Abstract
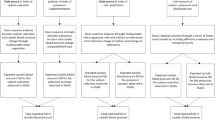
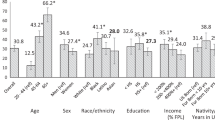
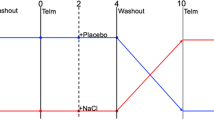
Dietary sodium and potassium have been shown to affect blood pressure (BP) but their influence on BP variability (BPV) is less studied as is the influence of sex. The aim of this study was to compare 24 h BP and short-term BPV in response to varying dietary levels of sodium and potassium in healthy non-obese normotensive salt-resistant adults. We hypothesized that high sodium would increase short-term BP and BPV while the addition of high potassium would counteract this increase. Furthermore, we hypothesized that women would experience greater increases in BPV under high sodium conditions compared to men while potassium would attenuate this response. Thirty-seven participants (17 M/20 W; 27 ± 5 years old; BMI 24.3 ± 3 kg/m2) completed seven days each of the following randomized diets: moderate potassium/low sodium (MK/LS), moderate potassium/high sodium (MK/HS) and high potassium/high sodium (HK/HS). BP and short-term BPV were assessed using 24 h ambulatory BP monitoring starting on day 6. BPV was calculated using the average real variability (ARV) index. Twenty-four hour, daytime, and nighttime systolic BP (SBP) were lower in women compared to men regardless of diet. However, 24 h and daytime SBP were lowered in women on the HK/HS diet compared to the MK/HS diet. There were no significant effects of diet or sex for 24 h, daytime or nighttime SBP ARV. However, men exhibited a higher 24 hDBP ARV than women regardless of diet. In conclusion, a high potassium diet lowered BP under high sodium conditions in women alone while men exhibited higher short-term BPV that was not influenced by diet.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data are available upon request from the corresponding author.
References
Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ 2013;346:f1378.
Stallings VA, Harrison, M, Oria M. Dietary References Intakes for Sodium and Potassium. Washington, D.C.: National Academies Press; 2019.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10.
Bray GA, Vollmer WM, Sacks FM, Obarzanek E, Svetkey LP, Appel LJ, et al. A further subgroup analysis of the effects of the DASH diet and three dietary sodium levels on blood pressure: results of the DASH-Sodium Trial. Am J Cardiol. 2004;94:222–7.
Elliott P, Marmot M, Dyer A, Joossens J, Kesteloot H, Stamler R, et al. The INTERSALT study: main results, conclusions and some implications. Clin Exp Hypertens A 1989;11:1025–34.
DuPont JJ, Greaney JL, Wenner MM, Lennon-Edwards SL, Sanders PW, Farquhar WB, et al. High dietary sodium intake impairs endothelium-dependent dilation in healthy salt-resistant humans. J Hypertens. 2013;31:530–6.
Smiljanec K, Mbakwe A, Ramos Gonzalez M, Farquhar WB, Lennon SL. Dietary Potassium Attenuates the Effects of Dietary Sodium on Vascular Function in Salt-Resistant Adults. Nutrients 2020;12:1206.
Mena LJ, Felix VG, Melgarejo JD, Maestre GE. 24-Hour Blood Pressure Variability Assessed by Average Real Variability: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2017;6:e006895.
Dai L, Song L, Li X, Yang Y, Zheng X, Wu Y, et al. Association of visit-to-visit blood pressure variability with the risk of all-cause mortality and cardiovascular events in general population. J Clin Hypertens (Greenwich). 2018;20:280–8.
Frattola A, Parati G, Cuspidi C, Albini F, Mancia G. Prognostic value of 24-hour blood pressure variability. J Hypertens. 1993;11:1133–7.
Simmonds SS, Lay J, Stocker SD. Dietary salt intake exaggerates sympathetic reflexes and increases blood pressure variability in normotensive rats. Hypertension 2014;64:583–9.
Ozkayar N, Dede F, Ates I, Akyel F, Yildirim T, Altun B. The relationship between dietary salt intake and ambulatory blood pressure variability in non-diabetic hypertensive patients. Nefrologia 2016;36:694–700.
Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension 2001;37:1199–208.
He J, Gu D, Chen J, Jaquish CE, Rao DC, Hixson JE, et al. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J Hypertens. 2009;27:48–54.
Wenger NK, Arnold A, Bairey Merz CN, Cooper-DeHoff RM, Ferdinand KC, Fleg JL, et al. Hypertension Across a Woman’s Life Cycle. J Am Coll Cardiol. 2018;71:1797–813.
Greaney JL, DuPont JJ, Lennon-Edwards SL, Sanders PW, Edwards DG, Farquhar WB. Dietary sodium loading impairs microvascular function independent of blood pressure in humans: role of oxidative stress. J Physiol. 2012;590:5519–28.
Kurtz TW, DiCarlo SE, Pravenec M, Morris RC Jr. An Appraisal of Methods Recently Recommended for Testing Salt Sensitivity of Blood Pressure. J Am Heart Assoc. 2017;6:e005653.
O’Brien E, Coats A, Owens P, Petrie J, Padfield PL, Littler WA, et al. Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British hypertension society. BMJ 2000;320:1128–34.
Mena L, Pintos S, Queipo NV, Aizpurua JA, Maestre G, Sulbaran T. A reliable index for the prognostic significance of blood pressure variability. J Hypertens. 2005;23:505–11.
Tai C, Sun Y, Dai N, Xu D, Chen W, Wang J, et al. Prognostic significance of visit-to-visit systolic blood pressure variability: a meta-analysis of 77,299 patients. J Clin Hypertens (Greenwich). 2015;17:107–15.
Murtaugh MA, Beasley JM, Appel LJ, Guenther PM, McFadden M, Greene T, et al. Relationship of Sodium Intake and Blood Pressure Varies With Energy Intake: Secondary Analysis of the DASH (Dietary Approaches to Stop Hypertension)-Sodium Trial. Hypertension 2018;71:858–65.
Thayer JF, Sollers JJ 3rd, Friedman BH, Koenig J. Gender differences in the relationship between resting heart rate variability and 24-hour blood pressure variability. Blood Press. 2016;25:58–62.
Felder RA, Gildea JJ, Xu P, Yue W, Armando I, Carey RM, et al. Inverse Salt Sensitivity of Blood Pressure: Mechanisms and Potential Relevance for Prevention of Cardiovascular Disease. Curr Hypertens Rep. 2022;24:361–74.
Overlack A, Ruppert M, Kolloch R, Kraft K, Stumpe KO. Age is a major determinant of the divergent blood pressure responses to varying salt intake in essential hypertension. Am J Hypertens. 1995;8:829–36.
Jaquet F, Goldstein IB, Shapiro D. Effects of age and gender on ambulatory blood pressure and heart rate. J Hum Hypertens. 1998;12:253–7.
Maseli A, Aeschbacher S, Schoen T, Fischer A, Jung M, Risch M, et al. Healthy Lifestyle and Blood Pressure Variability in Young Adults. Am J Hypertens. 2017;30:690–9.
Imai Y, Aihara A, Ohkubo T, Nagai K, Tsuji I, Minami N, et al. Factors that affect blood pressure variability. A community-based study in Ohasama, Japan. Am J Hypertens. 1997;10:1281–9.
Migdal KU, Babcock MC, Robinson AT, Watso JC, Wenner MM, Stocker SD, et al. The Impact of High Dietary Sodium Consumption on Blood Pressure Variability in Healthy, Young Adults. Am J Hypertens. 2020;33:422–9.
Xue B, Badaue-Passos D Jr, Guo F, Gomez-Sanchez CE, Hay M, Johnson AK. Sex differences and central protective effect of 17beta-estradiol in the development of aldosterone/NaCl-induced hypertension. Am J Physiol Heart Circ Physiol. 2009;296:H1577–85.
Barnett SR, Morin RJ, Kiely DK, Gagnon M, Azhar G, Knight EL, et al. Effects of age and gender on autonomic control of blood pressure dynamics. Hypertension 1999;33:1195–200.
Hart EC, Charkoudian N, Wallin BG, Curry TB, Eisenach J, Joyner MJ. Sex and ageing differences in resting arterial pressure regulation: the role of the beta-adrenergic receptors. J Physiol. 2011;589:5285–97.
Lekontseva O, Chakrabarti S, Davidge ST. Endothelin in the female vasculature: a role in aging? Am J Physiol Regul Integr Comp Physiol. 2010;298:R509–16.
Komukai K, Mochizuki S, Yoshimura M. Gender and the renin-angiotensin-aldosterone system. Fundam Clin Pharm. 2010;24:687–98.
Pechere-Bertschi A, Maillard M, Stalder H, Brunner HR, Burnier M. Blood pressure and renal haemodynamic response to salt during the normal menstrual cycle. Clin Sci (Lond). 2000;98:697–702.
Staessen J, Bulpitt CJ, Fagard R, Lijnen P, Amery A. The influence of menopause on blood pressure. J Hum Hypertens. 1989;3:427–33.
Acknowledgements
We would like to thank our study coordinator Liza Walker, our research nurse, Wendy Nichols and the study dietitians, Sofia Sanchez and Kristina Krieger for their time and effort on this project.
Funding
This work was funded by the National Institutes of Health (P20GM113125 and 1R01HL145055).
Author information
Authors and Affiliations
Contributions
WBF and SLL conceived and designed research; MRG, KS, and AUM performed experiments; MRG, AJL, and RTP analyzed data; MRG, AJL, RTP, and SLL interpreted results of experiments; MRG and AJL prepared figures; MRG and AJL drafted manuscript; MRG, KS, AUM, AJL, RTP, WBF and SLL edited and revised manuscript; MRG, KS, AUM, AJL, RTP, WBF and SLL approved final version of manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramos-Gonzalez, M., Smiljanec, K., Mbakwe, A.U. et al. Sex influences blood pressure but not blood pressure variability in response to dietary sodium and potassium in salt-resistant adults. J Hum Hypertens 38, 62–69 (2024). https://doi.org/10.1038/s41371-023-00855-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-023-00855-5