Abstract
The COVID-19 pandemic placed a significant burden on the German healthcare system. Based on the experience of severe disease progression of the SARS-CoV‑2 infection from neighboring European countries in the early 2020s, with ICU overload and high mortality rates, efforts were made in Germany to increase the capacity of available ICU beds. Subsequently, all documentation and reporting focused on the ICU capacities for COVID-19 patients. It was hypothesized that mainly a few large hospitals provided care for the majority of COVID-19 patients. The COVID-19 Registry RLP of Rhineland-Palatinate documented SARS-CoV‑2 inpatients from daily mandatory queries of all hospitals throughout the pandemic from April 2020 to March 2023, distinguishing between patients in ICUs and normal wards. In its 18th Corona Ordinance, the state government required all hospitals to participate in the care of SARS-CoV‑2 inpatients. We investigated the participation of hospitals at different levels of care in Rhineland-Palatinate in the management of the COVID-19 pandemic. Nine pandemic waves were documented during the pandemic and exemplary data on the respective pandemic peaks were evaluated. A distinction was made between the burden on hospitals at different levels of care: primary care hospitals, standard care hospitals, specialty hospitals, and maximal care hospitals. Analysis of the data showed that all hospital types participated equally in the care of SARS-CoV-2 patients. The requirement of the Ministry of Health of Rhineland-Palatinate to provide at least 20% of the available capacity was met by all levels of care and there were no disparities between hospitals of different levels of care in the management of the pandemic.
Hospitals at all levels of care participated equally in the care of SARS-CoV‑2 inpatients and thus contributed significantly to the management of the pandemic in Rhineland-Palatinate.
Zusammenfassung
Die COVID-19-Pandemie stellte eine erhebliche Belastung für das deutsche Gesundheitssystem dar. Aufgrund der Erfahrungen schwerer Krankheitsverläufe der SARS-CoV-2-Infektion aus europäischen Nachbarländern Anfang des Jahres 2020 mit Überlastungen der Intensivstationen und einer hohen Sterblichkeit wurden in Deutschland Anstrengungen unternommen, die Kapazitäten zur Verfügung stehender Intensivbetten zu erhöhen. Sämtliche Dokumentationen sowie die Berichterstattungen konzentrierten sich fortan auf die für die COVID-19-Patienten genutzten und frei verfügbaren Intensivkapazitäten. Dabei wurde wiederholt die Hypothese aufgestellt, dass wenige große Krankenhäuser die Mehrzahl der COVID-19-Patienten versorgt hätten. Das COVID-19-Register des Bundeslandes Rheinland-Pfalz (RLP) hat über die gesamte Pandemiedauer von April 2020 bis März 2023 die stationären SARS-CoV-2-Patienten in täglichen verpflichtenden Abfragen aller Krankenhäuser dokumentiert, differenziert auch zwischen Patienten auf Intensivstationen und Normalstationen. Die Landesregierung hatte in ihrer 18. Corona-Verordnung alle Krankenhäuser zur Beteiligung an der Versorgung der stationären SARS-CoV-2 Patienten verpflichtet. Wir haben die Beteiligung der Krankenhäuser der unterschiedlichen Versorgungsstufen in Rheinland-Pfalz an der Bewältigung der COVID-19-Pandemie untersucht. Es wurden insgesamt 9 Pandemiewellen über den Gesamtzeitraum der Pandemie dokumentiert und exemplarische Daten zu den jeweiligen Pandemieapitzen wurden ausgewertet. Dabei wurde zwischen der Belastung der Krankenhäuser unterschiedlicher Versorgungsstufen unterschieden: Krankenhäuser der Regelversorgung, Krankenhäuser der Grundversorgung, Schwerpunktkrankenhäuser und Krankenhäuser der Maximalversorgung. Die Auswertung der Daten zeigte, dass alle Krankenhaustypen proportional in gleicher Weise an der Versorgung der SARS-CoV-2 Patienten teilgenommen hatten. Die Vorgabe des Gesundheitsministerium von RLP, mindestens 20 % der verfügbaren Kapazitäten zur Verfügung zu stellen, wurde von allen Versorgungsklassen eingehalten, und es gab keine Ungleichverteilungen im Management der Pandemie. Krankenhäuser aller Versorgungsstufen haben gleichermaßen an der Versorgung der stationären SARS-CoV-2-Patienten teilgenommen und damit maßgeblich zum Management der Pandemie in Rheinland-Pfalz beigetragen.
Similar content being viewed by others
The COVID-19 pandemic has placed a significant strain on the healthcare system worldwide since it began in 2019 in China. Due to the severity of the SARS-CoV‑2 infection at the beginning of the pandemic and the reports of overloading of the healthcare systems in neighboring European countries such as Italy, there was a significant focus on maintaining sufficient intensive care capacity to care for the feared large number of patients who might require intensive care. This focus on critical care in the initial waves of the pandemic created the impression that only a few hospitals would care for the vast majority of SARS-CoV-2 patients in Germany.
To guarantee adequate capacities for the treatment of SARS-CoV-2 patients who needed hospital care in Rhineland-Palatinate, the government of Rhineland-Palatinate obliged all hospitals that were part of the 2019–2025 Hospital Plan and were registered and listed in the Registry of the German Interdisciplinary Association for Intensive Care and Emergency Medicine (DIVI Registry) to provide intensive care beds with ventilation to the extent necessary in each case, but at least 20% of their respective capacities, and the treatment capacities of normal care on isolation wards to the extent necessary in each case, including the staff necessary for the care and treatment of patients with COVID-19 disease at all times (in § 17 of the 18th Corona Control Ordinance Rhineland-Palatinate: 18th CoBeLVO of 20 March 2021; [1]). This order focused not only on intensive care capacities but also on COVID-19 care on normal wards, paying attention to the overall burden of the disease for inpatient care.
Consequently, the aim of our analysis was to examine the participation of hospitals of different levels of care in Rhineland-Palatinate in the management of the COVID-19 pandemic.
Methods
The Institut für Herzinfarktforschung (IHF, Institute for Heart Attack Research) initiated the COVID-19 Registry for Rhineland-Palatine in April 2020 with the support of the Ministry of Social Affairs, Labor, Health and Demography (MSAGD) and from May 2021 with the support of the Ministry of Science and Health (MWG; [2]). Part of this prospective registry was the documentation of the number of patients hospitalized for the treatment of SARS-CoV‑2 infections and the occupancy rates in the intensive care units, which were also queried by the German DIVI registry. In addition to the latter, the occupancy rates on normal care wards in all hospitals in Rhineland-Palatinate had to be reported through daily mandatory queries from 8 April 2020 to 31 March 2023, in order to provide a better picture of the real pandemic burden on the healthcare system beyond the focus on intensive care capacities only [3, 4].
All hospitals included in the 2019–2025 Hospital Plan of Rhineland-Palatinate participated in the data acquisition over the full period of the COVID-19 pandemic (Fig. 1). In the 2019–2025 Hospital Plan, all hospitals were assigned to four different levels of care: (a) primary care hospitals, (b) standard care hospitals, (c) specialty care hospitals, and (d) maximal care hospitals. A list with the assignment of all hospitals in Rhineland-Palatinate to the four levels of care is provides as electronic supplementary material. We documented the occupancies of intensive care units and normal wards for the four different levels of care in Rhineland-Palatinate throughout the entire COVID-19 pandemic.
Results
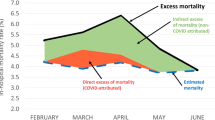
Volume of SARS-CoV-2 patients hospitalized in Rhineland-Palatinate
During the entire COVID-19 pandemic with a total of nine waves between April 2020 and March 2023, different numbers of SARS-CoV-2 patients required inpatient treatment in Rhineland-Palatinate. Figure 2 shows the daily number of hospitalized SARS-CoV-2 patients differentiating between intensive and normal care required. At the peak of the first pandemic wave, only 394 patients received inpatient treatment, whereas in the second pandemic wave in December 2020 a maximum of 1151 patients were hospitalized for SARS-CoV‑2 infections. In the course of the pandemic, multiple waves exceeded these numbers, with the highest number of patients by far being hospitalized during wave 7 in October 2022 (Table 1). During the pandemic the number of patients requiring intensive care decreased, whereas the number of patients requiring normal care on isolation wards increased over time. The number of patients on normal wards exceeded the number in intensive care units by two- to fourfold at the beginning of the pandemic, and by eight- to 15-fold at the end of the pandemic with milder courses of the infections due to mutation shifts of the virus as well as to the improved vaccination status of the patients.
SARS-CoV-2 treatment by hospitals of different levels of care
All 114 hospitals were involved in the care of SARS-CoV‑2 inpatients in Rhineland-Palatinate throughout the entire COVID-19 pandemic (Fig. 3). Hospitals of all care levels—primary care, standard care, specialty care, and maximal care—participated equally in the management of SARS-CoV-2 patients (Fig. 4). The 46 standard care hospitals (49% of all hospitals) together with the seven maximal care hospitals (6% of all hospitals) managed approximately 60% of all SARS-CoV-2 patients requiring intensive care throughout all of the waves of the pandemic (Table 2). This is due to the fact that, in absolute numbers, standard care and maximal care hospitals had the most operable intensive care beds available in Rhineland-Palatinate throughout the COVID pandemic. The involvement of hospitals in the intensive care of SARS-CoV-2 patients should be considered in relation to the actual operable intensive care beds. Primary care hospitals provided intensive care on average in 18.4%, standard care hospitals in 31.6%, specialty care hospitals in 21.5%, and maximal care hospitals in 28.5% of their actual operable intensive care beds during all the pandemic waves. Up to 60% of SARS-CoV-2 patients requiring in-hospital care on normal isolation wards were treated in primary care and standard care hospitals (Table 2). In Rhineland-Palatinate all hospitals at different levels of care participated proportionally in the management of the COVID-19 pandemic and fulfilled the expected provision of at least 20% of the available intensive care capacities for the SARS-CoV-2 patients in Rhineland-Palatinate (Table 3).
Discussion
Due to the scale of the COVID-19 pandemic, the participation of all hospitals was necessary for the care of SARS-CoV-2 patients. Shortly before the COVID-19-pandemic, which started in China in December 2019, the Bertelsmann Foundation published a report on the future design of the hospital landscape in the Federal Republic of Germany. It suggested a significant reduction in the number of hospitals in Germany [5]. Since this publication, the proposal of restructuring the hospital care system in Germany and the closure of approximately 50% of German hospitals has been hotly debated. Particularly during the COVID-19 pandemic period, it was repeatedly reported in the media that mainly large hospitals would bear the main burden of caring for hospitalized SARS-CoV-2 patients in Germany. In view of the fear of shortages of intensive care capacities during the pandemic, the Bertelsmann Foundation stated that their proposal should not include a reduction in intensive care beds.
The Scientific Institute of the German healthcare provider AOK (WidO = Wissenschaftliches Institut der AOK [Allgemeine Ortskrankenkassen]) reported on the management of the COVID-19 pandemic in Germany and its impact on the country’s federal healthcare system [6]. In 2020, 24% of hospitals had treated 66% of all hospitalized patients with SARS-CoV‑2 infections [7]. This analysis included SARS-CoV-2 patients who were insured by the AOK only. It described the dominance of large hospitals in the care of inpatients with SARS-CoV‑2, which did not apply to Rhineland-Palatinate, however. All hospitals in Rhineland-Palatinate participated proportionally in the care of the large number of SARS-CoV-2 patients during the entire COVID-19 pandemic between April 2020 and March 2023.
Conclusion
The COVID-19 Registry of Rhineland-Palatinate provided an important prospective database for real-time monitoring of the course of the COVID-19 pandemic and the allocation of healthcare capacities for the best possible management of SARS-CoV-2 patients requiring hospital care. It was used as an important central instrument by the Ministry for Science and Healthcare (MWG) in Rhineland-Palatinate in order to provide the basis for creating networking structures and stringent planning of the COVID-19 crisis.
References
Achtzehnte Corona-Bekämpfungsverordnung Rheinland-Pfalz (18. CoBeLVO) vom 20. März 2021. https://Corona.rlp.de/fileadmin/coroona/210331_18._CoBeLVO_1AEndVO_konsolidierte_Fassung.pdf. Accessed: 5 May 2023
Gitt AK, Bernhardt A, Zahn R et al (2020) The COVID-19 Registry in Rhineland-Palatinate in the context of international registry activities documenting COVID-19 outcomes. Herz 45(4):316–318
Gitt AK, Lober C, Neumer A, Schneider S et al (2022) Krankenhäuser an den Grenzen der Versorgung. Dtsch Arztebl 119(43):A 1846–A 1850
Gitt AK, Lober C, Bernhardt A et al (2022) Coronabelastung auf den Normalstationen stärker beachten: Die Fokussierung auf die Intensivmedizin in der COVID-19-Pandemie ist unzureichend für die Beurteilung der Auslastung des Krankenhaussystems. Dtsch Arztebl 119(6):221–224
Loos S, Albrecht M, Zich K (2019) Zukunftsfähige Krankenhausversorgung, Simulation und Analyse einer Neustrukturierung der Krankenhausversorgung am Beispiel einer Versorgungsregion in Nordrhein-Westfalen. Bertelsmann https://doi.org/10.11586/2019042
Klauber J, Wasem J, Beibers A et al (2022) Krankenhaus-Report 2022: Patientenversorgung während der Pandemie https://doi.org/10.1007/978-3-662-64685-4. ISBN 978-3-662-64685‑4 (eBook)
Mostert C, Hentschker C, Scheller-Kreinsen D et al (2021) Auswirkungen der Covid-19-Pandemie auf die Krankenhausleistungen im Jahr 2020. In: Klauber J, Wasem J, Beivers A, Mostert C (eds) Krankenhaus-Report 2021. Springer, Berlin, Heidelberg https://doi.org/10.1007/978-3-662-62708-2_16
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.K. Gitt, M. Horack, S. Schneider, U. Zeymer and R. Zahn declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Supplementary Information
Rights and permissions
About this article
Cite this article
Gitt, A.K., Horack, M., Schneider, S. et al. Management of the COVID-19 pandemic in Rhineland-Palatinate hospitals of all levels of care. Herz 48, 184–189 (2023). https://doi.org/10.1007/s00059-023-05187-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-023-05187-1