Abstract
Purpose of the Review
Current global information on incidence, prevalence, and mortality of type 1 diabetes (T1D) is limited, particularly in low- and middle-income countries. To address this gap in evidence, JDRF, Life for a Child, International Society for Pediatric and Adolescent Diabetes, and International Diabetes Federation have developed the T1D Index, which uses a Markov mathematical model, and machine learning and all available data to provide global estimates of the burden on T1D. This review assesses the methodology, limitations, current findings, and future directions of the Index.
Recent Findings
Global prevalence was estimated at 8.4 million in 2021, with 1.5 million <20 years (y). T1D prevalence varied from 1.5 to 534 per 100,000, with T1D accounting for <0.1–17.8% of all diabetes in different countries. A total of 35,000 young people <25 y are estimated to have died at clinical onset of T1D from non-diagnosis. An estimated 435,000 people <25 y were receiving “minimal care.” Health-adjusted life years (HALYs) lost for individuals diagnosed with T1D at age 10 y in 2021 ranged from 14 to 55 y.
Summary
These results show that interventions to reduce deaths from non-diagnosis, and improve access to at least an intermediate care level, are needed to reduce projected life years lost. The results have significant uncertainties due to incomplete data across the required inputs. Obtaining recent incidence, prevalence, and mortality data, as well as addressing data quality issues, misdiagnoses, and the lack of adult data, is essential for maintaining and improving accuracy. The index will be updated regularly as new data become available.
Similar content being viewed by others
Introduction
There is an urgent need for improved type 1 diabetes (T1D) epidemiology data across the world, in order to guide and inform resource allocation and health professional training and thereby improve outcomes. Data on T1D incidence, prevalence, or mortality is absent in many countries, and, even when there are data, they are often dated [1•, 2, 3]. Furthermore, although onset of clinical T1D can occur throughout the lifespan, epidemiological data is concentrated on T1D in children and youth and is scarce for adults [2, 4].
This problem of missing data is most pronounced in low- and middle-income countries where access to care is limited, and complications and mortality rates are thought to be high due to marked differences in diabetes diagnosis rates and treatment [2, 5,6,7].
The T1D Index project of the JDRF, Life for a Child, International Society for Pediatric and Adolescent Diabetes (ISPAD) and the International Diabetes Federation (IDF) was designed to produce just such an understanding by providing estimates of T1D prevalence and mortality in all countries, both now and into the future [8•, 9•]. It is an evolving, open-source project aimed at addressing data shortages through an innovative simulation-based approach, which will be updated regularly as new data become available. The initial findings have been published recently [8•] and were used in a 2022 update for the IDF Atlas [10]. These results emphasise the need for timely diagnosis of T1D and improved access to higher levels of care, which could together save millions of lives in coming decades.
Methodology
At the heart of the T1D Index is a Markov model that estimates the total number of people who have been diagnosed with or died from T1D in any given year based on incidence, mortality, and population size. In simple terms, historical data are used to follow a birth cohort of individuals throughout their simulated lives, with particular proportions of a given cohort developing symptomatic T1D, dying from T1D, or dying from other causes each year, based on the incidence and mortality data available for that year.
Whilst the concept of a Markov model is mathematically sound and frequently used in epidemiologic studies [8•, 11], the outputs of such a model (namely, estimates of prevalence and life-expectancy, and quantities derived from counter-factual scenarios such as “missing prevalence”) can only be as accurate as the model’s inputs allow. In particular, to provide a full set of prevalence estimates in a given year for individuals under the age of 80 years (y), the Markov model requires estimates of population, incidence, and mortality in each country, in each year, and at each age going back at least 80 y prior to the year in question. In addition, to project future prevalence estimates, the model requires projections of population, incidence, and mortality as inputs.
Determining estimates of incidence with this degree of granularity requires access to detailed data on incidence and population denominators in narrow age bands. Some data on diagnosed incidence (under age 20 y) for approximately half of the world’s countries are available from the literature. Data on adult incidence in 32 countries were obtained from Harding and colleagues [4]. However, although T1D incidence has been changing over time [3], data on long-term historical incidence are only available for relatively few countries. This first edition of the T1D Index used ratio-based imputation and stratified regression to extrapolate estimates based on these limited available data.
Producing mortality estimates poses similar challenges in terms of data limitations, requiring estimates of both background and diabetes-related mortality in each country, for each decrement of age and year. Whilst estimates of background population mortality are readily accessible from the UN World Population Prospects [12], it is much less clear how to model mortality arising from T1D, particularly historically. The approach taken in the T1D Index separates T1D-associated mortality into two categories: death soon after onset of symptomatic T1D from non-diagnosis and death in individuals living with a T1D diagnosis. Deaths from non-diagnosis were estimated based on a survey conducted by JDRF and ISPAD in 2020. These were modelled for those younger than 25 y in all countries except for high-income countries (where such deaths were assumed to be zero). Death in individuals living with T1D was estimated as a standardised mortality ratio (SMR) relative to the population mortality. These estimates were derived from a machine-learning method that, for countries and years without published data, predicted SMR based on region, country income class, infant mortality rate, doctors per capita, gross domestic product (GDP) per capita, mortality <5 years, and urbanisation percentage..
Not only is this approach novel but separating the two types of T1D-related deaths allows a quantification of the relative impacts of interventions targeting accurate diagnosis as compared to improving the quality of chronic care. Furthermore, modelling diabetes-related mortality in diagnosed patients based on an SMR allows the index to be integrated with previous work that has estimated SMRs for a given mean HbA1c [2]. The T1D Index can then be used to model the impact of certain T1D interventions such as the provision of insulin and blood glucose test strips on any of the model outputs (e.g., prevalence, life expectancy) by estimating the impact of these interventions on mean HbA1c and thereby on SMR.
Key Initial Findings
The model estimated that there were 8.4 million prevalent cases of T1D in 2021, with 1.5 million (18%) of these in people <20 y [8••]. The majority of all-age prevalent cases lived in just 10 countries (USA, India, Brazil, China, Germany, UK, Russia, Canada, Saudi Arabia, and Spain).
In 2021, there were an estimated 510,000 incident cases, with 194,000 <20 y [8••].
The results showed that exclusive focus on T1D in the paediatric and young adult population overlooks a significant portion of the T1D global burden. Adult-onset T1D is, in fact, more common than childhood-onset. The median age at diagnosis is 29 y, and the median age of a person living with T1D is 39 y. Although there is an early peak in the age of onset around age 10–14 y, incidence in adults remains substantial with even a potential trend towards an increasing incidence after age 50 y [8••].
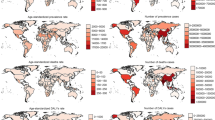
Prevalence per 100,000 population in 2021 <20 y varied significantly around the world, from 1.5 in Papua New Guinea to 534 in Finland. Table 1 gives 2021 prevalence estimates for all countries for <20 y and all ages, and Fig. 1 shows prevalence by world region and income group. Table 1 in the Supplementary Materials provides prevalence/100,000 for various age groups for all countries.
Diagnosed incidence <15 y ranged from 0.02/100,000 in parts of Melanesia to >50/100,000 in parts of Europe and the Middle East (see Table 1).
Table 1 in the Supplementary Materials provides prevalence and incidence per 100,000 <15 y, 15–19 y, <20 y, and all ages.
In 2021, there were an estimated 175,000 deaths due to T1D, 35,000 (20%) due to non-diagnosis, and 140,000 (80%) related to excess mortality in diagnosed individuals. However, the relative impact of these two types of mortality is reversed in the younger population. Of the 52,600 deaths occurring in individuals aged <25 y, the majority (67%) of deaths were attributed to non-diagnosis. Most of these occurred in Sub-Saharan Africa (14,500 deaths) and South Asia (8,700) [8••].
Estimated life expectancy of a 10-year old who develops new-onset symptomatic T1D varied from 7 years in a few African countries to up to 70 years in high-income countries [8••].
Using the T1D Index prevalence data and the IDF Atlas type 2 diabetes (T2D) prevalence data, T1D as a percentage of all diabetes in the population aged 0–79 years is 1.6% globally (this calculation excludes T2D <20 y as there are no current global estimates of this number). As the incidence of both T1D and T2D vary widely around the world, this percentage varies from 0.01% in Papua New Guinea to 17.8% in Norway. Figure 2 shows the range of T1D as a percentage of all cases of diabetes aged 0–79 y by world region and income group, and Table 1 provides this number for all countries.
Data Limitations
Incidence
Countries Without Data or With Fluctuating Data
There are few data available on the incidence of T1D; hence, the methods for the T1D Index rely on extrapolation [8••]. For example, only 97 of the 205 countries with more than 50,000 inhabitants have published data for any year at all, and very few countries have any data prior to 1975. Assumptions made about incidence prior to this time naturally affect any estimates made for the population over the age of 45 y. In some countries where data are available, observed incidence rates fluctuate from year to year. In order to use these data to estimate incidence over time in other countries in the same region, these estimates are smoothed. This may partially mask true incidence trends, although it reduces the risk of over-fitting.
Incidence Over Time
The work necessitated modelling of changes in incidence over time to populate most data points for most countries. This was done by fitting a line of best-fit to year-on-year annual percentage incidence change data for all years for which two or more countries had data (1985–2015). A global curve was developed, as well as curves for 10 geographic regions where there was sufficient data to model this, which were used in place of the global curves for years that had relevant data.
Table 1 shows the 2021 index incidence per 100,000 population <15 years for all countries, and compares these to the IDF Atlas 10th Edition figures [1•, 13], in which incidence for a particular country was kept stable at the level of the last published data. The median within-country difference between these estimates is an IDF Atlas estimate that was 27.5% lower than the T1D Index estimate. These differences will be greater in low- and middle-income countries if estimated non-diagnosis cases were included as the T1D Index incidence figure would be higher.
These index data show that, whilst estimated incidences have increased in nearly all countries (commensurate with global trends), they have increased three- to five-fold in some countries in Eastern Europe and the Middle East. This is due to the age of some of the studies which date from 1990 to 1999 (including the landmark DIAMOND studies [14]), or even earlier, as well as the rapid year-on-year increases seen in the published data from these regions. Whilst it is reasonable to assume that incidence has risen markedly in these countries with only dated studies countries since the mid-1990s, the 2021 index predictions for countries like Kuwait, Ukraine, and Poland are most likely over-estimated as the projected incidences are now approaching or exceeding incidence in Finland, which has the highest reported incidence. We believe that it is more likely that after incidence has increased steadily for a period, the increase in incidence will then plateau as has been seen in some high-risk European-origin populations [3, 9•]. Further variation would then occur between countries depending on where they are in the timescale depending on the varying temporal impacts of the incompletely understood environmental factors which are causing the increase in incidence. Nonetheless, there is marked inter-country variation in incidence over time even in European-origin populations [3, 9•].
Limited Data for Adults, and Misclassification of Diabetes Type
Adult T1D incidence data are only available from 32 countries. The peak age-of-onset appears to be later in sub-Saharan Africa (from a pool of four studies), and so a separate T1D onset pattern was modelled for this region. Moreover, the diagnosis of adult-onset T1D is complicated by the high incidence of T2D in this age group, with a disease progression that is slower and less likely to present with diabetic ketoacidosis, or for insulin treatment to be initiated at onset irrespective of probable type [15]. Misclassification rates of T1D versus T2D are therefore likely to be high [16, 17], and methods of diagnosis vary, depending on the use or availability of biomarkers such as C-peptide and autoantibodies [4].
The potential for misclassification can also occur in childhood and adolescent populations as well, due to the heterogeneity of T1D [18, 19], which appears to be more pronounced in sub-Saharan Africa and South Asia [5, 20].
Death from Non-diagnosis
It is not possible to obtain data on the death rate from non-diagnosis since unidentified cases by their very nature cannot be reliably enumerated. The rates of death from non-diagnosis used in the index were therefore derived from the JDRF/ISPAD 2020 survey of health professionals, who were asked to estimate, in the region in which they live, the percentage of all children and youth who develop symptomatic T1D who die soon after onset without ever being diagnosed [8••]. They were requested to estimate this rate in three time periods: before 2000, 2000–2010, and after 2010. For example, in Sub-Saharan Africa prior to 2010, the mean survey response was a non-diagnosis rate of 60%.
These numbers may well be underestimates of the number of cases missed. Data from case studies following the initiation of systematic care and increased diabetes awareness can help quantify this issue. For example, in Mali [6], the observed incidence of T1D in the <25-year age group in 2007 was 0.12/100,000, increasing to 0.74/100,000 in 2016, an observed incidence ratio of 6.2. The ratio of observed incidences is equal to the ratio of true incidences multiplied by the ratio of diagnosis rates. Therefore, an increase of this magnitude in the observed incidence can only be due to a substantial increase in true incidence or a substantial increase in diagnosis rate. To explain this increase by true incidence increase alone would require assuming an average annual year-to-year increase in incidence of 22.4% (1.2246 = 6.2), far higher than that observed in other countries. A more modest but still rapid increase in true incidence of 7% per year would only give a true incidence ratio of 1.8 (1.076). To explain the observed ratio of 6.2 would require a diagnosis rate in 2016 that was 3.4 times higher than the 2007 rate (6.2/1.8). Even if no cases were missed in 2016 (diagnosis rate of 100%), these figures would imply a diagnosis rate of just 30% (100%/3.4) in 2007. Similar rapid increases in incidence have been observed in Rwanda [21], Gabon [22], and Burkina Faso [23]. See also the Supplementary Material in [8••].
Recently, Ward et al. [24], using a different modelling approach, have also drawn attention to this large number of estimated deaths from non-diagnosis.
Mortality
Estimates of mortality in individuals living with T1D were based on an SMR relative to background mortality. The SMRs used in the index are based on the outputs of a machine learning model trained on a very sparse dataset consisting of 71 data points representing the SMR for a person with T1D in a particular year, country, and age group. This extrapolation relied on assumptions including that the overall pattern of SMR variation across an individual’s life-span was constant across all countries and years. In addition, one of the inputs on which the model was trained (aside from readily available population statistics such as infant mortality rate, doctors per capita or GDP) was an estimate of the proportion of individuals in a particular region and at a particular time who were receiving a “minimal” versus a more than minimal (“non-minimal”) level of care (minimal care is defined as a simple insulin regimen with minimal or no self-blood glucose monitoring, HbA1c testing, and diabetes education) [2, 7]). These estimates were made based on expert opinion alone (Table 2).
Projections
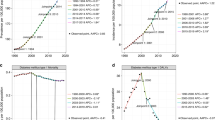
Projections of future prevalence and associated statistics rely on underlying assumptions about ongoing trends in incidence and mortality which cannot be known with certainty. To account for this, the index modelled two scenarios. In one case (conservative estimate), incidence, mortality, and diagnosis rates were held constant going forward. In the second case (momentum estimate), they continued to change at the average rate of change between 2012 and 2021. Projections suggest that there will be a substantial increase in T1D prevalence between 2020 and 2040, of between 66 and 116% depending on the scenario, due to projected reductions in mortality and, in some regions, increase in incidence. Although the figures are not precise, it is clear that the global burden of T1D will markedly increase in the medium-term future.
Further Modelling on Health Life Years and Numbers Receiving “Minimal Care”
This work aimed to quantify health-adjusted life years. HALYs, also known as disability-free life-expectancy, is the number of remaining years a person is expected to live without disability. HALYs were quantified by a two-stage procedure. In the first stage, a level of care is assigned to a particular region [2]. A given level of care is assumed to be associated with a particular level of glycaemic control, reflected in the mean achieved HbA1c, and in turn with a particular SMR for diabetes-associated mortality. An iteration of the T1D Index model is run to produce estimates of incidence, prevalence, and mortality for that region. In particular, such an iteration allows estimation of the number of individuals in a particular region who have been living with diabetes for any duration of time.
In the second stage, the proportions of individuals living with specific complications of diabetes are determined using methodology from the childhood-onset cohort of the University of Pittsburgh Epidemiology of Diabetes Complications (EDC) study [25•], followed out to 30 years after diagnosis. This methodology provides estimates of the prevalence of several complications at each duration of diabetes, as a function of mean HbA1c. The modelled complications are distal symmetric polyneuropathy, ulcer or amputation, hypertension or microalbuminuria, overt nephropathy, proliferative retinopathy, blindness, non-fatal myocardial infarction, and non-fatal cerebrovascular disease. Each complication type is modelled as a separate occurrence, conditionally independent of one another at a given level of glycaemic control (mean Hba1c). The exception to this principle is an adjustment made to disallow the de novo occurrence of proliferative retinopathy in an already blind individual, and likewise of hypertension/microalbuminuria in an individual with overt nephropathy (such situations were termed ‘impermissible journeys’). Figure 3 is an example of the Gregory et al. [25•] study results, showing the modelled frequency of selected complications at 30 years after diagnosis. Finally, these proportions are combined with population data and standard disability adjusted life years (DALY) costs for each complication to produce an overall estimate of DALYs, reframed as HALYs lost.
Modelled frequency of selected complications at 30 years after diagnosis of type 1 diabetes. Data from Gregory et al. (2020) [24]
The analysis showed marked disparities in predicted outcomes for people living with T1D depending on geography. The estimated HLY lost for an individual diagnosed with T1D at age 10 y in 2021 varied from 14 to 55 years (Fig. 4). Figure 5 shows, for 12 representative countries, that the HALY lost in high-income countries are mostly due to disability, whilst in lower-income countries, a shorter lifespan is the major contributor to total HLY lost.
This analysis has a number of limitations. In addition to those noted above regarding the modelling of diabetes-related mortality with SMRs, key assumptions of this modelling are (a) that a particular level of care is able to achieve a given mean HbA1c and (b) that mortality and complication rates can be reliably estimated based on this metric. In practice, the HbA1c achieved by a particular level of care will vary both across individuals receiving that care level, and within patients throughout the duration of their diabetes. For example, the level of glycaemic control tends to vary with age and likely varies across time.
In addition, the EDC study only estimated complication rates up to a diabetes duration of 30 years, and it is not clear what the best assumptions should be for extrapolating ongoing rates of complications beyond 30-year duration. It was also a study of complication rates in a higher-income setting, which may underestimate the complication rates truly experienced by people with diabetes with higher mean HbA1c’s in lower income settings.
Future Development and Actions
The T1D Index model’s limitations are not static, but rather serve as catalysts for continuous refinement. This improvement is a dual-pronged process involving the integration of new data and the enhancement of the model’s components.
New T1D-specific data will be assimilated into the model at each revision. This includes not just incidence, prevalence, and mortality data but also information on the proportions in each country receiving specific levels of care, and attendant outcomes. These epidemiological and clinical data are becoming more abundant due to the establishment of regional and national registries, the continuous expansion of trans-national initiatives such as the SWEET Database [26], the fostering of epidemiological studies in countries where there are no data or it is quite dated [1•, 27], and data resulting from the operations and attendant research, in partnership with local stakeholders, of programs such as Life for a Child [28], Changing Diabetes in Children [29], and Action4Diabetes [30]. Data collection is becoming easier through digital tools that streamline data collection with in-clinic workflows, using mobile phones and the web. However, there is a recognition [27] that guidelines and tools are needed, such as for standardising the definition of T1D, with resources such as the IDF Guide for Diabetes Epidemiology Studies being potentially helpful in this regard [31].
We will also incorporate changes in underlying country characteristics such as infant mortality, doctor-population ratio, urbanisation rates, and economic changes.
This generation of new data should progressively enhance the accuracy of the index’s predictions. Ideally, as data quality improves and ascertainment becomes complete, reliance on predictions will diminish.
In the interim and beyond integrating new data, we are also committed to refining the model's components. Our strategy involves implementing our own improvements and modifications, which will be open for public comment before integration.
Key areas of methodological improvement we are exploring for future versions of the T1D Index include the following:
Prevalence: Integrating actual prevalence data (e.g., from registries) into the model. Discrepancies between observed prevalence and the model’s predictions will inform adjustments to our overall estimates as well as the inputs and algorithms which shaped them. A “tuning” algorithm of this kind will also mean that including prevalence data from one country will help to refine estimates for similar countries.
Incidence: Through increased access to registry data, as well as new studies and refinements in modelling, we aim to improve our capacity for more accurately projecting out-of-sample data, particularly in settings where a lower incidence (from an older study) could still imply a significantly higher future incidence. We also aim to examine regional differences within large countries such as India.
Diagnosis Rates: Our estimates of non-diagnosis mortality rates described above suggest that the model may currently be under-estimating these rates. We are interested in exploring other estimation methods as well as encouraging and supporting new interventions aimed at improving diagnosis, such as those described in Mali [6].
Mortality and Complication Rates: Recent models predict these rates using published mortality rates and either HbA1C [25•] and/or country characteristics [8••]. Future model revisions will integrate these approaches and include data from registries and administrative data under various monitoring and treatment regimens. This will allow us to improve our estimates of mortality and complication rates, and also improve projections, by leveraging data on the adoption rates of different types and models of care in each country.
We welcome feedback and suggestions for improvement, which can be submitted directly to the authors or to the Index staff at hello@t1dindex.org.
Conclusions
The first version of the T1D Index has produced robust estimates of T1D incidence, prevalence, and mortality for all countries. The various limitations of the model will be reduced with progressive new versions as more data become available and the modelling is refined.
The results demonstrate great disparity in outcomes around the world. Initiatives are needed to reduce death from non-diagnosis, and improve the level of care, especially in low- and middle-income countries.
Change history
14 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11892-023-01524-0
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
. Ogle GD, James S, Dabelea D, Pihoker C, Svennson J, Maniam J, et al. Global estimates of incidence of type 1 diabetes in children and adolescents: results from the International Diabetes Federation Atlas, 10th edition. Diabetes Res Clin Pract. 2022;183:109083. 2021 International Diabetes Federation Atlas data.
Chan JCN, Lim L-L, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2021;396:2019–82.
Tuomilehto J, Ogle GD, Lund-Blix NA, Stene LC. Update on worldwide trends in occurrence of childhood type 1 diabetes in 2020. Pediatr Endocrinol Rev. 2020;17:198–209.
Harding JL, Wander PL, Zhang X, Li X, Karuranga S, Chen H, et al. The incidence of adult-onset type 1 diabetes: a systematic review from 32 countries and regions. Diabetes Care. 2022;45:994–1006.
Atun R, Davies JI, Gale EAM, Bärnighausen T, Beran D, Kengne AP, et al. Diabetes in sub-Saharan Africa: from clinical care to health policy. Lancet Diabetes Endocrinol. 2017;5:622–67.
Sandy JL, Besançon S, Sidibé AT, Minkailou M, Togo A, Ogle GD. Rapid increases in observed incidence and prevalence of type 1 diabetes in children and youth in Mali, 2007-2016. Pediatr Diabetes. 2021;22:545–51.
Ogle GD, von Oettingen JE, Middlehurst AC, Hanas R, Orchard TJ. Levels of type 1 diabetes care in children and adolescents for countries at varying resource levels. Pediatr Diabetes. 2019;20:93–8.
. Gregory GA, Robinson TIG, Linklater SE, Wang F, Colagiuri S, de Beaufort C, et al. Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: a modelling study. Lancet Diabetes Endocrinol. 2022;10:741–60. The first publication of T1D Index methodology and data.
.•Type 1 Diabetes Index [Internet]. Type 1 diabetes index. 2022 [cited 2023 May 21]. Available from: https://www.t1dindex.org/. Detailed T1D data by country.
Type 1 diabetes estimates in children and adults [Internet]. [cited 2023 May 21]. Available from: https://diabetesatlas.org/atlas/t1d-index-2022.
Sonnenberg FA, Beck JR. Markov models in medical decision making: a practical guide. Med Decis Making. 1993;13:322–38.
World Population Prospects - Population Division - United Nations [Internet]. [cited 2023 May 22]. Available from: https://population.un.org/wpp/.
IDF Diabetes Atlas 2021 [Internet]. [cited 2023 May 21]. Available from: https://diabetesatlas.org/atlas/tenth-edition/.
DIAMOND Project Group. Incidence and trends of childhood Type 1 diabetes worldwide 1990-1999. Diabet Med. 2006;23:857–66.
Leslie RD, Evans-Molina C, Freund-Brown J, Buzzetti R, Dabelea D, Gillespie KM, et al. Adult-onset type 1 diabetes: current understanding and challenges. Diabetes Care. 2021;44:2449–2456.
Thomas NJ, Lynam AL, Hill AV, Weedon MN, Shields BM, Oram RA, et al. Type 1 diabetes defined by severe insulin deficiency occurs after 30 years of age and is commonly treated as type 2 diabetes. Diabetologia. 2019;62:1167–72.
Muñoz C, Floreen A, Garey C, Karlya T, Jelley D, Alonso GT, et al. Misdiagnosis and diabetic ketoacidosis at diagnosis of type 1 diabetes: patient and caregiver perspectives. Clin Diabetes. Am Diabetes Assoc. 2019;37:276–81.
Leete P, Oram RA, McDonald TJ, Shields BM, Ziller C, TIGI study team, et al. Studies of insulin and proinsulin in pancreas and serum support the existence of aetiopathological endotypes of type 1 diabetes associated with age at diagnosis. Diabetologia. 2020;63:1258–67.
Battaglia M, Ahmed S, Anderson MS, Atkinson MA, Becker D, Bingley PJ, et al. Introducing the endotype concept to address the challenge of disease heterogeneity in type 1 diabetes. Diabetes Care. 2020;43:5–12.
Zabeen B, Maniam J, Balsa AMM, Tayyeb S, Huda K, Azad K, et al. Incidence of diabetes in children and adolescents in Dhaka Bangladesh. J Pediatr Endocrinol Metab. 2021;34:509–15.
Marshall SL, Edidin D, Arena VC, Becker DJ, Bunker CH, Gishoma C, et al. Prevalence and incidence of clinically recognized cases of type 1 diabetes in children and adolescents in Rwanda. Africa. Diabet Med. 2015;32:1186–92.
Pambou Damiens A, Ganga-Zandzou PS, Tsoucka Ibounde E, Kayemba-Kay’s S, Baye E, Biloghe P, et al. Type 1 diabetes mellitus in Gabon: a study of epidemiological aspects. Int J Pediatr Adolesc Med. 2019;6:87–91.
Sagna Y, Bagbila WPAH, Zoungrana L, Saloukou ME, Traore S, Sawadogo CG, et al. Incidence and prevalence of type 1 diabetes in children and young adults in Burkina Faso. Pediatr Diabetes. 2022;10(23):44–178.
Ward ZJ, Yeh JM, Reddy CL, Gomber A, Ross C, Rittiphairoj T, et al. Estimating the total incidence of type 1 diabetes in children and adolescents aged 0-19 years from 1990 to 2050: a global simulation-based analysis. Lancet Diabetes Endocrinol. 2022;10:848–58.
. Gregory GA, Guo J, Klatman EL, Ahmadov GA, Besançon S, Gomez ED, et al. Costs and outcomes of “intermediate” vs “minimal” care for youth-onset type 1 diabetes in six countries. Pediatr Diabetes. 2020;21:628–36. Background methodology of complications and HALYs.
SWEET Database [Internet]. [cited 2023 May 21]. Available from: https://www.sweet-project.org/sweet-database.php.
Beran D, Højlund K, Besançon S, Mundt ML, Ogle GD, Ramaiya K, et al. A plan to improve global type 1 diabetes epidemiology data. Lancet Diabetes Endocrinol. 2023;11:154–5.
Home - Life for a Child [Internet]. Life for a Child - No child should die of diabetes. 2022 [cited 2023 May 21]. Available from: https://lifeforachild.org/.
Changing Diabetes in Children programme for children with type 1 diabetes [Internet]. Novo Nordisk. [cited 2023 May 21]. Available from: https://www.novonordisk.com/content/nncorp/global/en/sustainable-business/access-and-affordability/changing-diabetes-in-children.html.
Action4Diabetes (A4D) [Internet]. Action4Diabetes (A4D) - Giving Health & Hope to people with Type 1 Diabetes. 2021 [cited 2023 May 21]. Available from: https://action4diabetes.org/.
Guide for Diabetes Epidemiology Studies [Internet]. [cited 2023 May 21]. Available from: https://www.idf.org/our-activities/epidemiology-research/idf-guide-for-diabetes-epidemiology-studies.html
Acknowledgements
We acknowledge the support of JDRF Global and the Leona M and Harry B Helmsley Charitable Trust, the other co-authors of the first T1D Index paper (Ms Priyanka Rai, Professor Kim Donaghue, Professor Stephen Colagiuri, Dr Sarah Linklater, Professor Carine de Beaufort, and International Diabetes Federation Diabetes Atlas Type 1 Diabetes in Adults Special Interest Group).
Data Sharing
The data will be made available to any researcher who requests them from the corresponding author. Data is also publicly accessible at "http://t1dindex.org".
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions This study was funded by The Leona M. and Harry B. Helmsley Charitable Trust (grant 2019PG-T1D023 part-supporting salaries of GDO, JM, and GAG), JDRF International (salary support of TIGR, FW), and the University of Sydney Medical School (Faculty of Medicine and Health Summer Research Scholarship to GAG). DJM is supported by a NHMRC Investigator Grant, level 2.
Author information
Authors and Affiliations
Contributions
Graham Ogle contributed to study conception and design. Data were produced by Fei Wang, Gabriel Gregory, and Thomas Robinson. Fei Wang and Jayanthi Maniam analysed the data. The first draft of the manuscript was written by Graham Ogle, Gabriel Gregory, and Thomas Robinson. All other co-authors contributed to the manuscript drafts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Graham D. Ogle and Gabriel A. Gregory are co-first authors.
Topical Collection on Diabetes Epidemiology
The original online version of this article was revised: The original version of this article contained a mistake in the name of the 6th author. It should be Dianna J Magliano rather than Diana J Magliano.
Supplementary Information
ESM 1
(DOCX 52 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ogle, G.D., Gregory, G.A., Wang, F. et al. The T1D Index: Implications of Initial Results, Data Limitations, and Future Development. Curr Diab Rep 23, 277–291 (2023). https://doi.org/10.1007/s11892-023-01520-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-023-01520-4