Abstract
Background
In the neonatal period, cardiac hypertrophy (CH) has been commonly associated with hyperinsulinemic pathologies, and the first case of CH in an extremely preterm infant treated with insulin infusion has recently been reported. To confirm this association, we report a case series of patients who developed CH after insulin therapy.
Methods
Infants with gestational age < 30 weeks and birth weight < 1500 g, born from November 2017 to June 2022, were studied if they developed hyperglycemia requiring treatment with insulin and had echocardiographic diagnosis of CH.
Results
We studied 10 extremely preterm infants (24.3 ± 1.4 weeks) who developed CH at a mean age of 124 ± 37 h of life, 98 ± 24 h after the initiation of insulin therapy. All surviving patients had resolution of CH at discharge, while three of four (75%) of the deceased patients had persistent CH.
Conclusions
Our case series supports the association between the development of CH and insulin therapy in extremely preterm infants and suggests further caution and the need for echocardiographic monitoring when treating these fragile patients with insulin.
Similar content being viewed by others
This is the first case series that reports the association between insulin therapy and the development of cardiac hypertrophy (CH). |
All patients were extremely preterm infants and CH resolved in seven of these patients and persisted in three patients who deceased. |
This association suggests great caution when treating these fragile patients with insulin and the need for echocardiographic monitoring. |
1 Introduction
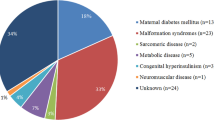
Hypertrophic cardiomyopathy (HCM) and cardiac hypertrophy (CH) are rare pathologies in infants that are often confused in the literature, likely because they cannot be clearly distinguished by echocardiography [1]. In fact, both present thickening of one or both of the ventricular walls, including the interventricular septum with or without systolic and diastolic dysfunction [2]. On the other hand, the histologic pattern of HCM is characterized by the disruption of the myocardial structures, including disarray of the muscle fibers, intramyocardial fibrosis, and interstitial collagen depositions [3,4,5], which differs from diffuse hyperplasia of cardiomyocytes with normal configuration that is observed in CH [2]. Differential diagnosis between HCM and CH is very important from a prognostic point of view. In fact, HCM has been reported as associated with severe pathologies with poor prognosis, such as sarcomeric protein, lysosomal storage, and mitochondrial diseases, disorders of glycogen and fatty acids metabolism, and malformation syndromes [6]. Conversely, although CH can also be associated with severe pathologies with poor prognosis (i.e., leprechaunism, congenital lipodystrophy, etc.), in the neonatal period it is more commonly associated with pathologies with a more benign prognosis, such as hyperinsulinism due to maternal diabetes (infants of diabetic mothers [IDMs]), congenital hyperinsulinism (previously called ‘nesidioblastosis’) [1], and insulin treatment for hyperglycemia in very preterm infants [7]. In these cases, CH often resolves spontaneously and its echocardiographic pattern progressively decreases to normal, although some patients may require β-blocker therapy and/or have a less favorable prognosis when comorbidities exist, as happens in very preterm infants [7, 8].
Recently, Salvatori et al. reported the first case of CH in an extremely preterm infant who was treated with insulin infusion for a persistent hyperglycemia [7]. They found that CH disappeared after insulin discontinuation and the patient had a good cardiologic outcome at discharge. However, we hypothesized that CH associated with insulin treatment may be more frequent than expected in preterm infants and that its management may be more complex and with less favorable prognosis than previously reported [7].
Thus, the objective of this study was to report the clinical course of a cohort of extremely preterm infants who were treated with insulin for hyperglycemia and developed CH, detailing data that can support the previous case report [7] and confirm that CH can be associated with insulin therapy in preterm infants.
2 Patient and Methods
2.1 Patient Population
This retrospective study was carried out at the neonatal intensive care unit (NICU) of the Careggi University Hospital of Florence from November 2017 to June 2022 following approval by the Ethics Committee. Infants with gestational age (GA) < 30 weeks and birth weight (BW) < 1500 g were studied if they developed hyperglycemia requiring treatment with insulin and CH. Exclusion criteria were treatment with fewer than two doses of insulin and for less than 48 h, death before the first week of life, and postnatal treatment with steroids (i.e., dexamethasone) since CH is a well-known adverse effect of steroids.
2.2 Study Design
All infants followed the same enteral nutrition protocol: trophic feeding was initiated within 24 h after birth and was continued at 20–40 mL/kg/day as tolerated for up to 5 days. Subsequently, the amount was increased by 20 mL/kg every day if enteral nutrition was tolerated. The goals for enteral nutrition were 150 mL/kg/day and 120 kcal/kg/day. Human milk was enriched with a fortifier when enteral feeding of 90–100 mL/kg/day was reached. Parenteral nutrition was started with the infusion of a standard glucose and amino acid solution as soon as central venous access was obtained, while in the following days lipids, electrolytes and other components (i.e., vitamins and trace elements) were added as required. Glucose intake was 4–8 mg/kg/min [9] and hyperglycemia was defined as a glucose level measurement > 180 mg/dL [10, 11]. Glucose concentrations were measured on a blood gas analyzer (ABL 90 Flex, Radiometer Ltd, Copenhagen, Denmark) two to three times a day on the basis of patients’ clinical condition and biochemical indications. Hyperglycemia was initially managed by reducing the glucose infusion rate without falling below 4 mg/kg/min, and when this was not sufficient, insulin therapy was started to maintain a blood glucose concentration of 60–180 mg/dL. Insulin (Humulin R®, Eli Lilly Italia S.p.A., Sesto Fiorentino, Italy) was administered as an intravenous bolus (0.1–0.2 UI/kg) or intravenous continuous infusion (0.01–0.1 UI/kg/h) when hyperglycemia was refractory to two consecutive insulin boluses.
CH was defined by the echocardiographic evidence of diastolic left ventricular wall thickness or diastolic septal thickness ≥ 2 standard deviations (SDs) above the mean (Z score ≥ 1.96; corrected for age, sex, and body size) [12,13,14]. Echocardiography was repeated every 24 h during the first week of life and then weekly or more frequently as suggested by the clinical conditions. Cardiac ultrasounds were performed by expert personnel, specifically a pediatric cardiologist (VV) or a neonatologist (IC, CP, SP) who has achieved adequate expertise in newborn heart ultrasound.
Management of infants with CH included careful echocardiographic follow-up and, in symptomatic infants, supportive therapy (i.e., non-invasive and invasive respiratory support), increased intravenous fluid administration [15], and/or propranolol or other β-blockers to improve cardiac output [2, 7, 8], as required.
2.3 Data Collection and Analysis
The following data were recorded for each studied infant: GA, BW, sex, antenatal steroids, mode of delivery, age at onset of hyperglycemia, peak level of glycemia, age at the beginning of insulin therapy, infant of a diabetic mother, need for non-invasive and invasive respiratory support, need for inotropes, peak level of glycemia, age at the beginning of insulin therapy, mode of insulin administration (bolus and/or continuous infusion), cumulative dose of insulin, age at diagnosis of CH, diastolic septal thickness, need for increased intravenous fluid administration and/or propranolol for CH, outcome of CH at discharge, occurrence of patent ductus arteriosus (PDA) requiring medical treatment, bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), sepsis, intraventricular hemorrhage (IVH), retinopathy of prematurity (ROP), mortality, and duration of stay in hospital. BPD was defined as oxygen requirement at 36 weeks of postmenstrual age [16]. PDA was diagnosed by echocardiography; NEC was defined as Bell’s stage 2 or higher [17]; and sepsis was defined as positive blood culture. IVH was classified according to the Papile classification scheme [18], and ROP was graded according to the international classification of ROP [19].
Patients’ clinical characteristics, data on hyperglycemia, its treatment with insulin therapy, and development, treatment and outcome of CH were described as mean ± SD, and rate and percentage.
3 Results
We studied 10 preterm infants who were treated with insulin for hyperglycemia and then developed CH diagnosed by echocardiography. This group represents 3% (10/329) of infants with similar GA and BW values admitted in our NICU.
During the study period, only one patient who met the inclusion and exclusion criteria was treated with insulin for hyperglycemia without developing CH, while 54 patients developed hyperglycemia that did not require insulin therapy and 4 (7%) developed CH.
All patients included in the study were extremely preterm infants (24.3 ± 1.4 weeks of GA) with extremely low BW (740 ± 216 g). Consistently, the infants were very ill, as evidenced by the high frequency of mechanical ventilation (100%), need for inotropes (80%), complications of prematurity, and mortality (40%) (Table 1).
Diagnosis of hyperglycemia was early (21 ± 27 h) and was followed by the beginning of insulin therapy some hours later (28 ± 31 h) because it was initially managed by reducing the glucose infusion rate. Insulin bolus therapy was attempted, with most patients (70%) needing continuous infusion. The duration of insulin therapy was 110 ± 79 h and the cumulative dose was 1.48 ± 1.40 UI/kg (Table 2).
CH was diagnosed at a mean age of 124 ± 37 h of life, 98 ± 24 h after the initiation of insulin therapy. Mean diastolic septal thickness was 4.5 ± 1.2 mm, with a Z score of 3.2 ± 1.0 [14]. Four patients developed a mild–moderate left ventricular outflow obstruction (three subsequently died) and were treated with an increase in intravenous fluid administration, while none required β-blockers. All surviving patients had resolution of CH, which occurred after 21 ± 31 days (range 5–80). Two infants died as a result of refractory respiratory failure (one with CH) and two as a result of late-onset sepsis (both with CH).
4 Discussion
In this retrospective study, we report the first case series of 10 extremely preterm infants who were treated with insulin for hyperglycemia and developed CH, and detail their management and outcome. Although these infants represent a low percentage (3%) of very preterm infants admitted to our NICU, we found in the severity of their prematurity and their clinical conditions a trait that makes them worthy of great attention.
Currently, CH is not considered a possible adverse effect of insulin therapy in the neonatal period [1, 20], and particularly not in extremely preterm infants, although a relationship between CH and hyperinsulinism has been reported in several pathologies, such as in IDMs [21, 22], congenital hyperinsulinism [23], leprechaunism [24], and congenital lipodystrophy [25]. On the other hand, this correlation appears to be not only possible but also rational and predictable considering the reported antenatal effects of insulin on fetal heart development that can ideally be observed in IDMs [21]. In fact, up to 40% of IDMs develop CH [21], and one of its most important etiological factors is fetal hyperinsulinemia induced by the chronic hyperglycemia that causes hypertrophy of the insulin-sensitive tissues, including the heart, and increased expression and affinity of insulin receptors [26]. Thus, chronic fetal hyperinsulinemia can trigger CH by increasing myocardial nuclei and cell number, and inducing hypertrophy of myocardial fibers by promoting protein and fat synthesis in cardiomyocytes [27]. These insulin effects could be potentiated in extremely preterm infants by the high fetal proliferative capacity of immature cardiomyocytes [28]. Moreover, this hypothesis is consistent with the fact that 9 of our 10 patients were born between 23 and 25 weeks GA, they developed hyperglycemia in the first days of life, and CH developed shortly after the beginning of insulin therapy.
Management of CH in very preterm infants is not well-established and consists, as with term infants, of supportive therapy, increased intravenous fluid administration [15], and/or propranolol or other β-blocker treatment [2, 7, 8], on the basis of patient’s clinical status and echocardiographic findings. However, our case series and the previous case report [7] suggest that CH spontaneously resolves at a later time in most patients without a specific treatment, and it is possible that a resolution occurs in all surviving patients. Nevertheless, the development of CH in otherwise severely ill extremely preterm infants can further complicate their management and worsen their outcome, for example by limiting or precluding the treatment with steroids of BPD [28].
4.1 Limitations
Limitations of our study include its retrospective design and the small size of our population, which did not allow us to evaluate a possible correlation between cumulative dose of insulin and severity of CH, although CH in response to insulin could be independent of dose or treatment duration, as occurs for CH associated with postnatal steroid treatment [29, 30]. Moreover, the blood level of insulin was not measured and therefore a possible correlation between elevated insulinemia and the development of CH was not evaluated. However, our data are exhaustive and have recently been collected in an homogeneous population over a short period of time, and can therefore support the publication of further studies on this issue.
5 Conclusion
This is the first case series of extremely preterm infants who developed CH in association with insulin therapy for hyperglycemia. In agreement with the previous case report [7], CH spontaneously resolved in most patients without any treatment. Further studies are necessary to confirm that CH can be an adverse effect of insulin therapy in preterm infants, and, if so, further caution will be required when treating these fragile patients with insulin.
References
Paauw ND, Stegeman R, de Vroede MAMJ, et al. Neonatal cardiac hypertrophy: the role of hyperinsulinism—a review of literature. Eur J Pediatr. 2020;179:39–50.
Huang T, Kelly A, Becker SA, et al. Hypertrophic cardiomyopathy in neonates with congenital hyperinsulinism. Arch Dis Child Fetal Neonatal Ed. 2013;98:F351–4.
Maron BJ, Roberts WC. Quantitative analysis of cardiac muscle cell disorganization in the ventricular septum of patients with hypertrophic cardiomyopathy. Circulation. 1979;59:689–706.
Sutton MGSJ, Lie JT, Anderson KR, et al. Histopathological specificity of hypertrophic obstructive cardiomyopathy. Myocardial fibre disarray and myocardial fibrosis. Br Heart J. 1980;44:433–43.
Shirani J, Pick R, Roberts WC, Maron BJ. Morphology and significance of the left ventricular collagen network in young patients with hypertrophic cardiomyopathy and sudden cardiac death. J Am Coll Cardiol. 2000;35:36–44.
Moak JP, Kaski JP. Hypertrophic cardiomyopathy in children. Heart. 2012;98:1044–54.
Salvatori G, Brindisi G, Colantonio M, et al. Cardiac hypertrophy and insulin therapy in a pre-term newborn: is there a relationship? Ital J Pediatr. 2022;48:24.
Codazzi AC, Ippolito R, Novara C, et al. Hypertrophic cardiomyopathy in infant newborns of diabetic mother: a heterogeneous condition, the importance of anamnesis, physical examination and follow-up. Ital J Pediatr. 2021;47:197.
Mesotten D, Joosten K, van Kempen A, et al. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: carbohydrates. Clin Nutr. 2018;37:2337–43.
Tottman AC, Alsweiler JM, Bloomfield FH, et al. Relationship between measures of neonatal glycemia, neonatal illness, and 2-year outcomes in very preterm infants. J Pediatr. 2017;188:115–21.
Zamir I, Tornevi A, Abrahamsson T, et al. Hyperglycemia in extremely preterm infants-insulin treatment, mortality and nutrient intakes. J Pediatr. 2018;200:104-10.e1.
Gersh BJ, Maron BJ, Bonow RO, et al. ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Thorac Cardiovasc Surg. 2011;142:e153-203.
Chubb H, Simpson JM. The use of Z-scores in paediatric cardiology. Ann Pediatr Cardiol. 2012;5:179–84.
Choudhry S, Salter A, Cunningham TW, et al. Normative left ventricular m-mode echocardiographic values in preterm infants up to 2 kg. J Am Soc Echocardiogr. 2017;30:781–9.
Robinson B, Eshaghpour E, Ewing S, et al. Hypertrophic obstructive cardiomyopathy in an infant of a diabetic mother: support by extracorporeal membrane oxygenation and treatment with beta-adrenergic blockade and increased intravenous fluid administration. ASAIO J. 1998;44:845–7.
Ehrenkranz RA, Walsh MC, Vohr BR, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal necrotizing enterocolitis: therapeutic decisions based on clinical staging. Ann Surg. 1978;187:1–7.
Papile LS, Burstein J, Burstein R, et al. Incidence and evolution of the subependymal intraventricular hemorrhage: a study of infants weighing less than 1500 grams. J Pediatr. 1978;92:529–34.
The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Beardsall K, Vanhaesebrouck S, Ogilvy-Stuart AL, et al. Early insulin therapy in very-low-birth-weight infants. N Engl J Med. 2008;359:1873–84.
Al-Biltagi M, El Razaky O, El Amrousy D. Cardiac changes in infants of diabetic mothers. World J Diabetes. 2021;12:1233–47.
Bolin EH, Spray BJ, Mourani PM, et al. Mortality among infants of diabetic mothers with hypertrophic cardiomyopathy. J Matern Fetal Neonatal Med. 2022;19:1–7.
Massin MM, Van Elmbt G, Soyeur D. Reversible hypertrophic cardiomyopathy in congenital hyperinsulinism. Acta Cardiol. 1999;54:359–61.
Rosenberg AM, Haworth JC, Degroot GW, et al. A case of leprechaunism with severe hyperinsulinemia. Am J Dis Child. 1980;134:170–5.
Rheuban KS, Blizzard RM, Parker MA, et al. Hypertrophic cardiomyopathy in total lipodystrophy. J Pediatr. 1986;109:301–2.
Boucher J, Kleinridders A, Kahn CR. Insulin receptor signaling in normal and insulin-resistant states. Cold Spring Harb Perspect Biol. 2014;6: a009191.
Pabis JS, Schneider L, Stoll LF, et al. Heart changes in a fetus of a diabetic mother. Trends Diabetes Metab. 2019;2:1–3.
Seok H, Oh JH. Hypertrophic cardiomyopathy in infants from the perspective of cardiomyocyte maturation. Korean Circ J. 2021;51:733–51.
Vimala J, Prabhu A, Pavithran S, et al. Hydrocortisone induced hypertrophic cardiomyopathy. Int J Cardiol. 2011;150:e94–5.
Kale Y, Aydemir O, Ceylan O, et al. Hypertrophic cardiomyopathy after a single dose of dexamethasone in a preterm infant. Pediatr Neonatol. 2015;56:268–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement.
Conflicts of interest
CD received honoraria from Chiesi Farmaceutici Spa and Vyaire Medical Inc. for scientific consultancy. Michele Luzzati, Iuri Corsini, Chiara Poggi, Venturella Vangi, Caterina Coviello, Simone Pratesi declare that they have no competing interests.
Ethics approval
Local Ethics Committees approved this study.
Consent to participate
Parental consent was not required since the data were anonymous.
Consent for publication
Parental consent was not required since the data were anonymous.
Availability of data and material
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
All authors made substantive intellectual contributions to the study design and manuscript, and revised the manuscript critically. CD and SP conceived the study; ML collected the data; IC, CP, VV, and SP performed the heart ultrasounds; and CD wrote the manuscript. All authors revised and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Dani, C., Luzzati, M., Corsini, I. et al. Cardiac Hypertrophy Associated with Insulin Therapy in Extremely Preterm Infants. Pediatr Drugs 25, 453–457 (2023). https://doi.org/10.1007/s40272-023-00571-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-023-00571-0