Abstract
The number of childhood cancer survivors is increasing rapidly. According to American Association for Cancer Research, there are more than 750,000 childhood cancer survivors in the United States and Europe. As the number of childhood cancer survivors increases, so does cancer treatment-related cardiac dysfunction (CTRCD), leading to heart failure (HF). It has been reported that childhood cancer survivors who received anthracyclines are 15 times more likely to have late cancer treatment-related HF and have a 5-fold higher risk of death from cardiovascular (CV) disease than the general population. CV disease is the leading cause of death in childhood cancer survivors. The increasing need to manage cancer survivor patients has led to the rapid creation and adaptation of cardio-oncology. Cardio-oncology is a multidisciplinary science that monitors, treats, and prevents CTRCD. Many guidelines and position statements have been published to help diagnose and manage CTRCD, including those from the American Society of Clinical Oncology, the European Society of Cardiology, the Canadian Cardiovascular Society, the European Society of Medical Oncology, the International Late Effects of Childhood Cancer Guideline Harmonization Group, and many others. However, there remains a gap in identifying high-risk patients likely to develop cardiomyopathy and HF in later life, thus reducing primary and secondary measures being instituted, and when to start treatment when there is echocardiographic evidence of left ventricular (LV) dysfunctions without symptoms of HF. There are no randomized controlled clinical trials for treatment for CTRCD leading to HF in childhood cancer survivors. The treatment of HF due to cancer treatment is similar to the guidelines for general HF. This review describes the latest pharmacologic therapy for preventing and treating LV dysfunction and HF in childhood cancer survivors based on expert consensus guidelines and extrapolating data from adult HF trials.




Similar content being viewed by others
References
Wallace KB, Sardao VA, Oliveira PJ. Mitochondrial determinants of doxorubicin-induced cardiomyopathy. Circ Res. 2020;126(7):926–41.
Kitakata H, Endo J, Ikura H, et al. Therapeutic targets for DOX-induced cardiomyopathy: role of apoptosis vs. ferroptosis. Int J Mol Sci. 2022;23(3):1414. https://doi.org/10.3390/ijms23031414.
Kamphius JAM, Linschoten M, Cramer M, et al. Cancer therapy-related cardiac dysfunction of nonanthracycline chemotherapeutics: what is the evidence? JACC CardioOncol. 2019;1(2):280–90.
Zhang X, Zhu Y, Dong S, et al. Role of oxidative stress in cardiotoxicity of antineoplastic drugs. Life Sci. 2019;232: 116526. https://doi.org/10.1016/j.lfs.2019.06.001.
Rhea IB, Oliveira GH. Cardiotoxicity of novel targeted chemotherapeutic agents. Curr Treat Options Cardiovasc Med. 2018;20(7):53.
Mitchell JD, Cehic DA, Morgia M, et al. Cardiovascular manifestations from therapeutic radiation: a multidisciplinary expert consensus statement from the international cardio-oncology society. JACC Cardio Oncol. 2021;3:360–80.
Bansal N, Blanco JG, Sharma U, Pokharel S, Shisler S, Lipshultz SE. Cardiovascular diseases in survivors of childhood cancer. Cancer Metastases Rev. 2020;39(1):55–68.
de Baat EC, van Dalen EC, Mulder RL, et al. Primary cardioprotection with Dexrazoxane in patients with childhood cancer who are expected to receive anthracyclines: recommendations from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Child Adolesc Health. 2022;6(12):885–94.
Feijen EAM, Font-Gonzalez A, Van der Pal HJH, et al. Risk and temporal changes of heart failure among 5-year childhood cancer survivors: a DCOG-LATER study. JAHA. 2019;8:e009122.
de Baat EC, Feijen EAM, Reulen RC, et al. risk factors for heart failure among Pan-European childhood cancer survivors: a PanCareSurFup and ProCardio cohort and nested case–control study. J Clin Oncol. 2023;41(1):96–106.
Harake D, Franco VI, Henkel JM, Miller TL, Lipshultz SE. Cardiotoxicity in childhood cancer survivors: strategies for prevention and management. Future Cardiol. 2012;8(4):647–70.
Armstrong GT, Oeffinger KC, Chen Y, et al. Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J Clin Oncol. 2013;31:3673–80.
Lyon AR, Dent S, Stanway S, et al. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: a position statement and new risk assessment tools from the Cardio-Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio-Oncology Society. Eur J Heart Fail. 2020;22(11):1945–60.
Srivastava R, Batra A, Dhawan D, Bakhshi S. Association of energy intake and expenditure with obesity: a cross-sectional study of 150 pediatric patients following treatment for leukemia. Pediatr Hematol Oncol. 2017;34:29–35.
Iughetti L, Bruzzi P, Predieri B, Paolucci P. Obesity in patients with acute lymphoblastic leukemia in childhood. Ital J Pediatr. 2012;38:4.
Acar Z, Kale A, Turgut M, et al. Efficiency of atorvastatin in the protection of anthracycline-induced cardiomyopathy. J Am Coll of Cardiol. 2011;58(9):988–9.
Chotenimitkhun R, D’Agostino R Jr, Lawrence JA, et al. Chronic statin administration may attenuate early anthracycline-associated declines in left ventricular ejection function. Can J Cardiol. 2015;31(3):302–7.
Hundley WG, D’Agostino R, Crots T. Statins and left ventricular ejection fraction following doxorubicin treatment. NEJM Evid. 2022;1(9):EVIDoa2200097.
Nelian TG et al. STOP-CA clinical trial finds statins lower rate of heart decline in lymphoma patients, Late Breaking ACC23 Clinical Trial Reports. ACC.23/WCC Meeting Newspaper. Published on March 4, 2023, in JACC.
Marques-Aleixo I, Santos-Alves E, Oliveira PJ, Moreira PI, Magalhães J, Ascensão A. The beneficial role of exercise in mitigating doxorubicin-induced Mitochondrionopathy. Biochim Biophys Acta Rev Cancer. 2018;1869(2):189–99.
Smarz K, Jaxa-Chamiec T, Chwyczko T, et al. Cardiopulmonary exercise testing in adult cardiology: expert opinion of the Working Group of Cardiac Rehabilitation and Exercise Physiology of the Polish Cardiac Society. Kardiol Pol. 2019;77:730–56.
Toko H, Oka T, Zou Y, et al. Angiotensin II type 1a receptor mediates doxorubicin-induced cardiomyopathy. Hypertens Res. 2002;25:597–603.
Bien S, Riad A, Ritter CA, et al. The endothelin receptor blocker bosentan inhibits doxorubicin-induced cardiomyopathy. Cancer Res. 2007;67:10428–35.
Bernstein D, Fajardo G, Zhao M, et al. Differential cardioprotective/cardiotoxic effects mediated by beta-adrenergic receptor subtypes. Am J Physiol Heart Circ Physiol. 2005;289:H2441–9.
Lódi M, Priksz D, Fülöp GÁ, et al. Advantages of prophylactic versus conventionally scheduled heart failure therapy in an experimental model of doxorubicin-induced cardiomyopathy. J Transl Med. 2019;17(1):229. https://doi.org/10.1186/s12967-019-1978-0.
Bosch X, Rovira M, Sitges M, et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (Prevention of left ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive chemotherapy for the treatment of Malignant hEmopathies). J Am Coll Cardiol. 2013;61:2355–62.
Pituskin E, Mackey JR, Koshman S, et al. Multidisciplinary approach to novel therapies in cardio-oncology research (MANTICORE 101–breast): a randomized trial for the prevention of trastuzumab-associated cardiotoxicity. J Clin Oncol. 2016;35:870–7.
Gulati G, Heck SL, Ree AH, et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 × 2 factorial, randomized, placebo-controlled, double-blind clinical trial of Candesartan and Metoprolol. Eur Heart J. 2016;37:1671–80.
Kalay N, Basar E, Ozdogru I, et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2006;48(11):2258–62.
Jhorawat R, Kumari S, Varma SC, et al. Preventive role of carvedilol in adriamycin-induced cardiomyopathy. Indian J Med Res. 2016;144(5):725–9.
Nabati M, Janbabai G, Baghyari S, Esmaili K, Yazdani J. Cardioprotective effects of carvedilol in inhibiting doxorubicin-induced cardiotoxicity. J Cardiovasc Pharmacol. 2017;69(5):279–85.
Salehi R, Zamani B, Esfehani A, Ghafari S, Abasnezhad M, Goldust M. Protective effect of carvedilol in cardiomyopathy caused by anthracyclines in patients suffering from breast cancer and lymphoma. Am Heart Hosp J. 2011;9(2):95–8.
Georgakopoulos P, Roussou P, Matsakas E, et al. Cardioprotective effect of metoprolol and enalapril in doxorubicin-treated lymphoma patients: a prospective, parallel-group, randomized, controlled study with 36-month follow-up. Am J Hematol. 2010;85(11):894–6.
Avila MS, Ayub-Ferreira SM, de Barros Wanderley MR, et al. Carvedilol for prevention of chemotherapy-related cardiotoxicity: the CECCY trial. J Am Coll Cardiol. 2018;71(20):2281–90.
Barış VÖ, Dinçsoy AB, Gedikli E, Zırh S, Müftüoğlu S, Erdem A. Empagliflozin significantly prevents the doxorubicin-induced acute cardiotoxicity via non-antioxidant pathways. Cardiovasc Toxicol. 2021;21(9):747–58.
Hitawala G, Jain E, Castellanos L, et al. Pediatric chemotherapy drugs associated with cardiotoxicity. Cureus. 2021;13(11): e19658. https://doi.org/10.7759/cureus.19658.
Garcia-Pavia P, Kim Y, Restrepo-Cordoba MA, et al. Genetic variants associated with cancer therapy-induced cardiomyopathy. Circulation. 2019;140:31–4.
Lipshultz SE, Anderson LM, Miller TL, et al. Impaired mitochondrial function is abrogated by Dexrazoxane in doxorubicin-treated childhood acute lymphoblastic leukemia survivors. Cancer. 2016;122(6):946–53.
Aminkeng F, Bhavsar AP, Visscher H, et al. A coding variant in RARG confers susceptibility to anthracycline-induced cardiotoxicity in childhood cancer. Nat Genet. 2015;47(9):1079–84.
Magdy T, Jiang Z, Jouni M, et al. RARG variant predictive of doxorubicin-induced cardiotoxicity identifies a cardioprotective therapy. Cell Stem Cell. 2021;28(12):2076-2089.e7. https://doi.org/10.1016/j.stem.2021.08.006.
Wang X, Sun CL, Quinones-Lombrana A, et al. CELF4 variant and anthracycline-related cardiomyopathy: a Children’s Oncology Group genome-wide association study. J Clin Oncol. 2016;34(8):863–70.
Ohiri JC, McNally EM. Gene editing and gene-based therapeutics for cardiomyopathies. Heart Fail Clin. 2018;14(2):179–88.
Messinis DE, Melas IN, Hur J, Varshney N, Alexopoulos LG, Bai JPF. Translational systems pharmacology-based predictive assessment of drug-induced cardiomyopathy. CPT Pharmacometrics Syst Pharmacol. 2018;7(3):166–74.
Sapkota Y, Qin N, Ehrhardt MJ, et al. Genetic variants associated with therapy-related cardiomyopathy among childhood cancer survivors of African ancestry. Cancer Res. 2021;81(9):2556–65.
Vinodhini MT, Sneha S, Nagare RP, et al. Evaluation of a polymorphism in MYBPC3 in patients with anthracycline-induced cardiotoxicity. Indian Heart J. 2018;70(2):319–22.
Li L-P, Zhong J, Li M-H, et al. Disruption of MAP7D1 gene function increases the risk of doxorubicin-induced cardiomyopathy and heart failure. Biomed Res Int. 2021. https://doi.org/10.1155/2021/8569921.
Singh P, Wang X, Hageman L, et al. Association of GSTM1 null variant with anthracycline-related cardiomyopathy after childhood cancer—a Children’s Oncology Group ALTE03N1 report. Cancer. 2020;126(17):4051–8.
Anderson BS, Eksborg S, Vidal RF, Sundberg M, Carlberg M. Anthraquinone-induced cell injury: acute toxicity of actinomycin, epirubicin, idarubicin and mitoxantrone in isolated cardiomyocytes. Toxicology. 1999;135(1):11–20.
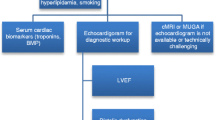
Leerink JM, Feijen EAM, Moerland PD, et al. Candidate plasma biomarkers to detect anthracycline-related cardiomyopathy in childhood cancer survivors: a case–control study in the Dutch Childhood Cancer Survivor study. J Am Heart Assoc. 2022;11(14): e025935.
Bisoc A, Ciurescu D, Rădoi M, et al. Natriuretic peptide levels in the serum can predict the development of anthracycline-induced cardiomyopathy. Am J Ther. 2020;27(2):e142–50.
Pudil R, Mueller C, Celutkiene J, et al. Role of serum biomarkers in cancer patients receiving cardiotoxic cancer therapies: a position statement from the Cardio-Oncology Study Group of the Heart Failure Association and the Cardio-Oncology Council of the European Society of Cardiology. Eur J Heart Fail. 2020;22:1966–83.
Lipshuntz SE, Landy DC, Lopez-Mitnik G, Lipsitz SR, Hinkle AS, Constine LS. Cardiovascular status of childhood cancer survivors exposed and unexposed to cardiotoxic therapy. J Clin Oncol. 2012;30:1050–7.
Zamorano JL, Lancellotti P, Aboyans V, et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC committee for practice guidelines. Eur Heart J. 2016;37(36):2768–801.
Thavendiranathan P, Grant AD, Negishi T, Plana JC, Popovi ZB, Marwick TH. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. J Am Coll Cardiol. 2013;61:77–84.
Moon TJ, Miyamoto S, Younosazai AK, Landeck BF. Left ventricular strain and strain rates are decreased in children with normal fractional shortening after exposure to anthracycline chemotherapy. Cardiol Young. 2014;24(5):854–65.
Akam-Venkata J, Kadiu G, Galas J, Lipshultz SE, Aggarwal S. Left ventricle segmental function in childhood cancer survivors using speckle-tracking echocardiography. Cardiol Young. 2019;29(12):1494–500.
Thavendiranathan P, Poulin F, Lim KD, Plana JC, Woo A, Marwick TH. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol. 2014;63:2751–68.
Negishi T, Thavendiranathan P, Penicka M, et al. Cardioprotection using strain-guided management of potentially cardiotoxic cancer therapy: 3-year results of the SUCCOUR trial. JACC Cardiovasc Imaging. 2023;16(3):269–78.
Doherty JU, Kort S, Mehran R, et al. ACC/AATS/AHA/ASE/ASNC/HRS/SCAI/SCCT/ SCMR/STS 2019 appropriate use criteria for multimodality imaging in the assessment of cardiac structure and function in nonvalvular heart disease: a report of the American College of Cardiology appropriate use criteria task force, American association for thoracic surgery, American heart association, American society of echocardiography, American society of nuclear cardiology, heart rhythm society, society for cardiovascular angiography and interventions, society of cardiovascular computed tomography, society for cardiovascular magnetic resonance, and the society of thoracic surgeons. J Am Coll Cardiol. 2019;73:488–516.
Deng S, Yan T, Jendrny C, et al. Dexrazoxane may prevent doxorubicin-induced DNA damage via depleting topoisomerase 2 isoforms. BMC Cancer. 2014;14:842. https://doi.org/10.1186/1471-2407-14-842.
Lue Y, Gao C, Swerdloff R, et al. Humanin analog enhances the protective effect of dexrazoxane against doxorubicin-induced cardiotoxicity. Am J Physiol Heart Circ Physiol. 2018;315:H634–43.
Wnag P, Wang L, Lu J, et al. SESN2 protects against doxorubicin-induced cardiomyopathy by rescuing mitophagy and improving mitochondrial function. J Mol Cell Cardiol. 2019;133:125–37.
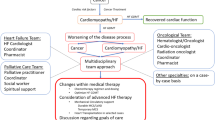
Cardinale D, Colombo A, Bacchiani G, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131:1981–8.
Gupta V, Singh SK, Agrawal V, Singh TB. Role of ACE inhibitors in anthracycline-induced cardiotoxicity: a randomized, double-blind, placebo-controlled trial. Pediatr Blood Cancer. 2018;65: e27308.
Silber JH, Cnaan A, Clark BJ, et al. Enalapril to prevent cardiac function decline in long-term survivors of pediatric cancer exposed to anthracyclines. J Clin Oncol. 2004;22:820–8.
Lipshultz SE, Lipsitz SR, Sallan SE, et al. Long-term enalapril therapy for left ventricular dysfunction in doxorubicin-treated survivors of childhood cancer. J Clin Oncol. 2002;20:4517–22.
Armenian S, Bhatia S. Predicting and preventing anthracycline-related cardiotoxicity. Am Soc Clin Oncol Educ Book. 2018;38:3–12.
Huang S, Zhao Q, Yang ZG, et al. Protective role of beta-blockers in chemotherapy-induced cardiotoxicity—a systematic review and meta-analysis of carvedilol. Heart Fail Rev. 2019;24(3):325–33.
El-Shitany NA, Tolba OA, El-Shanshory MR, El-Hawary EE. Protective effect of carvedilol on adriamycin-induced left ventricular dysfunction in children with acute lymphoblastic leukemia. J Card Fail. 2012;18:607–13.
Armenian SH, Hudson MM, Chen MH, et al. Rationale and design of the Children’s Oncology Group (COG) study ALTE1621: a randomized, placebo-controlled trial to determine if low-dose carvedilol can prevent anthracycline-related left ventricular remodeling in childhood cancer survivors at high risk for developing heart failure. BMC Cardiovasc Disord. 2016;16(1):187. https://doi.org/10.1186/s12872-016-0364-6.
Das B, Deshpande S, Venkata JA, Shakti D, Moskowitz W, Lipshulz SE. Heart failure with preserved ejection fraction in children. Pediatr Cardiol. 2022. https://doi.org/10.1007/s00246-022-02960-7.
Das B, Moskowitz W, Butler J. Current and future drug and device therapies for pediatric heart failure patients: potential lessons from adult trials. Children. 2021;8(5):322. https://doi.org/10.3390/children8050322
Kirk R, Dipchand AI, Rosenthal DN, et al. The International Society for Heart and Lung Transplantation guidelines for the management of pediatric heart failure executive summary. J Heart Lung Transplant. 2014;33:888–909.
Franco VI, Lipshultz SE. Cardiac complications in childhood cancer survivors treated with anthracyclines. Cardiol Young. 2015;25(Suppl 2):107–16.
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2022;145:e895–1032.
De Marzo V, Savarese G, Tricarcio L, et al. Network meta-analysis of medical therapy efficacy in more than 90,000 patients with heart failure and reduced ejection fraction. J Intern Med. 2022;292:333–49.
Frey MK, Arfsten H, Pavo N, et al. Sacubitril/valsartan is well tolerated in patients with long-standing heart failure and history of cancer and improves ventricular function: real-world data. Cardio-Oncol. 2021;7:1–6.
Gregorietti V, Fernandez TL, Costa D, Chahla EO, Daniele AJ. Use of Sacubitril/valsartan in patients with cardiotoxicity and heart failure due to chemotherapy. Cardio-Oncology. 2020;6:1–6.
Sheppard CE, Anwar M. The use of sacubitril/valsartan in anthracycline-induced cardiomyopathy: a mini case series. J Oncol Pharm Pract. 2019;25(5):1231–4.
Martín-García A, Díaz-Peláez E, Martín-García AC, et al. Myocardial function and structure improvement with sacubitril/valsartan in cancer therapy-induced cardiomyopathy. Rev Esp Cardiol (Engl Ed). 2020;73(3):268–9.
Mecinaj A, Gulati G, Heck SL, et al. Rationale and design of the prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA II) trial: a randomized, placebo-controlled, multicenter trial. Cardiooncology. 2021;2021(7):33. https://doi.org/10.1186/s40959-021-00115-w.
Chiang CH, Chiang CH, Chiang CH, et al. Impact of sodium–glucose cotransporter-2 inhibitors on heart failure and mortality in patients with cancer. Heart. 2023;109:470–7.
Gongora CA, Drobni ZD, Costa Silva TQA, et al. Sodium–glucose co-3transporter-2 inhibitors and cardiac outcomes among patients treated with anthracyclines. JACC Heart Fail. 2022;10(8):559–67.
Khouri MG, Greene SJ. Sodium–glucose co-transporter-2 inhibitor therapy [y during anthracycline treatment: is there a role of cardioprotection? JACC Heart Fail. 2022;10:568–70.
Newland DM, Law YM, Albers EL, et al. Early clinical experience with dapagliflozin in children with heart failure. Ped Cardiol. 2023;44:146–52.
Azer J, Hua R, Krishnaswamy PS, Rose RA. Effects of natriuretic peptides on electrical conduction in the sinoatrial node and atrial myocardium of the heart. J Physiol. 2014;592:1025–45.
Armstrong PW, Pieske B, Anstrom KJ, et al. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020;382:1883–93.
Nagiub M, Filippone D, Durrant D, Das A, Kukreja RC. Long-acting PDE5 inhibitor tadalafil prevents early doxorubicin-induced left ventricle diastolic dysfunction in juvenile mice: potential role of cytoskeletal proteins. Can J Physiol Pharmacol. 2017;95:295–304.
Frisk M, Le C, Shen X, et al. Etiology-dependent impairment of diastolic cardiomyocyte calcium homeostasis in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2021;4:405–19.
Merck Sharp & Dohme LLC (sponsors). Efficacy, safety, and pharmacokinetics of vericiguat in pediatric participants with heart failure due to left ventricular systolic dysfunction (MK-1242-036). ClinicalTrials.gov identifier (NCT number): NCT0571408592.
Kosmala W, Marwick TH. Asymptomatic left ventricular diastolic dysfunction: predicting progression to symptomatic heart failure. JACC Cardiovasc Imaging. 2020;13:215–7.
Yu W, Li SN, Chan GC, et al. Transmural Strain and rotation gradient in survivors of childhood cancers. Eur Heart J Cardiovasc Imaging. 2013;14:175–82.
Lipshultz SE, Scully R, Stevenson KE, et al. Hearts too small for body size after doxorubicin for childhood ALL: Grinch syndrome. J Clin Oncol. 2014;32(suppl):10021A.
Das B. Therapeutic approaches in heart failure with preserved ejection fraction (HFpEF) in children: present and future. Pediatr Drugs. 2022;24(3):235–46.
Minotti G, Menna P, Camilli M, Salvatorelli E, Levi R. Beyond hypertension: diastolic dysfunction associated with cancer treatment in the era of cardio-oncology. Adv Pharmacol. 2022;94:365–409.
Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E. Prospective comparison of ARNI with ARB on management of heart failure with preserved ejection fraction (PARAMOUNT) investigators. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind, randomized controlled trial. Lancet. 2012;380:1387–95.
Packer M, Butler J, Zannad F, et al. Effect of empagliflozin on worsening heart failure events in patients with heart failure and a preserved ejection fraction: the EMPEROR-preserved trial. Circulation. 2021;144:1284–9.
Sabatino J, De Rosa S, Tammè L, et al. Empagliflozin prevents doxorubicin-induced myocardial dysfunction. Cardiovasc Diabetol. 2020;19:66. https://doi.org/10.1186/s12933-020-01040-5].
Bianco C, Al-Kindi SG, Oliveira GH. Advanced heart failure therapies for cancer therapeutics-related cardiac dysfunction. Heart Fail Clin. 2017;13:327–36.
Fadol AP, Mouhavar E, Reyes-Gibby CC. The use of cardiac resynchronization therapy in cancer patients with heart failure. J Clin Exp Res Cardiol. 2017;3(1). https://doi.org/10.15744/2394-6504.3.105.
Oliveira GH, Qattan MY, Al-Kindi S, Park SJ. Advanced heart failure therapies for patients with chemotherapy-induced cardiomyopathy. Circ Heart Fail. 2014;7:1050–8.
Ezzeddine FM, Saliba AN, Jain V, et al. Outcomes of cardiac resynchronization therapy in patients with chemotherapy-induced cardiomyopathy. Pacing Clin Electrophysiol. 2021;44(4):625–32.
Singh JP, Solomon SD, Fradley MG, MADIT-CHIC Investigators, et al. Association of cardiac resynchronization therapy with change in left ventricular ejection fraction in patients with chemotherapy-induced cardiomyopathy. JAMA. 2019;322(18):1799–805.
Rickard J, Kumbhani DJ, Baranowski B, Martin DO, Tang WH, Wilkoff BL. The usefulness of cardiac resynchronization therapy in patients with adriamycin-induced cardiomyopathy. Am J Cardiol. 2010;105(4):522–6.
Patel D, Kumar A, Moennich LA, et al. Cardiac resynchronization therapy in anthracycline-induced cardiomyopathy. Heart. 2022;108(4):274–8.
Jones BO, Davis A, Alison J, Weintraub RG, Butt W, Cheung MM. Cardiac resynchronization therapy in a child with severe anthracycline-induced congestive heart failure and normal QRS duration. J Heart Lung Transplant. 2007;26:1333–5.
Schlam I, Lee AY, Li S, et al. LeftVentricular assist devices in patients with active malignancies. JACC Cardio Oncol. 2021;3:305–15.
Oliveira GH, Dupont M, Naftel D, et al. Increased need for right ventricular support in patients with chemotherapy-induced cardiomyopathy undergoing mechanical circulatory support: outcomes from the INTERMACS Registry (Interagency Registry for Mechanically Assisted Circulatory Support). J Am Coll Cardiol. 2014;63:240–8.
Puri K, Denfield SW, Adachi I, et al. Ventricular assist device support for children with chemotherapy-induced cardiomyopathy and advanced heart failure: perspectives gained from a single-center experience. Pediatr Transplant. 2022;26: e14286.
Oliveira GH, Hardaway BW, Kucheryavaya AY, Stehlik J, Edwards LB, Taylor DO. Characteristics and survival of patients with chemotherapy-induced cardiomyopathy undergoing heart transplantation. J Heart Lung Transplant. 2012;31:805–10.
Shugh SB, Ryan TD. Heart transplantation in survivors of childhood cancer. Transl Pediatr. 2019;8(4):314–21.
Sayed N, Ameen M, Wu JC. Personalized medicine in cardio-oncology: the role of induced pluripotent stem cell. Cardiovasc Res. 2019;115:949–59.
Santos DSD, Brasil GV, Ramos IPR, et al. Embryonic stem cell-derived cardiomyocytes for the treatment of doxorubicin-induced cardiomyopathy. Stem Cell Res Ther. 2018;9(1):30. https://doi.org/10.1186/s13287-018-0788-2.
Acknowledgements
Ms Sabrina M. Freeman, BSN, RN, has edited the manuscript for English and grammar.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of interest
Bibhuti Das has no potential conflicts of interest that might be relevant to the contents of this manuscript.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
BD: Conceptualized, wrote, and revised this manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Das, B. Pharmacotherapy for Cancer Treatment-Related Cardiac Dysfunction and Heart Failure in Childhood Cancer Survivors. Pediatr Drugs 25, 695–707 (2023). https://doi.org/10.1007/s40272-023-00585-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-023-00585-8