Abstract
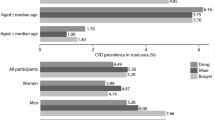
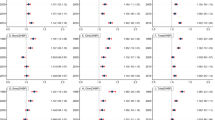
Higher rates of cardiovascular events have been observed among rural residents compared with urban. Hypertension and lack of blood pressure (BP) control are risk factors for cardiovascular events. We compared the prevalence of hypertension and controlled BP, and the distribution of systolic blood pressure (SBP), by urban-rural residence. Participants from the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study, a prospective cohort of Black and White adults aged ≥45 years, were categorized as either urban, large rural, or small-isolated rural, by using the Rural-Urban Commuting Area (RUCA) categorization B system. Oucomes were hypertension prevalence (BP ≥ 140/90 mmHg or antihypertensive use), BP control (BP < 140/90 among participants on antihypertensive medication), and the distribution of SBP. Counfounders were age, race, sex, antihypertensive medication use, and US Census Bureau division. The analysis included 26,133 participants (80.3% urban, 11.6% large-rural, 8.2% small-isolated rural). The unadjusted prevalence of hypertension was not different between groups. However, after adjustment, the odds of hypertension was higher among participants in the large rural group (odds ratio [OR] 1.17; 95% confidence interval [CI], 1.08–1.27) and small-isolated rural group (OR 1.19; 95% CI, 1.08–1.30), compared with the urban group. There was no evidence of an adjusted difference in BP control for those taking antihypertensive medications. Adjusted differences in SBP were greater for both rural groups, compared with urban, at the higher percentiles of SBP. Rural residence was associated with a higher adjusted odds of hypertension and higher SBP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
REGARDS facilitates data sharing through formal data use agreements. Any investigator is welcome to access the REGARDS data through this process. Requests for data access may be sent to regardsadmin@uab.edu.
References
Harrington RA, Califf RM, Balamurugan A, Brown N, Benjamin RM, Braund WE, et al. Call to action: rural health: a presidential advisory from the American Heart Association and American Stroke Association. Circulation. 2020;141:e615–e44.
Garcia MC, Faul M, Massetti G, Thomas CC, Hong Y, Bauer UE, et al. Reducing potentially excess deaths from the five leading causes of death in the rural United States. MMWR Surveill. Summaries. 2017;66:1.
Singh A, Jiang NM, Blaha M, Blankstein R, Nasir K. Urban-rural differences in coronary heart disease mortality in the United States in 2010-2015. Circ. Cardiovasc Qua Outcomes. 2019;12(Suppl_1):A135-A.
Kulshreshtha A, Goyal A, Dabhadkar K, Veledar E, Vaccarino V. Urban-rural differences in coronary heart disease mortality in the United States: 1999–2009. Public Health Rep. 2014;129:19–29.
Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–43.
Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1· 25 million people. Lancet. 2014;383:1899–911.
Collaboration PS. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Obisesan TO, Vargas CM, Gillum RF. Geographic variation in stroke risk in the United States: region, urbanization, and hypertension in the Third National Health and Nutrition Examination Survey. Stroke. 2000;31:19–25.
Levine DA, Lewis CE, Williams OD, Safford MM, Liu K, Calhoun DA, et al. Geographic and demographic variability in 20-year hypertension incidence: the CARDIA study. Hypertension. 2011;57:39–47.
Loop MS, Howard G, de Los Campos G, Al-Hamdan MZ, Safford MM, Levitan EB, et al. Heat maps of hypertension, diabetes mellitus, and smoking in the continental United States. Circ Cardiovasc Qual Outcomes. 2017;10:e003350.
Li C, Balluz LS, Okoro CA, Strine TW, Lin J-MS, Town M, et al. Surveillance of certain health behaviors and conditions among states and selected local areas—Behavioral Risk Factor Surveillance System, United States, 2009. Morbid Mortal Wkly Rep: Surveill Summ. 2011;60:1–249.
Washington W, Alaska, Montana, Idaho (WWAMI) Rural Health Research Center (RHRC). Rural Urban Commuting Area [depts.washington.edu/uwruca/ruca-uses.php].
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–71.
Bureau UC. 2010 Census Regions and Divisions of the United States 2010 [https://www.census.gov/geographies/reference-maps/2010/geo/2010-census-regions-and-divisions-of-the-united-states.html.
Howard G, Kleindorfer DO, Cushman M, Long DL, Jasne A, Judd SE, et al. Contributors to the excess stroke mortality in rural areas in the United States. Stroke. 2017;48:1773–8.
Cromartie J Rural America at a glance 2018 edition. 2018.
Gillum RF, Mussolino ME, Madans JH. Relation between region of residence in the United States and hypertension incidence-the NHANES I epidemiologic follow-up study. J Natl Med Assoc. 2004;96:625.
Mainous AG 3rd, King DE, Garr DR, Pearson WS. Race, rural residence, and control of diabetes and hypertension. Ann Fam Med. 2004;2:563–8.
Samanic CM, Barbour KE, Liu Y, Wang Y, Fang J, Lu H, et al. Prevalence of self-reported hypertension and antihypertensive medication use by county and rural-urban classification—United States, 2017. MMWR Morb Mortal Wkly Rep. 2020;69:533–9.
Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med. 2013;173:46–51.
Clark D, Colantonio LD, Min Y-I, Hall ME, Zhao H, Mentz RJ, et al. Population-attributable risk for cardiovascular disease associated with hypertension in black adults. JAMA Cardiol. 2019;4:1194–202.
Aggarwal R, Chiu N, Loccoh EC, Kazi DS, Yeh RW, Wadhera RK. Rural-urban disparities: diabetes, hypertension, heart disease, and stroke mortality among black and white adults, 1999-2018. J Am Coll Cardiol. 2021;77:1480–1.
Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015–2016. 2017.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115.
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596.
Ogunniyi MO, Commodore-Mensah Y, Ferdinand KC. Race, ethnicity, hypertension, and heart disease: JACC Focus Seminar 1/9. J Am Coll Cardiol. 2021;78:2460–70.
Howard G, Cushman M, Moy CS, Oparil S, Muntner P, Lackland DT, et al. Association of clinical and social factors with excess hypertension risk in black compared with white US adults. JAMA. 2018;320:1338–48.
Couch CA, Gray MS, Shikany JM, Howard VJ, Howard G, Long DL, et al. Correlates of a southern diet pattern in a national cohort study of blacks and whites: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Br J Nutr. 2021;126:1904–10.
Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129:611–20.
MacDowell M, Glasser M, Fitts M, Nielsen K, Hunsaker M. A national view of rural health workforce issues in the USA. Rural and Remote Health. 2010;10:1531.
Casey MM, Call KT, Klingner JM. Are rural residents less likely to obtain recommended preventive healthcare services? Am J Prev Med. 2001;21:182–8.
Probst JC, Laditka JN, Laditka SB. Association between community health center and rural health clinic presence and county-level hospitalization rates for ambulatory care sensitive conditions: an analysis across eight US states. BMC Health Serv Research. 2009;9:134.
Foutz J, Artiga S, Garfield R. The role of Medicaid in rural America. Washington, DC: Kaiser Family Foundation. 2017.
Ziller EC, Coburn AF, Yousefian AE. Out-of-pocket health spending and the rural underinsured. Health Affairs. 2006;25:1688–99.
Rural Health Research Center. Using RUCA data. http://depts.washington.edu/uwruca/ruca-uses.php.
Acknowledgements
The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at https://www.uab.edu/soph/regardsstudy/. This research project is supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health (NIH), Department of Health and Human Service (HHS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS, NIA, NIH, or HHS. Representatives of the NINDS were involved in the review of the manuscript but were not directly involved in the collection, management, analysis or interpretation of the data. Representatives of the NINDS were involved in the review of the manuscript but were not directly involved in the collection, management, analysis or interpretation of the data.
Author information
Authors and Affiliations
Contributions
BH helped concieve the project and drafted the manuscript; GH designed the analyses, performed the analyses, and helped draft and revise the manuscript; SC provided suggestsions and revisions for the manuscript; DK provided suggestsions and revisions for the manuscript; DL provided suggestions and revisions for the manuscript; PM helped design the analyses and helped draft the manuscript; EH helped design the analysis and drafted the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The REGARDS study was approved by the institutional review boards of the investigators, and all participants provided written informed consent. Ethical approval was not again needed for this secondary analysis of REGARDS data.
Competing interests
EAJ currently has funding from the NIH, Amgen, and the Agency for Healthcare Research and Quality, as well as consulting fees from the American College of Cardiology, Change Healthcare Technologies, and the American Heart Association. The other authors do not have relevant financial competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heindl, B., Howard, G., Clarkson, S. et al. Urban-rural differences in hypertension prevalence, blood pressure control, and systolic blood pressure levels. J Hum Hypertens 37, 1112–1118 (2023). https://doi.org/10.1038/s41371-023-00842-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-023-00842-w