rzemieniec et al. 2016; Kajta et al. 2019). The substrate was cleaved by caspase-3 to p-nitroaniline, and the levels were measured after 60 min using an Infinite M200PRO microplate reader (Tecan, Switzerland) and Tecan i-control software. The blank sample was subtracted from each value, and the obtained data were standardized to the absorbance of the control (DMSO-treated) cells. The results are presented as a percentage of the control ± SEM.
Neurodegenerative Cell Staining Utilizing Fluoro-Jade C
Fluoro-Jade C staining was used to label degenerating neurons. The procedure was performed as described by Gu et al. (2014). The culture medium was replaced with reagent (Biosensis, Australia) dissolved in distilled water. Then, the cells were incubated with the mixture for 1 h. The fluorescence intensity was measured at 490 nm excitation and 525 nm emission wavelengths using an Infinite M200PRO microplate reader (Tecan, Switzerland) and Tecan i-control software. The obtained results were normalized to the control cells and are presented as a percent of the control ± SEM. The blank sample was subtracted from each value.
Mitochondrial Membrane Potential Assessment Using JC-10
Measurement of mitochondrial membrane potential was performed using a JC-10 Assay Kit (Abcam, Cambridge, UK) as previously described (Przepiórska et al. 2023). JC-10 transpires into mitochondria and polymerizes there in cells with proper mitochondrial membrane potential, forming aggregates with characteristic red fluorescence. Low mitochondrial membrane potential results in a lack of JC-10 transport into mitochondria, leading to JC-10 green fluorescent monomer deposition in the cytoplasm. The cell culture medium was replaced with phosphate-buffered saline (PBS) (Biomed, Poland). After a 15-min incubation, the JC-10 dye solution was added, and the cells were incubated with the reagent for another 30 min. Then, Assay Buffer B was added, and immediate measurements at Ex/Em = 490/525 nm (green fluorescence) and 540/590 (red fluorescence) were performed using the Infinite M200PRO microplate reader (Tecan, Switzerland) and Tecan i-control software. The next step of the analysis was a calculation of the red to green fluorescence ratio. The obtained values were normalized to those of vehicle-treated cells and are expressed as a percent of the control ± SEM.
Determination of Cell Metabolic Activity with MTT Staining
MTT staining is based on the oxidoreductase ability to reduce yellow tetrazolium salt to purple formazan salt. The amount of formazan crystals is proportional to cell metabolic activity. Neuronal metabolic activity was determined using thiazolyl blue tetrazolium bromide (Sigma-Aldrich, St. Louis, MO, USA) as previously described (Wnuk et al. 2020, 2021a, 2021b). Briefly, methylthiazolyldiphenyl-tetrazolium bromide (MTT) solution was added to the culture medium for 1 h, and then, to dissolve formazan crystals, the medium was replaced with DMSO. The absorbance was measured at 570 nm in an Infinite M200PRO microplate reader (Tecan, Switzerland) and analyzed with Tecan i-control software. The value of the blank sample was subtracted from each value, and the obtained data were normalized to the absorbance of the control (DMSO-treated) cells. The results are presented as a percentage of the control ± SEM.
Staining with Calcein AM and Hoechst 33342
Cells were stained with calcein AM and Hoechst 33342 after 18 h of hypoxia/ischemia and 6 h of reoxygenation, as previously described (Kajta et al. 2009b). Calcein AM, a dye based on intracellular esterase activity, was used to visualize cell viability. Apoptotic cells containing bright blue fragmented nuclei, indicating condensed chromatin, were identified as apoptotic cells using Hoechst 33342. Cells cultured on glass coverslips were washed with PBS and incubated with Hoechst 33342 (0.6 mg/ml) at room temperature (RT) for 5 min. Cells were then washed with PBS and incubated in 2 μM calcein AM in PBS at RT for 10 min. Fluorescence intensity was monitored using a reversed fluorescence microscope (Leica DMIL LED, Leica Camera AG, Wetzlar, Germany) equipped with a Leica Flexacam C3 camera. The mean fluorescence intensity of calcein AM was quantified from 5 to 6 images per group using ImageJ software. The results are presented as a percentage of the control ± SEM.
Silencing of Esr1, Esr2, and Gper1 Using Small Interfering RNA (siRNA)
Esr1, Esr2, and Gper1 gene silencing was performed using specific siRNAs (Santa Cruz Biotechnology, Santa Cruz, CA, USA). Each siRNA was applied separately for 7 h at 50 nM in antibiotic-free medium containing the siRNA transfecting reagent INTERFERin™ as previously described (Kajta et al. 2014, 2020). After transfection, the cell culture medium was changed, and the cells were incubated for 21 h prior to the start of the hypoxic/ischemic experiment. As a control, negative (scrambled) siRNA containing sequences that do not lead to degradation of any known mRNA was used. The effectiveness of mRNA silencing was previously verified through the measurement of specific mRNAs using qPCR (Rzemieniec et al. 2015; Wnuk et al. 2018).
RT qPCR Analysis
An RNeasy Mini Kit (Qiagen, Hilden, Germany) and the spin column method were used to extract total RNA from neocortical cell cultures. The quantity of RNA was measured using an ND-1000 UV Vis NanoDrop (Thermo Fisher NanoDrop, Waltham, MA, USA) at 260 nm and 260/280 nm. Immediately after isolation, the extracted RNA was reverse-transcribed with a High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher Scientific, Waltham, MA, USA) with the T100 Thermal Cycler (Bio-Rad, Hercules, CA, USA). The obtained cDNA was then stored at − 20 °C. The cDNA was amplified by quantitative polymerase chain reaction (qPCR) using FastStart Universal Probe Master (Roche, Switzerland) that included TaqMan Gene Expression Assays (Thermo Fisher Scientific, Waltham, MA, USA) specific for Bax, Bcl2, Fas, Fasl, Gsk3b, Esr1, Esr2, Gper1, Cyp19a1, Hprt, Gapdh, and Actb. The amplification mixture in a total volume of 20 μl contained the following: 10 μl of FastStart Universal Probe Master, 8 μl of RNase free water, 1 μl of cDNA template, and 1 μl of the TaqMan gene expression Assay Mix. The procedure was performed using the following steps: 2 min at 50 °C, 10 min at 95 °C, and 40 cycles of 15 s at 95 °C and 1 min at 60 °C, with the CSX Real-Time system (Bio-Rad, Hercules, CA, USA) as previously described (Wnuk et al. 2016, 2018, 2019). Then, the delta Ct method was utilized to analyze the obtained data. To choose the reference gene, we used the following algorithms: geNorm, NormFinder, BestKeeper, and delta Ct, which identified Actb as the most stable reference gene among all experimental groups.
Enzyme-Linked Immunosorbent Assays (ELISAs)
To determine the protein expression of BAX, BCL2, FAS, FASL, GSK3β, ESR1, ESR2, and GPER1, we used enzyme-linked immunosorbent mouse-specific assays (ELISAs; Bioassay Technology Laboratory, China) according to the manufacturer’s instructions, as previously described (Kajta et al. 2017; Rzemieniec et al. 2019). Values obtained by the absorbance measurement at 450 nm were correlated with the amount of specific protein. For the measurement of the total protein concentration, Bradford reagent (Bio-Rad Protein Assay, Hercules, CA, USA) and bovine serum albumin (as a standard) were utilized. The results are presented as a percentage of the control ± SEM.
Data Analysis
The statistical tests were performed on raw data and are expressed as the mean absorbance or fluorescence units per well containing 50,000 cells for the LDH, caspase-3, Fluoro-Jade C, JC-10, and MTT assays; the fluorescence units per 1.5 million cells for qPCR; and the pg of BAX, BCL2, FAS, FASL, GSK3β, ESR1, ESR2, and GPER1 per µg of total protein for the ELISAs. Leven’s test for homogeneity of variances, followed by one-way analysis of variance (ANOVA), was used to determine the overall significance. The differences between the control and experimental groups were assessed with a post hoc Newman‒Keuls test. Significant differences were symbolized as follows: *p < 0.05, **p < 0.01, and ***p < 0.001 (compared to the control groups), #p < 0.05, ##p < 0.01, and ###p < 0.001 (compared to the cells subjected to hypoxia), and ^p < 0.05, ^^p < 0.01, and ^^^p < 0.001 (compared to the cultures exposed to ischemia). The results are expressed as the mean ± SEM of the number of experiments and replicates indicated below the corresponding figures.
Results
Ospemifene Decreased Hypoxia- and Ischemia-Induced LDH Release in the Posttreatment Paradigm, but Ormeloxifene Stimulated LDH Release in Hypoxic and Ischemic Neurons
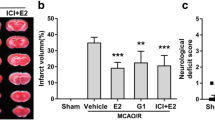
Measurement of LDH release was performed to assess the extent of hypoxia/ischemia-induced cytotoxicity. Eighteen hours of hypoxia or ischemia followed by 6 h of reoxygenation resulted in an increase in LDH release to 312-315% or 280% of the normoxic value, respectively.
In the hypoxic model, ospemifene at concentrations of 5 and 10 μM effectively decreased LDH release from 312 to 248% and 226% of the normoxic control in cotreatment (Fig. 1a) and from 315 to 277% and 260% of the normoxic control in the posttreatment paradigm (Fig. 1b). Furthermore, ospemifene (5 and 10 μM) administration after the episode effectively diminished ischemia-induced LDH release, resulting in a change in this parameter from 278% of the control to 231% and 246%, respectively (Fig. 1b).
Ospemifene reduced hypoxia- and ischemia-induced LDH release in the posttreatment paradigm. Ospemifene (0.1, 1, 5, and 10 μM) was applied in the cotreatment paradigm (a) and posttreatment paradigm (b). The results are presented as a percentage of the normoxic control. Each bar represents the mean ± SEM of three independent experiments. The number of replicates ranged from 20 to 30. ***p < 0.001 compared to the normoxic cultures; ##p < 0.01 and ###p < 0.001 compared to the cultures exposed to hypoxia; ^^p < 0.01 and ^^^p < 0.001 compared to the cultures exposed to ischemia
In these models, ospemifene concentrations of 0.1 and 1 μM were ineffective. Concentrations of 5 and 10 μM did not have any protective effects in the ischemic model when the compound was administered in a cotreatment paradigm.
Ospemifene at concentrations of 0.1, 1, 5, and 10 μM, either in the co- or posttreatment paradigm, did not change LDH release under normoxic conditions (Supplementary Materials, Tables S1 and S2).
Ormeloxifene (1, 5, and 10 μM) was applied in the posttreatment paradigm. Posttreatment with ormeloxifene (10 μM) further increased both hypoxia- and ischemia-induced LDH release, while concentrations of 1 and 5 μM did not alter this parameter in either model (Supplementary Materials, Fig. S1). In normoxic conditions, posttreatment with ormeloxifene did not affect LDH release (Supplementary Materials, Table S3).
Ospemifene Decreased Elevated Caspase-3 Activity in the Hypoxic Model in Both Cotreatment and Posttreatment Paradigms, but Ormeloxifene Stimulated Caspase-3 Activity in Hypoxic Neurons
Caspase-3 activity is a well-known indicator of apoptotic cell death. Hypoxia and ischemia increase caspase-3 activity to approximately 170% and 145% of the normoxic value, respectively.
Application of ospemifene at a concentration of 10 μM decreased caspase-3 activity in the hypoxic model in either paradigm (reduction from 160 to 127% of the normoxic value in the cotreatment paradigm and from 175 to 150% in the posttreatment paradigm) (Fig. 2a, b). The concentration of 5 μM was effective only in the posttreatment paradigm and caused caspase-3 activity to decrease from 175 to 157% of the normoxic control (Fig. 2b). In the ischemic model, ospemifene showed no effects in either of the utilized paradigms (Fig. 2a, b).
Ospemifene decreased elevated caspase-3 activity in the hypoxic model in both co-treatment and posttreatment paradigms. Ospemifene (0.1, 1, 5, and 10 μM) was applied in the cotreatment paradigm (a) and posttreatment paradigm (b). The results are presented as a percentage of the normoxic control. Each bar represents the mean ± SEM of three independent experiments. The number of replicates ranged from 20 to 30. ***p < 0.001 compared to the normoxic cultures; #p < 0.05, ##p < 0.01 and ###p < 0.001 compared to the cultures exposed to hypoxia
Ospemifene (0.1, 1, 5, and 10 μM), administered either in the co- or posttreatment paradigm, did not change caspase-3 activity under normoxic conditions (Supplementary Materials, Tables S1 and S2).
Since the posttreatment paradigm reflects clinical aspects much better than cotreatment and ospemifene is even more protective in this paradigm, we decided to use the posttreatment model for the following experiments. The most effective concentrations, i.e., 5 and 10 μM, were chosen for the next experiments.
Posttreatment with ormeloxifene (1, 5, and 10 μM) further increased hypoxia-induced caspase-3 activity and did not alter ischemia-induced caspase-3 activity (Supplementary Materials, Fig. S2). In normoxia, ormeloxifene had no effect on caspase-3 activity (Supplementary Materials, Table S3).
Ospemifene Reduced the Neuronal Cell Degeneration Induced by Hypoxia and Ischemia
Fluoro-Jade C labeling was used to assess the degree of neurodegeneration. Ospemifene (5 and 10 μM) effectively reduced hypoxia-induced cell degeneration from 118% of the normoxic control to 105% (5 μM) and 99% (10 μM) (Fig. 3). Moreover, the tested compound normalized the ischemia-induced increase in neurodegeneration, from 131% of the normoxic control to 113% in the case of 5 μM ospemifene and 106% in the case of 10 μM ospemifene (Fig. 3).
Posttreatment with ospemifene (5 and 10 μM) diminished neuronal cell degeneration (in terms of Fluoro-Jade C staining) induced by hypoxia and ischemia. The results are presented as a percentage of the normoxic control. Each bar represents a mean ± SEM. The number of replicates ranged from 12 to 24. ***p < 0.001 compared to the normoxic cultures; ###p < 0.001 compared to the cultures exposed to hypoxia; ^^^p < 0.001 compared to the cultures exposed to ischemia
Ospemifene administration showed no effects on the degree of neurodegeneration under normoxic conditions (Supplementary Materials, Table S2).
Ospemifene Partially Restored the Lost Mitochondrial Membrane Potential in the Ischemic Model
JC-10 dye was used to measure mitochondrial membrane potential. Both hypoxia and ischemia induced a loss of mitochondrial membrane potential to 60% and 24% of the control value, respectively (Fig. 4). Ospemifene at concentrations of 5 and 10 μM partially restored the lost potential in the ischemic model (35% and 33% of the normoxic value, respectively) but showed no effects under hypoxic conditions (Fig. 4).
Posttreatment with ospemifene (5 and 10 μM) partially restored the lost mitochondrial membrane potential in the ischemic model. The results are presented as a percentage of the normoxic control. Each bar represents the mean ± SEM of three independent experiments. The number of replicates ranged from 15 to 20. ***p < 0.001 compared to the normoxic cultures; ^^^p < 0.001 compared to the cultures exposed to ischemia
Ospemifene itself (5 and 10 μM) did not alter this parameter under normoxic conditions (Supplementary Materials, Table S2).
Ospemifene Restored Cell Metabolic Activity, Which Was Decreased by Hypoxia and Ischemia
Hypoxia and ischemia diminished cell metabolic activity to 86% and 71% of the normoxic value, respectively (Fig. 5). Ospemifene administration increased the abovementioned parameter value to 95% (5 μM) and 97% (10 μM) in the hypoxia model and to 75% (5 μM) and 83% (10 μM) in the ischemia model (Fig. 5).
Posttreatment with ospemifene elevates cell metabolic activity that was decreased by hypoxia and ischemia. The results are presented as a percentage of the normoxic control. Each bar represents the mean ± SEM of three independent experiments. The number of replicates ranged from 10 to 20. ***p < 0.001 compared to the normoxic cultures; ###p < 0.001 compared to the cultures exposed to hypoxia; ^p < 0.05 and ^^^p < 0.001 compared to the cultures exposed to ischemia
Under normoxic conditions, 5 and 10 μM ospemifene did not cause profound changes in cell metabolic activity (Supplementary Materials, Table S2).
For further analyses, 10 μM ospemifene was selected because it caused more pronounced neuroprotection than 5 μM ospemifene.
Ospemifene Increased Reduced Cell Viability and Lowered Apoptotic Body Formation
As indicated by calcein AM staining, hypoxia and ischemia decreased cell viability to 56% and 44% of the normoxic control, respectively (Fig. 6). Ospemifene (10 μM) partially reversed the observed effects in both hypoxia and ischemia (72% and 61% of the normoxic control, respectively) but did not alter the parameter in normoxia (Supplementary Materials, Table S2).
Hypoxia and ischemia decrease cell viability and increase apoptotic body formation. Ospemifene (10 μM) partially reverses these alterations. The results in the table are presented as a percentage of the normoxic control. Each value represents the mean ± SEM of the mean fluorescence intensity from 5 to 6 photos per group. ***p < 0.001 compared to the normoxic cultures; #p < 0.05 compared to the cultures exposed to hypoxia; ^p < 0.05 compared to the cultures exposed to ischemia
Both hypoxia and ischemia increased apoptotic body formation, visible as bright blue fragmented nuclei, indicating condensed chromatin. Administration of ospemifene (10 μM) reduced the number of apoptotic bodies in hypoxic and ischemic conditions (Fig. 6).
Ospemifene Altered the mRNA and Protein Levels of Apoptosis-Related Factors
Under the experimental conditions, the mRNA levels of antiapoptotic Bcl2 and proapoptotic Gsk3b are altered in similar ways, i.e., both hypoxia and ischemia significantly increased their levels (for Bcl2, 1.48-fold increase in hypoxia and 1.64-fold increase in ischemia; for Gsk3b, 1.29- and 1.36-fold increase in hypoxia and ischemia, respectively). The application of ospemifene showed no influence on the expression of the abovementioned genes in either the hypoxic or ischemic model (Fig. 7a). Hypoxia also increased the levels of proapoptotic Bax (1.26-fold) but did not affect Fas and Fasl levels, whereas the ischemic model was characterized by an increase in the mRNA levels of Bax (2.05-fold), Fas (11.68-fold), and Fasl (1.67-fold). Ospemifene (10 μM) caused a further increase in Bax (from 1.26- to 1.45-fold) and Fas (from 1.57- to 2.44-fold) expression in the hypoxic model as well as Fas (from 11.68- to 12.68-fold) and Fasl (from 1.67- to 1.95-fold) expression in the ischemic model (Fig. 7a).
Hypoxia and ischemia as well as posttreatment with ospemifene (10 μM) affected the levels of apoptosis-related mRNAs and protein levels. The results are presented as a percentage of the normoxic control. Each bar represents the mean ± SEM of 4 to 5 replicates per group. *p < 0.05, **p < 0.01, and ***p < 0.001 compared to the normoxic cultures; #p < 0.05, ##p < 0.01, and ###p < 0.001 compared to the cultures exposed to hypoxia; ^p < 0.05, ^^p < 0.01, and ^^^p < 0.001 compared to the cultures exposed to ischemia
Eighteen hours of either hypoxia or ischemia followed by 6 h of reoxygenation increased the protein levels of proapoptotic BAX (148% and 201% of the control in hypoxia and ischemia, respectively), FAS (152% and 285% of the normoxic control in hypoxia and ischemia, respectively), FASL (268% and 435% of the normoxic control in hypoxia and ischemia, respectively), and GSK3β (202% and 221% of the normoxic control in hypoxia and ischemia, respectively) (Fig. 7b). Administration of 10 μM ospemifene in both hypoxic and ischemic models normalized the protein levels of all of the abovementioned proapoptotic proteins to levels comparable to the normoxic values (Fig. 7b). Moreover, in hypoxia, ospemifene (10 μM) enhanced the antiapoptotic BCL2 protein level (312% of the normoxic control) (Fig. 7b). The level of BCL2 was also elevated in response to ischemia (345% of the normoxic control) (Fig. 7b). Additionally, a further increase was observed under the influence of 10 μM ospemifene (415% of the normoxic control) (Fig. 7b).
In normoxia, ospemifene administration influenced the expression of neither of the abovementioned apoptosis-related mRNAs nor proteins (Supplementary Materials, Tables S4 and S5).
Ospemifene Altered the mRNA and Protein Levels of Estrogen Signaling-Related Factors
In primary neocortical cell cultures subjected to 18 h of ischemia followed by a 6 h reoxygenation period, we observed a significant increase in Esr2 and Gper1 mRNA expression (2.33- and 4.24-fold, respectively) (Fig. 8a). Administration of ospemifene at a concentration of 10 μM diminished, elevated in response to the ischemia, Gper1 mRNA expression (from 4.24- to 3.91-fold) (Fig. 8a). The Esr1 and Cyp19a1 genes did not show altered expression in response to hypoxic/ischemic damage or treatment with ospemifene.
The effects of 18 h of hypoxia or ischemia followed by 6 h of reoxygenation as well as 10 μM ospemifene administration on the mRNA and protein levels of estrogen signaling-related factors. Ospemifene was administered at the beginning of the reoxygenation period, i.e., in the posttreatment paradigm. Each bar represents a mean ± SEM. The number of replicates per group ranged from 4 to 5. *p < 0.05, **p < 0.01, and ***p < 0.001 compared to the normoxic cultures; #p < 0.05 and ###p < 0.001 compared to the cultures exposed to hypoxia; ^^^p < 0.001 compared to the cultures exposed to ischemia
For protein expression, exposure to the hypoxic model led to a decrease in ESR1 (46% of the normoxic control) and ESR2 (32% of the normoxic control) protein levels. Cells that underwent ischemia showed a profound decrease in ESR2 (12% of the normoxic control) protein expression and an elevation of GPER1 (199% of the normoxic control) protein expression (Fig. 8b). Ospemifene (10 μM) administered 18 h after the beginning of the episode (in the reoxygenation period) increased ESR1 levels in both hypoxic and ischemic models (172% and 394% of the normoxic control) (Fig. 8b). Moreover, ospemifene (10 μM) normalized the levels of ESR2 diminished in response to both hypoxia and ischemia as well as normalized the GPER1 level elevated in response to ischemia (Fig. 8b).
Under normoxic conditions, administration of ospemifene did not affect the expression of the abovementioned estrogen signaling-related mRNAs and proteins, except for the ESR2 level (Supplementary Materials, Tables S4 and S5).
Impact of Specific siRNAs on Ospemifene-Evoked Neuroprotection in Hypoxia–Ischemia-Induced Damage
Hypoxic Damage
Since ospemifene is neuroprotective in hypoxic neurons in terms of LDH release and caspase-3 activity (Figs. 1 and 2), we tested the involvement of specific ER types in the observed effects using specific siRNAs targeting Esr1, Esr2, and Gper1. In the cells undergoing hypoxia, Esr1 and Esr2 siRNAs diminished ospemifene-induced neuroprotection measured by caspase-3 activity, and Esr1 and Gper1 siRNAs limited neuroprotective potential of ospemifene measured by LDH release. In the cells subjected to hypoxia and then treated with ospemifene, Esr1 and Esr2 siRNAs increased caspase-3 activity to 101% and 95% of the negative hypoxic control, respectively (Fig. 9a). Moreover, in these cells, Esr1 and Gper1 siRNAs increased LDH release to 96% and 100% of the negative hypoxic control, respectively (Fig. 9b).
The effects of siRNA-induced silencing of Esr1, Esr2, or Gper1 on caspase-3 activity and LDH release in response to hypoxia (a, b) and ischemia (c) in combination with ospemifene (10 μM) administration. Each bar represents the mean ± SEM of two independent experiments. The number of replicates ranged from 10 to 20. $$p < 0.01 and $$$p < 0.001 compared to the cultures exposed to negative (scrambled) siRNA and hypoxia or ischemia, respectively
Ischemic Damage
As mentioned above, ospemifene is neuroprotective in an ischemic model in terms of LDH release (Fig. 1). In the cells subjected to ischemia, Esr1 silencing abrogated the ospemifene-induced decrease in LDH release by increasing this parameter to 102% of the negative ischemic control (Fig. 9c). In the ischemic model, ospemifene did not affect caspase-3 activity; therefore, the impact of specific siRNAs has not been assessed.
Discussion
There is an urgent need for novel therapeutic strategies to treat conditions such as perinatal asphyxia and brain stroke. Since the available therapies are insufficient, researchers have put more effort into solving this pressing issue. According to the obtained data, ospemifene appears to be a promising pharmaceutical tool that can safely be used to treat injuries from brain hypoxia and ischemia. In this study, we demonstrated for the first time that posttreatment with ospemifene in primary neocortical cell cultures subjected to 18 h of hypoxia and/or ischemia followed by 6 h of reoxygenation has robust neuroprotective potential. Ospemifene partially reversed the hypoxia/ischemia-induced increase in LDH release and neurodegeneration, as well as the hypoxia/ischemia-evoked loss of metabolic activity. The mechanism of neuroprotective actions of ospemifene involves the inhibition of apoptosis since the compound lowers caspase-3 overactivity during hypoxia and enhances mitochondrial membrane potential during ischemia. Moreover, in both models of neuronal damage, ospemifene decreased the levels of the proapoptotic proteins BAX, FAS, FASL, and GSK3β while increasing the level of the antiapoptotic protein BCL2. Silencing of specific ERs suggested that the neuroprotective actions of ospemifene are mediated mainly via ESR1 (during hypoxia and ischemia) and GPER1 (during hypoxia), which is supported by ospemifene-evoked increases in ESR1 protein levels in hypoxic and ischemic neurons. Despite emerging evidence on the protective roles of certain SERMs against neurodegeneration, our data indicate that the neuroprotective capacity in such conditions is not attributed to all SERMs, as evidenced by testing ormeloxifene (supplementary data).
Neuronal cells subjected to hypoxia and ischemia die mainly in necrotic and apoptotic manners. Apoptosis is the basic mechanism of neuronal cell death that accompanies stroke and perinatal asphyxia. It is mainly because many apoptosis-related factors are located in mitochondria, and these organelles play a prominent role in cell metabolism that is depleted during oxygen deprivation. Cell membrane permeability is a hallmark of necrotic cell death, and in our study, the quantitative assessment of this process was performed by measuring the amount of LDH secreted outside the cell. We demonstrated that ospemifene protects neurons from hypoxia- and ischemia-induced increases in LDH activity and reduces caspase-3 activity (estimated to assess apoptosis) elevated due to hypoxia. Similar effects have been observed previously with other SERMs (e.g., bazedoxifene, raloxifene, and tamoxifen) or phytoestrogens (genistein, daidzein, and equol-daidzein metabolite), which possess SERM properties (Kajta et al. 2007, 2013; Wakade et al. 2008; Schreihofer and Redmond 2009; Rzemieniec et al. 2018). Nevertheless, the abovementioned substances were used in pre- or cotreatment paradigms, which do not reflect clinical utilization as a posttreatment paradigm does. Importantly, in the current study, ospemifene induced a significant neuroprotective effect when administered to the system several hours after the onset of the hypoxic-ischemic episode, which indicates the clinical potential of this compound. In this study, we also showed that ospemifene protects cells from neurodegeneration, which is similar to the effects previously demonstrated for tamoxifen and raloxifene in models of retinal ganglion cell and photoreceptor degeneration (Wang et al. 2017; Getter et al. 2019; Jiang et al. 2019).
A number of studies have proven that mitochondrial dysfunction plays an important role in the pathophysiology of neurodegenerative diseases, both acute (e.g., stroke) and chronic, e.g., Parkinson’s disease or Alzheimer’s disease (Soane et al. 2007). Improper mitochondrial function leads to several consequences, such as oxidative stress, disturbance of calcium ion homeostasis, induction of apoptosis, and metabolic failure (Soane et al. 2007). In the present study, hypoxia and ischemia decreased both the number of metabolically active cells and mitochondrial membrane potential. These effects were normalized by ospemifene, except for the hypoxia-induced decrease in mitochondrial membrane potential. The decreased mitochondrial membrane potential under hypoxic and ischemic conditions is a well-known phenomenon (Rzemieniec et al. 2015, 2018; Park et al. 2019; Ye et al. 2021). In addition to estradiol (Wang et al. 2001; Guo et al. 2010; Zhao et al. 2016), other SERMs, including raloxifene and bazedoxifene (in the cotreatment paradigm), are able to partially normalize this parameter (Rzemieniec et al. 2018).
The apoptotic pathway consists of several protein cascades, among which proapoptotic molecules such as BAX, BAD, BIM, JNK, GSK3β, and FAS as well as antiapoptotic BCL2 and BCLXL play important roles (Wnuk and Kajta 2017). In the current study, hypoxia and ischemia increased the expression of proapoptotic BAX, FAS, FASL, and GSK3β. Similar effects of hypoxia and ischemia have been observed in our previous studies performed with different time paradigms (6 h of hypoxia/ischemia and 18 h of reoxygenation) (Wnuk et al. 2021a, 2021b). The protein level of antiapoptotic BCL2 did not change in response to hypoxia but was increased in the ischemic model. The molecular mechanism of interaction between BCL2 and BAX relies on BCL2-induced conformational changes of BAX that prevent its oligomerization, which is necessary to form pores in the mitochondrial membrane (Dlugosz et al. 2006); in this way, the decrease in the BCL2/BAX ratio induces apoptosis. Upregulation of BCL2 in the ischemic model may seem surprising, but similar effects have already been observed in other cellular models of brain hypoxia and ischemia as well as Alzheimer’s and Huntington’s diseases (Satou et al. 1995; O’Barr et al. 1996; Kitamura et al. 1998; Sulejczak et al. 2004; Sassone et al. 2013; Wnuk et al. 2021a, 2021b; Przepiórska et al. 2023). The observed phenomenon is likely a survival mechanism. Ospemifene normalized all the mentioned proapoptotic protein levels and increased BCL2 levels in both used models. In general, estrogens are known to inhibit proapoptotic JNK and GSK3β kinase pathways, decrease the expression of proapoptotic proteins, such as BAX, BAD, or BIM, and increase antiapoptotic BCL2 and BCLXL expression (Arevalo et al. 2015; Wnuk and Kajta 2017; Raghava et al. 2017). A similar effect of upregulation of BCL2 and downregulation of BAX has been described previously for daidzein and genistein, which are phytoestrogens with SERM properties (Liu et al. 2017; Li et al. 2017). PaPE-1, a newly synthesized ER ligand that selectively acts on membrane ERs, has also recently been shown to reduce BAX, FAS, FASL, and GSK3β levels and upregulate BCL2 in response to hypoxia and ischemia (Wnuk et al. 2021a). The differences between the observed mRNA and protein levels may result from posttranscriptional degradation of mRNA, which may also contribute to the neuroprotective actions of the tested compound.
Ospemifene has a similar affinity for ESR1 (Ki = 380 nM) and ESR2 (Ki = 410 nM), but its binding to these receptors is weaker than that of estradiol (Ki = 10 and 5 nM, respectively) (Unkila et al. 2013). However, affinity does not necessarily determine the involvement of a given type of receptor in a particular effect observed under the influence of a ligand, as we evidenced using specific siRNAs. According to our results, in the cells subjected to ischemia and transfected with Esr1 siRNA, but not Esr2 or Gper1 siRNAs, ospemifene lost its neuroprotective property in terms of LDH release, which suggests the involvement of ESR1 in ospemifene-evoked neuroprotection against ischemic damage. For the model of hypoxia, in the cells transfected with all siRNAs used, ospemifene lost its neuroprotective capacity in terms of LDH release (Esr1 and Gper1 silencing) and caspase-3 activity (Esr1 and Esr2 silencing). Therefore, all studied ERs appeared to be involved in the neuroprotective action of ospemifene against hypoxic damage, although the measures of neuroprotection were different. Taking into account the LDH parameter, which reflects the final effect independent of preceding processes, such as caspase-3-dependent apoptosis, one may suggest that ESR1 plays a crucial role in ospemifene-evoked neuroprotection against hypoxic and ischemic damage, whereas GPER1 mediates the neuroprotective action of ospemifene only during hypoxia.
Ospemifene has thus far been tested on the U2OS osteosarcoma line, where similar to our results, the protective effect of ospemifene against etoposide-induced apoptosis was mediated primarily by ESR1 (Kallio et al. 2008). The protective effects of estrogens and SERMs may have different bases that depend on the type of ligand, the level of coregulators (coactivators and corepressors) in the cells and even their location in the body (Patel et al. 2018a, b). Previously, we demonstrated that the SERMs raloxifene and bazedoxifene executed ESR1-mediated neuroprotection against hypoxic damage in cortical and hippocampal neurons (Rzemieniec et al. 2015, 2018). We also showed key roles of ESR2 and GPER1 in the neuroprotective effect of daidzein, a phytoestrogen that possesses SERM properties (Kajta et al. 2013). Moreover, membrane ESR1 and ESR2 were found to mediate the protective effects of PaPE-1 on whole brains (Selvaraj et al. 2018) and hypoxic/ischemic neurons (Wnuk et al. 2021a).
In our study, a key role of ESR1 in ospemifene neuroprotection is supported by ospemifene-evoked increases in ESR1 protein levels during hypoxia and ischemia. Unfortunately, GPER1 involvement in ospemifene neuroprotection is not reflected by the ospemifene-induced increase in GPER1 protein levels during hypoxia. Intriguingly, ospemifene reduced GPER1 protein and Gper1 mRNA expression, but only during ischemia, suggesting an ambiguous role of the receptor during acute neuronal damage. For ESR2, its hypoxia/ischemia-reduced protein level was elevated after post-treatment with ospemifene, which suggests ESR2-mediated neuroprotection; however, Esr2 silencing suggested ESR2-mediated inhibition of hypoxia-induced caspase-3 activity but not LDH release.
In conclusion, in this study, it was demonstrated for the first time that posttreatment with ospemifene has a robust neuroprotective effect against hypoxic and ischemic damage. Ospemifene-evoked neuroprotection is mediated through ESR1 (hypoxia, ischemia) and GPER1 (hypoxia) and relies on inhibiting apoptosis, as evidenced by a decrease in caspase-3 activity, a rise in mitochondrial membrane potential and normalization of apoptosis-specific factors, in addition to lowering LDH release, neurodegeneration grade, and cellular metabolic activity.
Availability of Data and Materials
The data that support the findings of this study are available from the corresponding author upon reasonable request. Some data may not be made available because of privacy or ethical restrictions.
Abbreviations
- ERs:
-
Estrogen receptors
- rtPA:
-
Recombinant tissue plasminogen activator
- SERMs:
-
Selective estrogen receptor modulators
References
Arevalo MA, Azcoitia I, Garcia-Segura LM (2015) The neuroprotective actions of oestradiol and oestrogen receptors. Nat Rev Neurosci 16(1):17–29. https://doi.org/10.1038/nrn3856
Bernardo-Castro S, Sousa JA, Brás A, Cecília C, Rodrigues B, Almendra L, Machado C, Santo G, Silva F, Ferreira L, Santana I, Sargento-Freitas J (2020) Pathophysiology of blood-brain barrier permeability throughout the different stages of ischemic stroke and its implication on hemorrhagic transformation and recovery. Front Neurol 11:594672. https://doi.org/10.3389/fneur.2020.594672
Burguete MC, Jover-Mengual T, López-Morales MA, Aliena-Valero A, Jorques M, Torregrosa G, Alborch E, Castelló-Ruiz M, Salom JB (2019) The selective oestrogen receptor modulator, bazedoxifene, mimics the neuroprotective effect of 17β-oestradiol in diabetic ischaemic stroke by modulating oestrogen receptor expression and the MAPK/ERK1/2 signalling pathway. J Neuroendocrinol 31(8):e12751. https://doi.org/10.1111/jne.12751
Cagnacci A, Xholli A, Venier M (2020) Ospemifene in the management of vulvar and vaginal atrophy: focus on the assessment of patient acceptability and ease of use. Patient Prefer Adherence 14:55–62. https://doi.org/10.2147/PPA.S203614
Castelló-Ruiz M, Torregrosa G, Burguete MC, Salom JB, Gil JV, Miranda FJ, Jover-Mengual T, Marrachelli VG, Alborch E (2011) Soy-derived phytoestrogens as preventive and acute neuroprotectors in experimental ischemic stroke: influence of rat strain. Phytomedicine 18(6):513–515. https://doi.org/10.1016/j.phymed.2011.02.001
Di Donato V, Schiavi MC, Iacobelli V, D’oria O, Kontopantelis E, Simoncini T, Muzii L, Benedetti Panici P (2019) Ospemifene for the treatment of vulvar and vaginal atrophy: a meta-analysis of randomized trials. Part II: Evaluation of tolerability and safety. Maturitas 121:93–100. https://doi.org/10.1016/j.maturitas.2018.11.017
Dlugosz PJ, Billen LP, Annis MG, Zhu W, Zhang Z, Lin J, Leber B, Andrews DW (2006) Bcl-2 changes conformation to inhibit Bax oligomerization. EMBO J 25(11):2287–2296. https://doi.org/10.1038/sj.emboj.7601126
DrugBank database. https://go.drugbank.com/drugs/DB04938. Accessed 9 Mar 2023
Feigin VL, Nguyen G, Cercy K, Johnson CO, Alam T, Parmar PG, Abajobir AA, Abate KH, Abd-Allah F, Abejie AN, Abyu GY, Ademi Z, Agarwal G, Ahmed MB, Akinyemi RO, Al-Raddadi R, Aminde LN, Amlie-Lefond C, Ansari H, Roth GA (2018) Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med 379(25):2429–2437. https://doi.org/10.1056/NEJMoa1804492
Fukuta T, Asai T, Yanagida Y, Namba M, Koide H, Shimizu K, Oku N (2017) Combination therapy with liposomal neuroprotectants and tissue plasminogen activator for treatment of ischemic stroke. FASEB J 31(5):1879–1890. https://doi.org/10.1096/fj.201601209R
Gebregziabher GT, Hadgu FB, Abebe HT (2020) Prevalence and associated factors of perinatal asphyxia in neonates admitted to Ayder Comprehensive Specialized Hospital, Northern Ethiopia: a cross-sectional study. Int J Pediatr 2020:4367248. https://doi.org/10.1155/2020/4367248
Getter T, Suh S, Hoang T, Handa JT, Dong Z, Ma X, Chen Y, Blackshaw S, Palczewski K (2019) The selective estrogen receptor modulator raloxifene mitigates the effect of all-trans-retinal toxicity in photoreceptor degeneration. J Biol Chem 294(24):9461–9475. https://doi.org/10.1074/jbc.RA119.008697
Gu Q, Lantz-McPeak S, Rosas-Hernandez H, Cuevas E, Ali SF, Paule MG, Sarkar S (2014) In vitro detection of cytotoxicity using FluoroJade-C. Toxicol in Vitro 28(4):469–472. https://doi.org/10.1016/j.tiv.2014.01.007
Guo J, Krause DN, Horne J, Weiss JH, Li X, Duckles SP (2010) Estrogen-receptor-mediated protection of cerebral endothelial cell viability and mitochondrial function after ischemic insult in vitro. J Cereb Blood Flow Metab 30(3):545–554. https://doi.org/10.1038/jcbfm.2009.226
Jiang M, Ma X, Zhao Q, Li Y, Xing Y, Deng Q, Shen Y (2019) The neuroprotective effects of novel estrogen receptor GPER1 in mouse retinal ganglion cell degeneration. Exp Eye Res 189:107826. https://doi.org/10.1016/j.exer.2019.107826
Johnson CO, Minh Nguyen MN, Roth GA, Nichols E, Alam T, Abate D, Abd-Allah F, Abdelalim A, Abraha HN, Abu-Rmeileh NM, Adebayo OM, Christopher JL (2019) Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18(5):439–458. https://doi.org/10.1016/S1474-4422(19)30034-1
Jover-Mengual T, Castelló-Ruiz M, Burguete MC, Jorques M, López-Morales MA, Aliena-Valero A, Jurado-Rodríguez A, Pérez S, Centeno JM, Miranda FJ, Alborch E, Torregrosa G, Salom JB (2017) Molecular mechanisms mediating the neuroprotective role of the selective estrogen receptor modulator, bazedoxifene, in acute ischemic stroke: a comparative study with 17β-estradiol. J Steroid Biochem Mol Biol 171:296–304. https://doi.org/10.1016/j.jsbmb.2017.05.001
Kajta M, Budziszewska B, Marszał M, Lasoń W (2001) Effects of 17-beta estradiol and estriol on NMDA-induced toxicity and apoptosis in primary cultures of rat cortical neurons. J Physiol Pharmacol 52(3):437–446
Kajta M, Domin H, Grynkiewicz G, Lason W (2007) Genistein inhibits glutamate-induced apoptotic processes in primary neuronal cell cultures: an involvement of aryl hydrocarbon receptor and estrogen receptor/glycogen synthase kinase-3beta intracellular signaling pathway. Neuroscience 145(2):592–604. https://doi.org/10.1016/j.neuroscience.2006.11.059
Kajta M, Litwa E, Rzemieniec J, Wnuk A, Lason W, Zelek-Molik A, Nalepa I, Grzegorzewska-Hiczwa M, Tokarski K, Golas A, Guzik E, Grochowalski A, Szychowski KA, Wojtowicz AK (2014) Isomer-nonspecific action of dichlorodiphenyltrichloroethane on aryl hydrocarbon receptor and G-protein-coupled receptor 30 intracellular signaling in apoptotic neuronal cells. Mol Cell Endocrinol 392(1–2):90–105. https://doi.org/10.1016/j.mce.2014.05.008
Kajta M, Makarewicz D, Ziemińska E, Jantas D, Domin H, Lasoń W, Kutner A, Łazarewicz JW (2009b) Neuroprotection by co-treatment and post-treating with calcitriol following the ischemic and excitotoxic insult in vivo and in vitro. Neurochem Int 55(5):265–274. https://doi.org/10.1016/j.neuint.2009.03.010
Kajta M, Rzemieniec J, Litwa E, Lason W, Lenartowicz M, Krzeptowski W, Wojtowicz AK (2013) The key involvement of estrogen receptor β and G-protein-coupled receptor 30 in the neuroprotective action of daidzein. Neuroscience 238:345–360. https://doi.org/10.1016/j.neuroscience.2013.02.005
Kajta M, Rzemieniec J, Wnuk A, Lasoń W (2020) Triclocarban impairs autophagy in neuronal cells and disrupts estrogen receptor signaling via hypermethylation of specific genes. Sci Total Environ 701:134818. https://doi.org/10.1016/j.scitotenv.2019.134818
Kajta M, Trotter A, Lasoń W, Beyer C (2006) Impact of 17beta-estradiol on cytokine-mediated apoptotic effects in primary hippocampal and neocortical cell cultures. Brain Res 1116(1):64–74. https://doi.org/10.1016/j.brainres.2006.07.105
Kajta M, Wnuk A, Rzemieniec J, Lason W, Mackowiak M, Chwastek E, Staniszewska M, Nehring I, Wojtowicz AK (2019) Triclocarban disrupts the epigenetic status of neuronal cells and induces AHR/CAR-mediated apoptosis. Mol Neurobiol 56(5):3113–3131. https://doi.org/10.1007/s12035-018-1285-4
Kajta M, Wnuk A, Rzemieniec J, Litwa E, Lason W, Zelek-Molik A, Nalepa I, Rogóż Z, Grochowalski A, Wojtowicz AK (2017) Depressive-like effect of prenatal exposure to DDT involves global DNA hypomethylation and impairment of GPER1/ESR1 protein levels but not ESR2 and AHR/ARNT signaling. J Steroid Biochem Mol Biol 171:94–109. https://doi.org/10.1016/j.jsbmb.2017.03.001
Kajta M, Wójtowicz AK, Maćkowiak M, Lasoń W (2009a) Aryl hydrocarbon receptor-mediated apoptosis of neuronal cells: a possible interaction with estrogen receptor signaling. Neuroscience 158(2):811–822. https://doi.org/10.1016/j.neuroscience.2008.10.045
Kallio A, Guo T, Lamminen E, Seppänen J, Kangas L, Väänänen HK, Härkönen P (2008) Estrogen and the selective estrogen receptor modulator (SERM) protection against cell death in estrogen receptor alpha and beta expressing U2OS cells. Mol Cell Endocrinol 289(1–2):38–48. https://doi.org/10.1016/j.mce.2008.03.005
Khanna S, Stewart R, Gnyawali S, Harris H, Balch M, Spieldenner J, Sen CK, Rink C (2017) Phytoestrogen isoflavone intervention to engage the neuroprotective effect of glutamate oxaloacetate transaminase against stroke. FASEB J 31(10):4533–4544. https://doi.org/10.1096/fj.201700353
Kimelberg HK, Feustel PJ, Jin Y, Paquette J, Boulos A, Keller RW Jr, Tranmer BI (2000) Acute treatment with tamoxifen reduces ischemic damage following middle cerebral artery occlusion. NeuroReport 11(12):2675–2679. https://doi.org/10.1097/00001756-200008210-00014
Kitamura Y, Shimohama S, Kamoshima W, Ota T, Matsuoka Y, Nomura Y, Smith MA, Perry G, Whitehouse PJ, Taniguchi T (1998) Alteration of proteins regulating apoptosis, Bcl-2, Bcl-x, Bax, Bak, Bad, ICH-1 and CPP32, in Alzheimer’s disease. Brain Res 780(2):260–269. https://doi.org/10.1016/s0006-8993(97)01202-x
Li L, Xue J, Liu R, Li X, Lai L, Xie J, Huang Z, Huang C (2017) Neuroprotective effects of genistein-3′-sodium sulfonate on focal cerebral ischemia in rats. Neurosci Lett 646:43–48. https://doi.org/10.1016/j.neulet.2017.02.046
Liu R, Zhong X, Zeng J, Huang Z, Li X, Xiao H, Chen Q, Li D (2017) 3’-Daidzein sulfonate sodium inhibits neuronal apoptosis induced by cerebral ischemia-reperfusion. Int J Mol Med 39(4):1021–1028. https://doi.org/10.3892/ijmm.2017.2915
Locci E, Bazzano G, Demontis R, Chighine A, Fanos V, d’Aloja E (2020) Exploring perinatal asphyxia by metabolomics. Metabolites 10(4):141. https://doi.org/10.3390/metabo10040141
Lubián López DM (2022) Management of genitourinary syndrome of menopause in breast cancer survivors: an update. World J Clin Oncol 13(2):71–100. https://doi.org/10.5306/wjco.v13.i2.71
O’Barr S, Schultz J, Rogers J (1996) Expression of the protooncogene bcl-2 in Alzheimer’s disease brain. Neurobiol Aging 17(1):131–136. https://doi.org/10.1016/0197-4580(95)02024-1
Park HH, Han MH, Choi H, Lee YJ, Kim JM, Cheong JH, Ryu JI, Lee KY, Koh SH (2019) Mitochondria damaged by oxygen glucose deprivation can be restored through activation of the PI3K/Akt pathway and inhibition of calcium influx by amlodipine camsylate. Sci Rep 9(1):15717. https://doi.org/10.1038/s41598-019-52083-y
Patel S, Homaei A, Raju AB, Meher BR (2018a) Estrogen: The necessary evil for human health, and ways to tame it. Biomed Pharmacother 102:403–411. https://doi.org/10.1016/j.biopha.2018.03.078
Patel S, Homaei A, Raju AB, Meher BR (2018b) Estrogen: the necessary evil for human health, and ways to tame it. Biomed Pharmacother 102:403–411. https://doi.org/10.1016/j.biopha.2018.03.078
Przepiórska K, Wnuk A, Beyer C, Kajta M (2023) Amorfrutin B protects mouse brain neurons from hypoxia/ischemia by inhibiting apoptosis and autophagy processes through gene methylation- and miRNA-dependent regulation. Mol Neurobiol 60(2):576–595. https://doi.org/10.1007/s12035-022-03087-9
Raghava N, Das BC, Ray SK (2017) Neuroprotective effects of estrogen in CNS injuries: insights from animal models. Neurosci Neuroecon 6:15–29. https://doi.org/10.2147/NAN.S105134
Rutanen EM, Heikkinen J, Halonen K, Komi J, Lammintausta R, Ylikorkala O (2003) Effects of ospemifene, a novel SERM, on hormones, genital tract, climacteric symptoms, and quality of life in postmenopausal women: a double-blind, randomized trial. Menopause (new York, n.y.) 10(5):433–439. https://doi.org/10.1097/01.GME.0000063609.62485.27
Rzemieniec J, Litwa E, Wnuk A, Lason W, Gołas A, Krzeptowski W, Kajta M (2015) Neuroprotective action of raloxifene against hypoxia-induced damage in mouse hippocampal cells depends on ERα but not ERβ or GPR30 signalling. J Steroid Biochem Mol Biol 146:26–37. https://doi.org/10.1016/j.jsbmb.2014.05.005
Rzemieniec J, Litwa E, Wnuk A, Lason W, Kajta M (2018) Bazedoxifene and raloxifene protect neocortical neurons undergoing hypoxia via targeting ERα and PPAR-γ. Mol Cell Endocrinol 461:64–78. https://doi.org/10.1016/j.mce.2017.08.014
Rzemieniec J, Litwa E, Wnuk A, Lason W, Krzeptowski W, Kajta M (2016) Selective aryl hydrocarbon receptor modulator 3,3′-diindolylmethane impairs AhR and ARNT signaling and protects mouse neuronal cells against hypoxia. Mol Neurobiol 53(8):5591–5606. https://doi.org/10.1007/s12035-015-9471-0
Rzemieniec J, Wnuk A, Lasoń W, Bilecki W, Kajta M (2019) The neuroprotective action of 3,3′-diindolylmethane against ischemia involves an inhibition of apoptosis and autophagy that depends on HDAC and AhR/CYP1A1 but not ERα/CYP19A1 signaling. Apoptosis 24(5–6):435–452. https://doi.org/10.1007/s10495-019-01522-2
Sassone J, Maraschi A, Sassone F, Silani V, Ciammola A (2013) Defining the role of the Bcl-2 family proteins in Huntington′s disease. Cell Death Dis 4(8):e772. https://doi.org/10.1038/cddis.2013.300
Satou T, Cummings BJ, Cotman CW (1995) Immunoreactivity for Bcl-2 protein within neurons in the Alzheimer′s disease brain increases with disease severity. Brain Res 697(1–2):35–43. https://doi.org/10.1016/0006-8993(95)00748-f
Schreihofer DA, Redmond L (2009) Soy phytoestrogens are neuroprotective against stroke-like injury in vitro. Neuroscience 158(2):602–609. https://doi.org/10.1016/j.neuroscience.2008.10.003
Selvaraj UM, Zuurbier KR, Whoolery CW, Plautz EJ, Chambliss KL, Kong X, Zhang S, Kim SH, Katzenellenbogen BS, Katzenellenbogen JA, Mineo C, Shaul PW, Stowe AM (2018) Selective nonnuclear estrogen receptor activation decreases stroke severity and promotes functional recovery in female mice. Endocrinology 159(11):3848–3859. https://doi.org/10.1210/en.2018-00600
Shichita T, Hasegawa E, Kimura A, Morita R, Sakaguchi R, Takada I, Sekiya T, Ooboshi H, Kitazono T, Yanagawa T, Ishii T, Takahashi H, Mori S, Nishibori M, Kuroda K, Akira S, Miyake K, Yoshimura A (2012) Peroxiredoxin family proteins are key initiators of post-ischemic inflammation in the brain. Nat Med 18(6):911–917. https://doi.org/10.1038/nm.2749
Soane L, Kahraman S, Kristian T, Fiskum G (2007) Mechanisms of impaired mitochondrial energy metabolism in acute and chronic neurodegenerative disorders. J Neurosci Res 85(15):3407–3415. https://doi.org/10.1002/jnr.21498
Sulejczak D, Czarkowska-Bauch J, Macias M, Skup M (2004) Bcl-2 and Bax proteins are increased in neocortical but not in thalamic apoptosis following devascularizing lesion of the cerebral cortex in the rat: an immunohistochemical study. Brain Res 1006(2):133–149. https://doi.org/10.1016/j.brainres.2004.01.063
Unkila M, Kari S, Yatkin E, Lammintausta R (2013) Vaginal effects of ospemifene in the ovariectomized rat preclinical model of menopause. J Steroid Biochem Mol Biol 138:107–115. https://doi.org/10.1016/j.jsbmb.2013.04.004
Vivien D, Gauberti M, Montagne A, Defer G, Touzé E (2011) Impact of tissue plasminogen activator on the neurovascular unit: from clinical data to experimental evidence. J Cereb Blood Flow Metab 31(11):2119–2134. https://doi.org/10.1038/jcbfm.2011.127
Wakade C, Khan MM, De Sevilla LM, Zhang QG, Mahesh VB, Brann DW (2008) Tamoxifen neuroprotection in cerebral ischemia involves attenuation of kinase activation and superoxide production and potentiation of mitochondrial superoxide dismutase. Endocrinology 149(1):367–379. https://doi.org/10.1210/en.2007-0899
Wang J, Green PS, Simpkins JW (2001) Estradiol protects against ATP depletion, mitochondrial membrane potential decline and the generation of reactive oxygen species induced by 3-nitroproprionic acid in SK-N-SH human neuroblastoma cells. J Neurochem 77(3):804–811. https://doi.org/10.1046/j.1471-4159.2001.00271.x
Wang X, Zhao L, Zhang Y, Ma W, Gonzalez SR, Fan J, Kretschmer F, Badea TC, Qian HH, Wong WT (2017) Tamoxifen provides structural and functional rescue in murine models of photoreceptor degeneration. J Neurosci 37(12):3294–3310. https://doi.org/10.1523/JNEUROSCI.2717-16.2017
Wnuk A, Kajta M (2017) Steroid and xenobiotic receptor signalling in apoptosis and autophagy of the nervous system. Int J Mol Sci 18(11):2394. https://doi.org/10.3390/ijms18112394
Wnuk A, Przepiórska K, Pietrzak BA, Kajta M (2021a) Posttreatment strategy against hypoxia and ischemia based on selective targeting of nonnuclear estrogen receptors with PaPE-1. Neurotox Res 39(6):2029–2041. https://doi.org/10.1007/s12640-021-00441-y
Wnuk A, Przepiórska K, Pietrzak BA, Kajta M (2021b) Post-treatment with amorfrutin B evokes PPARγ-mediated neuroprotection against hypoxia and ischemia. Biomedicines 9(8):854. https://doi.org/10.3390/biomedicines9080854
Wnuk A, Przepiórska K, Rzemieniec J, Pietrzak B, Kajta M (2020) Selective targeting of non-nuclear estrogen receptors with PaPE-1 as a new treatment strategy for Alzheimer's Disease. Neurotox Res 38(4):957–966. https://doi.org/10.1007/s12640-020-00289-8
Wnuk A, Rzemieniec J, Lasoń W, Krzeptowski W, Kajta M (2018) Apoptosis induced by the UV filter benzophenone-3 in mouse neuronal cells is mediated via attenuation of Erα/Pparγ and stimulation of Erβ/Gpr30 signaling. Mol Neurobiol 55(3):2362–2383. https://doi.org/10.1007/s12035-017-0480-z
Wnuk A, Rzemieniec J, Litwa E, Lasoń W, Krzeptowski W, Wójtowicz AK, Kajta M (2016) The crucial involvement of retinoid X receptors in DDE neurotoxicity. Neurotox Res 29(1):155–172. https://doi.org/10.1007/s12640-015-9572-6
Wnuk A, Rzemieniec J, Staroń J, Litwa E, Lasoń W, Bojarski A, Kajta M (2019) Prenatal exposure to benzophenone-3 impairs autophagy, disrupts RXRs/PPARγ signaling, and alters epigenetic and post-translational statuses in brain neurons. Mol Neurobiol 56(7):4820–4837. https://doi.org/10.1007/s12035-018-1401-5
Ye M, Wu H, Li S (2021) Resveratrol alleviates oxygen/glucose deprivation/reoxygenation-induced neuronal damage through induction of mitophagy. Mol Med Rep 23(1):73. https://doi.org/10.3892/mmr.2020.11711
Zhao TZ, Shi F, Hu J, He SM, Ding Q, Ma LT (2016) GPER1 mediates estrogen-induced neuroprotection against oxygen-glucose deprivation in the primary hippocampal neurons. Neuroscience 328:117–126. https://doi.org/10.1016/j.neuroscience.2016.04.026
Funding
This study was financially supported by the statutory fund of the Maj Institute of Pharmacology Polish Academy of Sciences, Krakow, Poland.
Author information
Authors and Affiliations
Contributions
B. A. P.: data curation, investigation, methodology, and writing—original draft; A. W.: data curation, formal analysis, investigation, methodology, validation, and writing—original draft; K. P.: data curation, investigation, methodology, validation, and writing—original draft; A. Ł.: investigation; M. K.: conceptualization, funding acquisition, methodology, project administration, supervision, and writing—original draft. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All experiments were conducted according to the principles of the Three Rs in compliance with the European Union Legislation (Directive 2010/63/EU, amended by Regulation (EU) 2019.1010) and the ethical standards in the Guide for the Care and Use of Laboratory Animals (NIH).
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pietrzak, B.A., Wnuk, A., Przepiórska, K. et al. Posttreatment with Ospemifene Attenuates Hypoxia- and Ischemia-Induced Apoptosis in Primary Neuronal Cells via Selective Modulation of Estrogen Receptors. Neurotox Res 41, 362–379 (2023). https://doi.org/10.1007/s12640-023-00644-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-023-00644-5