Abstract
Proton pump inhibitors (PPI) and histamine-2 receptor antagonists (H2RA) are commonly used medications in neonates and infants for the treatment of gastroesophageal reflux disease (GERD), especially in neonatal intensive care units (NICUs). A literature review was conducted to evaluate the efficacy and safety of histamine-2 receptor antagonists (H2RAs) and proton pump inhibitors (PPIs) in preterm neonates, term neonates, and infants. A total of 27 studies were included in this review. Antacid medications in studies have consistently shown positive pharmacodynamic effects, including increasing gastric pH, reducing the reflux index, and reducing the number of acidic reflux events. The benefit found in placebo-controlled trials are limited exclusively to these surrogate outcomes. The actual clinically salient outcomes which H2RAs and PPIs are used for, such as reduction in GERD symptoms, especially irritability and improved feed tolerance and weight gain, have consistently shown no clinical benefit. H2RAs and PPIs appear to be extremely well tolerated by the neonatal and infant populations, which would mimic our experience with these medications in our unit. The available data from large, retrospective cohort and case-control studies paint a much more concerning picture regarding the potential for an increased risk in the development of allergies, anaphylactic reactions, necrotizing enterocolitis (NEC), other nosocomial infections, and lower respiratory tract infections. Given the risks associated with and lack of clinical effectiveness of both H2RAs and PPIs, use of these medications should be limited to specific clinical situations. Further studies are required to determine whether antacid pharmacologic therapy might benefit certain neonates and infants, such as those with complex medical issues.
Similar content being viewed by others
References
Baird DC, Harker DJ, Karmes AS. Diagnosis and treatment of gastroesophageal reflux in infants and children. Am Fam Physician. 2015;92:705–14.
Duncan DR, Rosen RL. Current insights into pharmacologic and nonpharmacologic management of gastroesophageal reflux in infants. NeoReviews. 2016;17:e203–12. https://doi.org/10.1542/neo.17-4-e203.
Eichenwald EC, AAP Committee on Fetus and Newborn. Diagnosis and management of gastroesophageal reflux in preterm infants. Pediatrics. 2018;142: e20181061. https://doi.org/10.1542/peds.2018-1061.
Rosen R, Vandenplas Y, Singendonk M, Cabana M, DiLorenzo C, Gottrand F, et al. Pediatric gastroesophageal reflux clinical practice guidelines: Joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2018;66:516–54. https://doi.org/10.1097/MPG.0000000000001889.
Davidson G, Wenzl TG, Thomson M, Omari T, Barker P, Lundborg P, et al. Efficacy and safety of once-daily esomeprazole for the treatment of gastroesophageal reflux disease in neonatal patients. J Pediatr. 2013;163:692–8. https://doi.org/10.1016/j.jpeds.2013.05.007.
Kierkus J, Furmaga-Jablonska W, Sullivan JE, David ES, Stewart DL, Rath N, et al. Pharmacodynamics and safety of pantoprazole in neonates, preterm infants and infants aged 1 through 11 months with a clinical diagnosis of gastroesophageal reflux disease. Dig Dis Sci. 2011;56:425–34. https://doi.org/10.1007/s10620-010-1321-3.
Kaguelidou F, Alberti C, Biran V, Bourdon O, Farnoux C, Zohar S, et al. Dose-finding study of omeprazole on gastric pH in neonates with gastro-esophageal acid reflux using a Bayesian sequential approach. PLoS ONE. 2016;11: e0166207. https://doi.org/10.1371/journal.pone.0166207.
Omari TI, Haslam RR, Lundborg P, Davidson GP. Effect of omeprazole on acid gastroesophageal reflux and gastric acidity in preterm infants with pathological acid reflux. J Pediatr Gastroenterol Nutr. 2007;44:41–4. https://doi.org/10.1097/01.mpg.0000252190.97545.07.
Omari T, Lundborg P, Sandstrom M, Bondarov P, Fjellman M, Haslam R, et al. Pharmacodynamics and systemic exposure of esomeprazole in preterm infants and term neonates with gastroesophageal reflux disease. J Pediatr. 2009;155:222–8. https://doi.org/10.1016/j.jpeds.2009.02.025.
Springer M, Atkinson S, North J, Raanan M. Safety and pharmacodynamics of lansoprazole in patients with gastroesophageal reflux disease aged < 1 year. Pediatr Drugs. 2008;10:255–63. https://doi.org/10.2165/00148581-200810040-00004.
Tham SY, Rogers IM, Samuel KF, Singh A, Ong KK. Dose oral lansoprazole really reduce gastric acidity in VLBW premature neonates? Med J Malaysia. 2012;67:284–8.
Ward RM, Tammara B, Sullivan SE, Stewart DL, Rath N, Meng X, et al. Single-dose, multiple-dose, and population pharmacokinetics of pantoprazole in neonates and preterm infants with a clinical diagnosis of gastroesophageal reflux disease (GERD). Eur J Clin Pharmacol. 2010;66:555–61. https://doi.org/10.1007/s00228-010-0811-8.
Wheatley E, Kennedy KA. Cross-over trial of treatment for bradycardia attributed to gastroesophageal reflux in preterm infants. J Pediatr. 2009;155:516–21. https://doi.org/10.1016/j.jpeds.2009.03.044.
Ranitidine. In: Micromedex [database on the Internet]. Greenwood Village (CO): IBM Corporation; 2023 [cited 2023 Jan 27]. Available from www.micromedexsolutions.com. Subscription required to view.
Moore DJ, Tao BSK, Lines DR, Hirte C, Heddle ML, Davidson GP. Double-blind placebo-controlled trial of omeprazole in irritable infants with gastroesophageal reflux. J Pediatr. 2003;143:219–23. https://doi.org/10.1067/S0022-3476(03)00207-5.
Omari T, Davidson G, Bondarov P, Nauclér E, Nilsson C, Lundborg P. Pharmacokinetics and acid-suppressive effects of esomeprazole in infants 1–24 months old with symptoms of gastroesophageal reflux disease. J Pediatr Gastroenterol Nutr. 2007;45:530–7. https://doi.org/10.1097/01.mpg.0000469415.50085.f7.
Bestebreurtje P, de Koning BAE, Roeleveld N, Knibbe CAJ, Tibboel D, van Groen B, et al. Rectal omeprazole in infants with gastroesophageal reflux disease: a randomized pilot trial. Eur J Drug Metab Pharmacokinet. 2020;45:635–43. https://doi.org/10.1007/s13318-020-00630-8.
Hussain S, Kierkus J, Hu P, Hoffman D, Lekich R, Sloan S, et al. Safety and efficacy of delayed release rabeprazole in 1- to 11-month-old infants with symptomatic GERD. J Pediatr Gastroenterol Nutr. 2014;58:226–36. https://doi.org/10.1097/MPG.0000000000000195.
Orenstein SR, Hassall E, Furmaga-Jablonska W, Atkinson S, Raanan M. Multicenter, double-blind, randomized, placebo-controlled trial assessing the efficacy and safety or proton pump inhibitor lansoprazole in infants with symptoms of gastroesophageal reflux disease. J Pediatr. 2009;154:514–20. https://doi.org/10.1016/j.jpeds.2008.09.054.
Orenstein SR, Shalaby TM, Devandry SN, Liacouras CA, Czinn SJ, Dice JE, et al. Famotidine for infant gastro-oesophageal reflux: a multi-centre, randomized, placebo-controlled, withdrawal trial. Aliment Pharmacol Ther. 2003;17:1097–107. https://doi.org/10.1046/j.1365-2036.2003.01559.x.
Winter H, Kum-Nji P, Mahomedy SH, Kierkus J, Hinz M, Li H, et al. Efficacy and safety of pantoprazole delayed-release granules for oral suspension in a placebo-controlled treatment-withdrawal study in infants 1–11 months old with symptomatic GERD. J Pediatr Gastroenterol Nutr. 2010;50:609–18. https://doi.org/10.1097/MPG.0b013e3181c2bf41.
Winter H, Gunasekaran T, Tolia V, Gottrand F, Barker PN, Illueca M. Esomeprazole for the treatment of GERD in infants ages 1–11 months. J Pediatr Gastroenterol Nutr. 2015. https://doi.org/10.1097/MPG.0B013E3182496B35.
Khoshoo V, Dhume P. Clinical response to 2 dosing regiments of lansoprazole in infants with gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 2008;46:352–4. https://doi.org/10.1097/MPG.0b013e31815667d7.
Mitre E, Susi A, Kropp LE, Schwartz DJ, Gorman GH, Nylund CM. Association between use of acid-suppressive medications and antibiotics during infancy and allergic diseases in early childhood. JAMA Pediatr. 2018;172: e180315. https://doi.org/10.1001/jamapediatrics.2018.0315.
Patil UP, Bailey SM, Wachtel EV, Orosz E, Zarchin R, Mally PV. Efficacy of and potential morbidities associate with the use of antacid medications in preterm neonates. J Perinat Med. 2017;45:947–52. https://doi.org/10.1515/jpm-2016-0285.
Singh N, Dhayade A, Mohamed AL, Chaudhari TV. Morbidiy and mortality in preterm infants following antacid use: a retrospective audit. Int J Pediatr. 2016. https://doi.org/10.1155/2016/9649162.
Guillet R, Stoll BJ, Cotton CM, Gantz M, McDonald S, Poole WK, Phelps DL. Association of H2-blocker therapy and higher incidence of necrotizing enterocolitis in very low birth weight infants. Pediatrics. 2006;117:e137–42. https://doi.org/10.1542/peds.2005-1543.
Terrin G, Passariello A, De Curtis M, Manguso F, Salvia G, Lega L, et al. Ranitidine is associated with infections, necrotizing enterocolitis, and fatal outcome in newborns. Pediatrics. 2012;129:e40–5. https://doi.org/10.1542/peds.2011-0796.
Bianconi S, Gudavalli M, Sutija VG, Lopez AL, Barillas-Arias L, Ron N. Ranitidine and late-onset sepsis in the neonatal intensive care unit. J Perinat Med. 2007;35:147–50. https://doi.org/10.1515/JPM.2007.017.
Bilali A, Galanis P, Bartsocas C, Sparos L, Velonakis E. H2-blocker therapy and incidence of necrotizing enterocolitis in preterm infants: a case-control study. Pediatr Neonatol. 2013;54:141–2. https://doi.org/10.1016/j.pedneo.2013.01.011.
Romaine A, Ye D, Ao Z, Fang F, Johnson O, Blake T, et al. Safety of histamine-2 receptor blockers in hospitalized VLBW infants. Early Hum Dev. 2016;99:27–30. https://doi.org/10.1016/j.earlhumdev.2016.05.010.
Santana RNS, Santos VS, Riberio-Júnior RF, Freire MS, Menezes MAS, Cipolotti R, et al. Use of ranitidine is associated with infections in newborns hospitalized in a neonatal intensive care unit: a cohort study. BMC Infect Dis. 2017;17:375. https://doi.org/10.1186/s12879-017-2482-x.
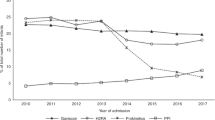
Slaughter JL, Stenger MR, Reagan PB, Jadcherla SR. Neonatal h2-receptor antagonist and proton pump inhibitor treatment at US children’s hospitals. J Pediatr. 2017;174:63-70.e3. https://doi.org/10.1016/j.jpeds.2016.03.059.
Cresi F, Martinelli D, Maggiora E, Locatelli E, Liguori SA, Baldassarre ME, et al. Cardiorespiratory events in infants with gastroesophageal reflux symptoms: is there any association? Neurogastroenterol Motil. 2018;30: e13278. https://doi.org/10.1111/nmo.13278.
Nobile S, Marchionni P, Noviello C, Carnielli VP. Correlation between cardiorespiratory events and gastro-esophageal reflux in preterm and term infants: analysis of predisposing factors. Early Hum Dev. 2019;134:14–8. https://doi.org/10.1016/j.earlhumdev.2019.05.003.
Di Fiore J, Arko M, Herynk B, Martin R, Hibbs AM. Charcterization of cardiorespiratory events following gastroesophageal reflux (GER) in preterm infants. J Perinatol. 2010;30:683–7. https://doi.org/10.1038/jp.2010.27.
Jadcherla SR, Hasenstab KA, Wei L, Osborn EK, Viswanathan S, Gulati IK, et al. Role of feeding strategy bundle with acid-suppressive therapy in infants with esophageal acid reflux exposure: a randomized controlled trial. Pediatr Res. 2021;89:645–52. https://doi.org/10.1038/s41390-020-0932-4.
Litalien C, Théorét Y, Faure C. Pharmacokinetics of proton pump inhibitors in children. Clin Pharmacokinet. 2005;44:441–66. https://doi.org/10.2165/00003088-200544050-00001.
Ward RM, Kearns GL. Proton pump inhibitors in pediatrics mechanism of action, pharmacokinetics, pharmacogenetics, and pharmacodynamics. Pediatr Drugs. 2013;15:119–31. https://doi.org/10.1007/s40272-013-0012-x.
Orenstein SR, Shalaby TM, Kelsey SF, Frankel E. Natural history of infant reflux esophagitis: symptoms and morphometric histology during one year without pharmacotherapy. Am J Gastroenterol. 2006;101:628–40. https://doi.org/10.1111/j.1572-0241.2006.00442.x.
Green DS, Abdel-Latif ME, Jones LJ, Lui K, Osborn DA. Pharmacological interventions for prevention and treatment of upper gastrointestinal bleeding in newborn infants. Cochrane Database Syst Rev. 2019;7:11785. https://doi.org/10.1002/14651858.CD011785.pub2.
Rommel N, van Wijk M, Boets B, Hebbard G, Haslam R, Davidson G, et al. Development of pharyngo-esophageal physiology during swallowing in the preterm infant. Neurogastroenterol Motil. 2011;23:e401–8. https://doi.org/10.1111/j.1365-2982.2011.01763.x.
Ayerbe JIG, Hauser B, Salvatore S, Vandenplas Y. Diagnosis and management of gastroesophageal reflux disease in infants and children: from guidelines to clinical practice. Pediatr Gastroenterol Hepatol Nutr. 2019;22:107–21. https://doi.org/10.5223/pghn.2019.22.2.107.
Cohen S, de Mesquita MB, Mimouni FB. Adverse effects reported in the use of gastroesophageal reflux disease treatments in children: a 10 years literature review. Br J Clin Pharmacol. 2015;80:200–8. https://doi.org/10.1111/bcp.12619.
Li Y, Xiong M, Yang M, Wang L, Nie S, Liu D, et al. Proton pump inhibitors and the risk of hospital-acquired acute kidney injury in children. Ann Transl Med. 2020;8:1438. https://doi.org/10.21037/atm-20-2284.
Anjewierden S, Han Z, Foster CB, Pant C, Deshpande A. Risk factors for Clostridium difficile infection in pediatric inpatients: a meta-analysis and systematic review. Infect Control Hosp Epidemiol. 2019;40:420–6. https://doi.org/10.1017/ice.2019.23.
Chang TH, Hsu WY, Yang TI, Lu CY, Hsueh PR, Chen JM, et al. Increased age and proton pump inhibitors are associated with severe Clostridium difficile infections in children. J Microbiol Immunol Infect. 2020;53:578–84. https://doi.org/10.1016/j.jmii.2018.09.002.
Bernal CJ, Aka I, Carroll RJ, Coco JR, Lima JJ, Acra SA, et al. CYP2C19 phenotype and risk of proton pump inhibitor-associated infections. Pediatrics. 2019;144: e20190857. https://doi.org/10.1542/peds.2019-0857.
William JH, Danziger J. Proton-pump inhibitor-induced hypomagnesemia: current research and proposed mechanisms. World J Nephrol. 2016;5:152–7. https://doi.org/10.5527/wjn.v5.i2.152.
Wang YH, Wintzell V, Ludvigsson JF, Svanström H, Pasternak B. Association between proton pump inhibitor use and risk of asthma in children. JAMA Pediatr. 2021;175:394–403. https://doi.org/10.1001/jamapediatrics.2020.5710.
Wang YH, Wintzwell V, Ludvigsson JF, Svanström H, Pasternak B. Association between proton pump inhibitor use and risk of fracture in children. JAMA Pediatr. 2020;174:1–10. https://doi.org/10.1001/jamapediatrics.2020.0007.
Malchodi L, Wagner K, Gorman G, Hisle-Gorman E. Early acid suppression therapy exposure and fracture in young children. Pediatrics. 2019;144: e20182625. https://doi.org/10.1542/peds.2018-2625.
Famouri F, Derakhshani F, Madihi Y, Shahsanai A. Electrolyte disturbances in children receiving omeprazole for gastroesophageal reflux disease. J Res Med Sci. 2020;25:106. https://doi.org/10.4103/jrms.JRMS_637_18.
Snoek KG, Reiss IKM, Greenough A, Capolupo I, Urlesberger B, Wessel L, et al. Standardized postnatal management of infants with congenital diaphragmatic hernia in Europe: The CDH EURO consortium consensus—2015 update. Neonatology. 2016;110:66–74. https://doi.org/10.1159/000444210.
Krishnan U, Mousa H, Dall’Oglio L, Homaira N, Rosen R, Faure C, et al. ESPGHAN-NASPGHAN guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with esophageal atresia-tracheoesophageal fistula. J Pediatr Gastroenterol Nutr. 2016;63:550–70. https://doi.org/10.1097/MPG.0000000000001401.
Sanchez JB, Jadcherla SR. Gastroesophageal reflux disease in neonates: facts and figures. NeoReviews. 2021;22:e104–17. https://doi.org/10.1542/neo.22-2-e104.
Chevalier I, Beck CE, Doré-Bergeron MJ, Orkin J. Medical management of gastro-esophageal reflux in healthy infants. Paediatr Child Health. 2022;27:503–11. https://doi.org/10.1093/pch/pxac068.
Acknowledgements
Not applicable
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
There are no conflicts of interest for Jason Tan, Sonia Jeffries, or Roxane Carr.
Ethics approval
Not applicable
Consent to participate
Not applicable
Consent for publication
Not applicable
Availability of data and material
This manuscript has no associated data.
Code availability
Not applicable
Author Contribution
All authors made substantial contributions to the conception and design of the work, and the acquisition, analysis, and interpretation of the data. All authors were involved in drafting the work and revising it critically for important intellectual content. All authors reviewed and provided approval for the final version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tan, J., Jeffries, S. & Carr, R. A Review of Histamine-2 Receptor Antagonist and Proton Pump Inhibitor Therapy for Gastroesophageal Reflux Disease in Neonates and Infants. Pediatr Drugs 25, 557–576 (2023). https://doi.org/10.1007/s40272-023-00580-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-023-00580-z