Abstract
Background
Identifying past temporal trends in non-alcoholic steatohepatitis (NASH)-associated liver cancer (NALC) can increase public awareness of the disease and facilitate future policy development.
Methods
Annual deaths and age-standardized death rates (ASDR) for NALC from 1990 to 2019 were collected from the Global Burden of Disease (GBD) 2019 study. The long-term trend and the critical inflection of mortality of NALC were detected by Joinpoint analysis. Age–period–cohort analysis was employed to evaluate the effects of age, period, and cohort. Last, decomposition analysis was used to reveal the aging and population growth effects for NALC burden.
Results
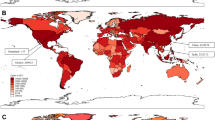
Between 1990 and 2019, the ASDR of NALC witnessed an overall declining trend on a global scale, with a decrease in females and a stable trend in males. However, the global ASDR demonstrated a significant upward trend from 2010 to 2019. Southern sub-Saharan Africa and Southeast Asia have the highest NALC burdens, while high socio-demographic index (SDI) region experienced the fastest escalation of NALC burdens over 30 years. The decomposition analysis revealed that population growth and aging were the primary catalysts behind the increase in global NALC deaths. Age–period–cohort analyses showed that NALC mortality declined the fastest among females aged 40–45 years in high SDI region, accompanied by a deteriorating period effect trend during the period of 2010–2019.
Conclusion
The global absolute deaths and ASDR of NALC have witnessed a rise in the past decade, with populations exhibiting considerable disparities based on sex, age, and region. Population growth, aging, and metabolism-related factors were the main factors behind the increase in global NALC deaths.





Similar content being viewed by others
Data availability
The data that support the findings of this study are openly available in https://ghdx.healthdata.org.
Abbreviations
- AAPC:
-
Average annual percentage change
- APC:
-
Annual percentage change
- ASDR:
-
Age-standardized death rate
- CI:
-
Confidence interval
- GBD:
-
Global Burden of Disease
- NASH:
-
Non-alcoholic steatohepatitis
- NAFLD:
-
Non-alcoholic fatty liver disease
- NALC:
-
NASH-associated liver cancer
- SDI:
-
Socio-demographic index
- T2DM:
-
Type 2 diabetes mellitus
- UI:
-
Uncertainty interval
- WHO:
-
World Health Organization
References
Gutiérrez-Cuevas J, Lucano-Landeros S, López-Cifuentes D, et al. Epidemiologic, genetic, pathogenic, metabolic, epigenetic aspects involved in NASH-HCC: current therapeutic strategies. Cancers (Basel). 2022;15:23.
Younossi ZM, Golabi P, Paik JM, et al. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology. 2023;77:1335–47.
Powell EE, Wong VW, Rinella M. Non-alcoholic fatty liver disease. Lancet. 2021;397:2212–24.
Li Z, Yang N, He L, et al. Estimates and trends of the global burden of NASH-related liver cancer attributable to high fasting plasma glucose in 1990–2019: analysis of data from the 2019 global burden of disease study. Diabetol Metab Syndr. 2023;15:6.
Tan DJH, Ng CH, Lin SY, et al. Clinical characteristics, surveillance, treatment allocation, and outcomes of non-alcoholic fatty liver disease-related hepatocellular carcinoma: a systematic review and meta-analysis. Lancet Oncol. 2022;23:521–30.
Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84.
Targher G, Corey KE, Byrne CD, et al. The complex link between NAFLD and type 2 diabetes mellitus - mechanisms and treatments. Nat Rev Gastroenterol Hepatol. 2021;18:599–612.
United Nations DoEaSA, population division (2019). World population prospects 2019: highlights (ST/ESA/SER.A/423). In.
Cheng X, Yang Y, Schwebel DC, et al. Population ageing and mortality during 1990–2017: a global decomposition analysis. PLoS Med. 2020;17: e1003138.
Liu Y, Zheng J, Hao J, et al. Global burden of primary liver cancer by five etiologies and global prediction by 2035 based on global burden of disease study 2019. Cancer Med. 2022;11:1310–23.
Choi S, Kim BK, Yon DK, et al. Global burden of primary liver cancer and its association with underlying aetiologies, sociodemographic status, and sex differences from 1990–2019: A DALY-based analysis of the global burden of disease 2019 study. Clin Mol Hepatol. 2023;29:433–52.
Pang J, Chen K, Chen S, et al. Global burden of nonalcoholic steatohepatitis-related liver cancer, 1990–2019: a systematic analysis for the GBD 2019. Diabetol Metab Syndr. 2022;14:112.
Mubarik S, Yu Y, Wang F, et al. Epidemiological and sociodemographic transitions of female breast cancer incidence, death, case fatality and DALYs in 21 world regions and globally, from 1990 to 2017: an age-period-cohort analysis. J Adv Res. 2022;37:185–96.
GBD 2019 diseases and injuries collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396:1204–22.
GBD 2019 risk factors collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396:1223–49.
Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51.
Zhu S, Zhang F, Zhao G, et al. Trends in the global burden of oral cancer joint with attributable risk factors: Results from the global burden of disease study 2019. Oral Oncol. 2022;134: 106189.
Rosenberg PS, Check DP, Anderson WF. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2014;23:2296–302.
Das Gupta P. Standardization and decomposition of rates from cross-classified data. Genus. 1994;50:171–96.
Gupta PD: Standardization and decomposition of rates: a users’s manual. washington d 1993.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Younossi ZM, Loomba R, Anstee QM, et al. Diagnostic modalities for nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, and associated fibrosis. Hepatology. 2018;68:349–60.
Gutiérrez-Cuevas J, Santos A, Armendariz-Borunda J. Pathophysiological molecular mechanisms of obesity: a link between MAFLD and NASH with cardiovascular diseases. Int J Mol Sci. 2021;22:11629.
Zhou J, Zhou F, Wang W, et al. Epidemiological features of NAFLD from 1999 to 2018 in China. Hepatology. 2020;71:1851–64.
Han A, Sun T, Ming J, et al. Are the Chinese moving toward a healthy diet? Evidence from macro data from 1961 to 2017. Int J Environ Res Public Health. 2020;17:5294.
Yang Y, Hu XM, Chen TJ, et al. Rural-urban differences of dietary patterns, overweight, and bone mineral status in Chinese students. Nutrients. 2016;8:537.
Wang W, Ren J, Zhou W, et al. Lean non-alcoholic fatty liver disease (Lean-NAFLD) and the development of metabolic syndrome: a retrospective study. Sci Rep. 2022;12:10977.
Wang Y, Zhao L, Gao L, et al. Health policy and public health implications of obesity in China. Lancet Diabetes Endocrinol. 2021;9:446–61.
Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol. 2017;960:1–17.
Seidell JC, Halberstadt J. The global burden of obesity and the challenges of prevention. Ann Nutr Metab. 2015;66(Suppl 2):7–12.
Wang D, Xu Y, Zhu Z, et al. Changes in the global, regional, and national burdens of NAFLD from 1990 to 2019: a systematic analysis of the global burden of disease study 2019. Front Nutr. 2022;9:1047129.
Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022;133: 155217.
Pirillo A, Casula M, Olmastroni E, et al. Global epidemiology of dyslipidaemias. Nat Rev Cardiol. 2021;18:689–700.
Friedman SL, Neuschwander-Tetri BA, Rinella M, et al. Mechanisms of NAFLD development and therapeutic strategies. Nat Med. 2018;24:908–22.
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of Type 2 diabetes mellitus. Endocr Rev. 2016;37:278–316.
Tchernof A, Després JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93:359–404.
Maric C. Sex differences in cardiovascular disease and hypertension: involvement of the renin-angiotensin system. Hypertension. 2005;46:475–6.
DiStefano JK. NAFLD and NASH in postmenopausal women: implications for diagnosis and treatment. Endocrinology. 2020;161:bqaa134.
Camhi SM, Bray GA, Bouchard C, et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity (Silver Spring). 2011;19:402–8.
Calcinotto A, Kohli J, Zagato E, et al. Cellular senescence: aging, cancer, and injury. Physiol Rev. 2019;99:1047–78.
Aunan JR, Cho WC, Søreide K. The biology of aging and cancer: a brief overview of shared and divergent molecular hallmarks. Aging Dis. 2017;8:628–42.
Campisi J. Aging, cellular senescence, and cancer. Annu Rev Physiol. 2013;75:685–705.
Aunan JR, Watson MM, Hagland HR, et al. Molecular and biological hallmarks of ageing. Br J Surg. 2016;103:e29-46.
Taddei S, Virdis A, Ghiadoni L, et al. Endothelium, aging, and hypertension. Curr Hypertens Rep. 2006;8:84–9.
Wu W, Feng A, Ma W, et al. Worldwide long-term trends in the incidence of nonalcoholic fatty liver disease during 1990–2019: a joinpoint and age-period-cohort analysis. Front Cardiovasc Med. 2022;9: 891963.
Younes R, Caviglia GP, Govaere O, et al. Long-term outcomes and predictive ability of non-invasive scoring systems in patients with non-alcoholic fatty liver disease. J Hepatol. 2021;75:786–94.
Di Mauro S, Scamporrino A, Filippello A, et al. Clinical and molecular biomarkers for diagnosis and staging of NAFLD. Int J Mol Sci. 2021;22:11950.
Tapper EB, Loomba R. Noninvasive imaging biomarker assessment of liver fibrosis by elastography in NAFLD. Nat Rev Gastroenterol Hepatol. 2018;15:274–82.
Wong VW, Adams LA, de Lédinghen V, et al. Noninvasive biomarkers in NAFLD and NASH - current progress and future promise. Nat Rev Gastroenterol Hepatol. 2018;15:461–78.
Mason WM, Fienberg SE. Introduction: beyond the identification problem. In: Mason WM, Fienberg SE, editors. Cohort analysis in social research: beyond the identification problem. New York, NY: Springer New York; 1985. p. 1–8.
Song C, Wang M, Chen Z, et al. Fetal exposure to Chinese famine increases obesity risk in adulthood. Int J Environ Res Public Health. 2020;17:3649.
Shi Z, Ji L, Ma RCW, et al. Early life exposure to 1959–1961 Chinese famine exacerbates association between diabetes and cardiovascular disease. J Diabetes. 2020;12:134–41.
Lazarus JV, Mark HE, Anstee QM, et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol. 2022;19:60–78.
Ioannou GN. Epidemiology and risk-stratification of NAFLD-associated HCC. J Hepatol. 2021;75:1476–84.
Arab JP, Dirchwolf M, Álvares-da-Silva MR, et al. Latin American association for the study of the liver (ALEH) practice guidance for the diagnosis and treatment of non-alcoholic fatty liver disease. Ann Hepatol. 2020;19:674–90.
Frohme J, Tacke F. The socioeconomic aspects of nonalcoholic fatty liver disease: food insecurity as a novel risk factor for steatosis and liver fibrosis. Hepatobiliary Surg Nutr. 2020;9:543–5.
Lazarus JV, Mark HE, Villota-Rivas M, et al. The global NAFLD policy review and preparedness index: are countries ready to address this silent public health challenge? J Hepatol. 2022;76:771–80.
Acknowledgements
We acknowledge GBD2019 collaborators whose outstanding contributions have enabled us to complete this study.
Funding
This study was supported by the project of the Institute of Hospital Management, National Health Care Commission (YLZLXZ22G026) and the self-funded science and technology program of Fuyang City (FK202081016).
Author information
Authors and Affiliations
Contributions
CL, SZ, and JZ: Writing – original draft, Writing – review & editing, Methodology, Formal analysis, Validation, Visualization. XW and PW: Writing – review & editing, Resources, Validation, Data curation. SD and EW: Writing – review & editing, Validation, Data curation. YK: Writing – review & editing, Data curation. KS: Conceptualization, Writing – review & editing, Funding acquisition. JY: Conceptualization, Writing – review & editing, Supervision.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. No support from any organization or activities for the submitted work.
Ethical approval and consent to participate
Ethical approval and consent were not required as this study was based on publicly available data.
Informed consent
N/A.
Registry and the registration No. of the study/trial
N/A.
Animal studies
N/A.
Research involving recombinant DNA
N/A.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, C., Zhu, S., Zhang, J. et al. Global, regional, and national burden of liver cancer due to non-alcoholic steatohepatitis, 1990–2019: a decomposition and age–period–cohort analysis. J Gastroenterol 58, 1222–1236 (2023). https://doi.org/10.1007/s00535-023-02040-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-023-02040-4