Abstract
DrugCentral, accessible at https://drugcentral.org, is an open-access online drug information repository. It covers over 4950 drugs, incorporating structural, physicochemical, and pharmacological details to support drug discovery, development, and repositioning. With around 20,000 bioactivity data points, manual curation enhances information from several major digital sources. Approximately 724 mechanism-of-action (MoA) targets offer updated drug target insights. The platform captures clinical data: over 14,300 on- and off-label uses, 27,000 contraindications, and around 340,000 adverse drug events from pharmacovigilance reports. DrugCentral encompasses information from molecular structures to marketed formulations, providing a comprehensive pharmaceutical reference. Users can easily navigate basic drug information and key features, making DrugCentral a versatile, unique resource. Furthermore, we present a use-case example where we utilize experimentally determined data from DrugCentral to support drug repurposing. A minimum activity threshold t should be considered against novel targets to repurpose a drug. Analyzing 1156 bioactivities for human MoA targets suggests a general threshold of 1 µM: t = 6 when expressed as − log[Activity(M)]). This applies to 87% of the drugs. Moreover, t can be refined empirically based on water solubility (S): t = 3 − logS, for logS < − 3. Alongside the drug repurposing classification scheme, which considers intellectual property rights, market exclusivity protections, and market accessibility, DrugCentral provides valuable data to prioritize candidates for drug repurposing programs efficiently.
Similar content being viewed by others
Introduction
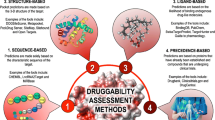
DrugCentral (http://drugcentral.org), established in 2016 [1] is an open-access drug compendium that connects the scientific basis of drug substances to approved pharmaceutical products for healthcare professionals. It encompasses drug structures and properties, regulatory details, bioactivity profiles, mechanism-of-action (MoA) targets, pharmacological actions, therapeutic applications and contraindications, adverse events, and drug formulations and products. Figure 1 demonstrates the main components and their links. Although some information is manually curated from scientific literature and drug labels, most data is aggregated from public online resources [1,2,3,4].
DrugCentral tracks drug approvals from three major regulatory agencies: the U.S. Food and Drug Administration (FDA) [5], European Medicines Agency (EMA) [6], and Japan Pharmaceutical and Medical Devices Agency (PMDA) [7]. In the last decade, the number of drugs approved for the first time per year varied between 29 and 70. Overall, the moving average of the past 10 years indicates an increasing trend (Fig. 2).
Here we describe DrugCentral content (related to 4959 drugs) with various features and functionalities (based on the entire 2022 release) added during the past years [1,2,3,4]. We briefly discuss drug properties, targets, clinical effects, drug products, pharmaceutical formulations, and data accessibility.
Drug properties
DrugCentral comprises 4959 active drug substances approved for human (4805) and veterinary use (396) [4], with properties computed or sourced externally. Various classification schemes, such as drug types, pharmacological classes, market availability, and patent coverage, enable users to select specific data sets. External identifiers link DrugCentral entries to complementary databases, creating a network of interconnected resources that provide users with a broad range of drug information.
Types of drugs
DrugCentral categorizes drugs into distinct types: small molecules, peptides, biologics (antibodies, antibody–drug conjugates, proteins, fused-proteins, oligonucleotides, small interfering RNA), and others (coordination, dendrimer, inorganic and organometallic molecules, polymer and radiopharmaceuticals). The majority of entries are small organic molecules (82.8%, 4108 entries), while peptides (133 entries) and biologics (260 entries) constitute 7.9% of the total (Table 1). Since 2020, biologics have gained traction, making up one-third of new approvals (59 out of 178). DrugCentral data indicates that 40.3% of all approved biologics have orphan designations. Conversely, only 6.8% of small molecules and 18% of peptide drugs are approved for rare diseases (Table 1).
Chemical structures and descriptors
Small-molecule and peptide drug chemical structures are accurately represented at the molecular level, with manual entry using depictions and information from sources like the WHO-INN [8]; United States Adopted Name, USAN [9]; and FDA drug labels [4]. Occasionally, information is verified through Chemical Abstract Service, CAS [9]. Drugs are standardized as follows: (i) Ionic salts have counterions removed and hydrated/solvated drug formulations have water/solvent removed (e.g., various atorvastatin calcium formulations are mapped to the single active ingredient, atorvastatin); (ii) Ester prodrugs are stored as-is (e.g., olmesartan medoxomil instead of its active metabolite, olmesartan); both enalapril and enalaprilat are indexed as enalapril is formulated both as a free acid and as the maleate salt of enalapril, the ethyl ester of enalaprilat [1].
Chemical structures of 4288 drugs have been manually entered and validated, with molecular weight (MW) spanning from 4 (Helium, a medically-used noble gas) to 22,125 a.m.u. (somatotropin, a 191-amino acid protein growth hormone). Several physicochemical properties relevant to drug analysis are available for small organic molecules, including the key properties used in the Lipinski rule of 5 (Ro5) criteria [10]: MW, number of rotatable bonds (RTB) [11], hydrogen bond donors/acceptors (HBD, HBA), and the calculated 1-octanol/water partition coefficient, CLOGP [12]—calculated using Biobyte software (http://www.biobyte.com/). Other properties encompass the number of rings and the topological polar surface area, TPSA [13]. DrugCentral enhances the chemical profiles of drugs, essential for understanding pharmacokinetics and toxicity, by calculating protonation constants with MOKA 3.0 software [14].
Figure 3 displays the distribution of six well-known properties calculated for 4092 small-molecule drugs (MW < 1250 a.m.u.). Median values are 326 for MW, 2.48 for CLOGP, 67.3 for TPSA, 5 for RTB, 5 for HBA, and 1 for HBD. Ninetieth percentile values for these physicochemical properties of drugs are as follows: MW ≤ 550, CLOGP ≤ 5.5, TPSA ≤ 145, RTB ≤ 10, HBA ≤ 10, HBD ≤ 4. The majority of these drugs (75%) are Ro5 compliant.
Pharmacology and external links
Pharmacokinetics
DrugCentral captures pharmacokinetics (absorption, distribution, metabolism, and excretion) using nine representative properties: BDDCS, biopharmaceutical drug disposition classification system [15]; the maximum recommended therapeutic daily dose, MRTD; clearance, Cl; half-life T1/2; the volume of distribution, Vd; absolute oral bioavailability, BA; the extent of metabolism, EoM; fraction unbound, fu; and water solubility, S [3]. Except for the last three, these properties are accessible for over 900 drugs each [3].
Pharmacologic classes
DrugCentral provides a range of pharmacological classifications. The manual allocation of WHO INN [8] stems allows for categorization based on chemical and pharmacological attributes. Where possible, drugs are connected to the most recent versions of ChEBI ontology [16], Medical Subject Headings, MeSH terms [17], and the FDA Established Pharmacologic Class, EPC [18]. In DrugCentral, 4230 unique drugs are linked to 2721 pharmaco-chemical class codes, with the distribution displayed in Table 2.
Drug repositioning categories
DrugCentral implemented a multi-category drug repositioning scheme [19], capturing information on patent and market status. Drugs are categorized based on intellectual property rights, market exclusivity protections, and market accessibility: off-patent (OFP) for on-market drugs with expired patents/exclusivities; on-patent (ONP) for on-patent, on-market drugs with active patents/exclusivity rights; and off-market (OFM) for discontinued or withdrawn drugs. This classification aids the drug repurposing and repositioning community, with 279 drugs as ONP, 1038 as OFP, and 402 as OFM. Drug repositioning strategies should prioritize drugs based on their intellectual property landscape and marketing status in the following order: (i) OFP, (ii) OFM, and (iii) ONP [19].
External identifiers
DrugCentral utilizes external digital resources for swift access to complementary data. CAS registry numbers [20], WHO INN IDs, and KEGG identifiers [21] are manually curated, while twelve other identifiers are automatically assigned based on drug names, synonyms, and chemical structures (InChIKey). Figure 4 displays the current number of identifiers and corresponding drug count in DrugCentral.
Drug targets and bioactivity data
DrugCentral captures quantitative bioactivity data for drug-target interactions when available. Comprehensive drug-target bioactivity profiles are compiled through automated extraction from multiple digital resources and enhanced by manual curation. This includes MoA (mechanism of action) targets, which are molecules (e.g., proteins, biopolymers, metabolites, metal atoms, drugs) that the drug (or its active metabolite) binds to for the intended therapeutic effect [22]. DrugCentral manually assigns MoA designations [23], offering a mechanistic understanding of drug actions related to human diseases and symptoms at the molecular level. MoA targets are manually annotated in DrugCentral using a curated list of external resources and expert curation. Drug labels and data reviewed by regulatory agencies are the primary sources for MoA target assignments. For approved drugs lacking this information in drug label data (e.g., pre-1990s approved drugs, some PMDA-approved drugs), MoA targets are critically assessed using scientific literature [23].
Bioactivity data
DrugCentral contains 20,658 activity endpoints (drug-target pairs) for 2715 drugs across 3171 targets. Bioactivities are compiled from various sources: ChEMBLdb [24] (59.7%), WOMBAT-PK [25] (13.8%), DrugMatrix [26] (11.0%), IUPHAR/BPS Guide to Pharmacology [27] (6.1%), scientific literature (3.7%), PDSP [28] (3.6%), and drug labels (1.6%) (Table 3). Multiple types of bioactivity data are stored: dissociation constants (Kd), and inhibition constants (Ki) but also inhibitory concentrations 50% (IC50) and effective concentrations 50% (EC50) accounting for drug-target interactions. Most activity determinations consist of Ki (7871) and IC50 (6043) values, followed by Kd (4141) and EC50 (898) values. Since IC50 and EC50 generally depend on assay details (such as concentration and Km of the substrate), users are advised to carefully check assay details when using bioactivity data to interpret in vivo effects. Among drug targets, 1795 (56.6%) are of human origin and interact with 2455 drugs.
Target classes
In DrugCentral’s bioactivity data, the largest target group are enzymes (53.5%; 15.6% are kinases), followed by G protein-coupled receptors—GPCRs (15.1%), and ion channels (11.1%). Most drugs (71%) target enzymes and GPCRs. The number of drugs exceeds the number of targets (Fig. 5), except for protein kinases, indicating a lack of selectivity among protein kinase inhibitors [19, 30, 31].
Mechanism-of-action targets
DrugCentral indexes 724 mechanism-of-action (MoA) protein targets (598 of human origin) with referenced UniProt IDs for 1905 drugs. Most of the MoA activity data (81% of 3491 activities) are derived from ChEMBL, WOMBAT-PK, and scientific literature (Table 3). Enzymes (34.9%), GPCRs (15.7%), and ion channels (14.6%) make up the majority of targets (473 in total), accounting for the therapeutic effects of 1287 drugs (68%). This includes 1148 small organic molecules targeting 413 enzymes, GPCRs, and ion channels as MoA targets. Within the group of biologics, monoclonal antibodies (mAb) are the most represented (91 drugs), binding to 57 MoA targets. Most of these targets are cytokines, surface antigens, and membrane receptors. Between 12 and 17 new MoA targets have appeared yearly, with increasing trends of mAb and ADCs over small molecule drugs, according to the Nature Reviews Drug Discovery TargetWatch series (Table 4) [32,33,34,35,36].
Target development levels
DrugCentral employs a knowledge-based classification scheme for targets, categorizing human proteins into four classes based on their target development level (TDL) [37]:
-
Tclin—assigned to drug targets involved in the MoA of approved drugs.
-
Tchem—annotates proteins known to bind small molecules with high affinity but not Tclin.
-
Tbio—designates proteins with significant biological experimental data available.
-
Tdark—refers to understudied proteins (covering ~ 29% of the human proteome).
Currently, DrugCentral has 709 Tclin and 485 Tchem targets, which are supplied (with supporting information) to the Target Central Resources Database (TCRD) [38] and further linked to the Pharos portal [38, 39].
Drug uses and adverse events
DrugCentral indexes drug-disease information, including approved and off-label uses, contraindications, and adverse events. Regulatory agencies grant drug approval based on substantial evidence of safety and efficacy for specific clinical situations, as indicated in the drug label (on-label drug use or drug indication). However, once a drug is on the market, physicians (or healthcare providers) can prescribe it off-label to address clinical conditions or diseases that are not on the list of approved indications. Off-label usage often supplements existing therapies to treat diseases without approved treatment options. DrugCentral provides information on therapeutic uses (on-label and off-label) and contraindications for a comprehensive understanding of the drug’s applications. Furthermore, pharmacovigilance data processed from the FDA’s Adverse Event Reporting System (FAERS) [40] is integrated into DrugCentral entries, providing details on adverse drug reactions. Currently, DrugCentral includes therapeutic use and adverse event information for 3278 drugs.
Indications, contraindications, and off-label uses
In DrugCentral, indications, contraindications, and off-label uses have been extracted from the OMOP data model version 4.4 up to 2012. The OMOP project then transitioned to OHDSI [41], which restricted access to such data. Consequently, all information after 2012 has been manually curated from approved drug labels. The current version of DrugCentral indexes 11,775 drug-indication pairs, 2542 drug-off-label use cases, and 27,671 drug-contraindication pairs. The vocabulary (medical concept terms) describing the related diseases and health conditions in DrugCentral has been mapped to SNOMED-CT [42] and UMLS [43]. This further enables extending the mappings to other terminologies, such as disease-ontology [44]. Out of 2497 medical concepts describing drug indications, approximately 65% have been mapped to existing dictionaries and ontologies, as shown in Table 5.
FDA adverse event reporting system
DrugCentral indexes FDA FAERS data based on drug names, drug product names, and UNII identifiers [45]. FAERS data not reported by healthcare professionals is discarded, and only ‘suspected drugs’ with more than three reports for each adverse event are considered. Concept names are mapped as MedDRA terms (Medical Dictionary for Regulatory Activities) [46]. The Likelihood Ratio Test (LRT) signal detection procedure [47] is applied to identify drug-MedDRA term combinations with disproportionally high reporting rates. Critical values based on a p-value < 0.05 under the null hypothesis H0 are computed and stored in DrugCentral. H0 compares the reporting rate for a MedDRA term for a drug against the reporting rates for all other MedDRA terms for that same drug. This comparison enables users to post-process the data using other criteria [2]. Significant signals are events with log-likelihood ratios (LLRs) larger than the calculated drug-specific threshold values (LLRT). Since 2020, the procedure has been applied separately for women and men, supporting analyses of sex-based adverse events [3]. The latest update of DrugCentral introduced two age-based groups: FAERS data for pediatric patients (age ≤ 17 years) and geriatric patients (age ≥ 65 years) [4].
According to LRT statistics, 24.3% (81,654), 22.0% (44,375), and 10.8% (22,250) of drug-MedDRA term combinations show strong signals (LLR/LLRT > 5) in neutral, female, and male FAERS data, respectively. In pediatric and geriatric patients, 0.1% (2) and 22% show strong signals, respectively (Table 6). Very strong signals (LLR/LLRT > 10) are provided by 0.7–12.2% of the FAERS data within the sex-based partitioning. Pediatric data are poorly represented in FAERS, whereas 10.5% of the geriatric reports have very strong signals (Table 6).
Drug products and formulations
Pharmaceutical formulations and drug products marketed (or discontinued) in the US are extracted from DailyMed [48] and the FDA Orange Book [49]. DrugCentral contains a total of 142,303 products and formulations, with most administered orally (48.26%) and topically (39.96%), as shown in Fig. 6a. In terms of drugs (active substances), 1121 (43.4%) are formulated for oral administration, 733 (28.4%) for parenteral, and 354 (13.7%) for topical administration.
Regarding prescription types, 1761 (82.4%) drugs are found in human prescription (Rx) products, and only 375 drugs in over-the-counter (OTCs) products (Fig. 6b). However, the proportion of Rx and OTC products is relatively similar, 67,103 Rx versus 75,200 OTC products. Additionally, full-content drug labels extracted from DailyMed, are stored in DrugCentral and available for query in the text search functionality accessible from the web portal.
Other features
L1000 signature
Gene expression changes across multiple cell lines after exposure to drugs and small molecules provided by the LINCS program (Library of Integrated Cellular Signatures) [50, 51] have been integrated into DrugCentral. Gene expression changes induced across 81 cell lines were mapped to 1613 drugs resulting in 8,757,622 drug-cell line combinations made available in DrugCentral. Perturbational similarity across drugs was computed as Pearson correlation. The root mean square deviation (RMSD) and Pearson correlation between the perturbational profiles of the drugs across the cell lines were used to encode similarity. A search interface was developed in R-Shiny and added to DrugCentral to search and browse drugs with the most similar gene perturbation profiles. Correlation/distance profiles for any drug can be queried and downloaded.
REDIAL-2020
DrugCentral has implemented a web server to support efforts in finding suitable treatments for COVID-19 by quickly and efficiently estimating anti-SARS-CoV-2 activities from molecular structures [52]. The REDIAL-2020 server consists of six machine learning (ML) models representing various experimental assays related to viral entry (VE), viral replication (VR), and live virus infectivity (LVI), extracted from the NCATS (National Center for Advancing Translational Sciences) COVID19 portal (SARS-CoV-2 Assays—NCATS) [53, 54]. The models were built independently using fingerprint, pharmacophore, and physicochemical descriptors, supplied to 22 different ML algorithms from sci-kit-learn [55]. Consensus models were built using the top-ranking model for each descriptor type to maximize prediction performance. The REDIAL-2020 server (http://drugcentral.org/Redial) implements the most predictive models based on extensive performance validation.
Data access
The DrugCentral web interface (Fig. 7) is accessible at https://drugcentral.org/ from various devices, including desktops, laptops, phones, or tablets. The web search functionality supports multiple search types:
-
1.
Drug search: uses terms such as generic drug names, synonyms, brand names, and identifiers.
-
2.
Target search: supports terms like HUGO gene symbols, UniProt accessions, target names, and Swissprot identifiers.
-
3.
Disease search: can be performed using SNOMED-CT and OMOP vocabulary terms.
-
4.
Pharmacological action search: supports terms like MeSH, Mechanism of Action, physiologic effect (PE), FDA-established pharmacologic class (EPC), and ChEBI action roles [1, 2].
Query results are sorted using a 4-level ranking scheme based on:
-
A.
Drug name or synonyms, mechanism-of-action, and indication terms;
-
B.
Medical terms describing contraindications or off-label uses, targets (not MoA) in bioactivity data, and pharmacological actions;
-
C.
Drug description;
-
D.
FDA drug labels.
The ‘Drugs in the News’ and ‘Featured News’ sections are updated based on recent events [3].
In the DrugCentral web interface, direct access to the ‘Redial’ and ‘L1000 signature’ portals is available. As a result, users can estimate anti-SARS-CoV-2 activities of chemical structures based on the REDIAL-2020 models [3], and browse the distance/correlation matrices of the L1000 ConnectivityMap perturbation profiles [2]. By clicking the ‘About’ button on DrugCentral’s web page, users can access a summary of the database, including charts and functional tables that illustrate the current content of the database.
The full DrugCentral database is available for download in PostgreSQL format, enabling advanced data query, export, and integration. Users can load the full database dump file into a local PostgreSQL instance and perform advanced data manipulation using multiple structured query language (SQL) examples available in the download section of the DrugCentral website [1]. Several user-requested downloads are also made available, including chemical structures of the drugs in structure-data files (SDF), SMILES, and InChI formats, and drug bioactivity profiles in tabular format [2]. These resources allow users to access and work with DrugCentral data more flexibly and efficiently, depending on their specific needs and preferences.
Web-interface use case: warfarin
DrugCentral can be browsed online through the text search functionalities implemented in the web interface. As an example, let’s consider a drug search for warfarin.
Warfarin, a widely-used anticoagulant, is primarily prescribed to prevent blood clots from forming and growing in people with various conditions such as heart attack, certain types of irregular heartbeat, prosthetic heart valve implants, and to treat or prevent venous thrombosis and pulmonary embolism. Searching DrugCentral for the drug name lists warfarin first, followed by several pharmacologically similar anticoagulants based on the sorting criteria (see the above section for sorting criteria).
The drug card view for warfarin contains several tables with information about the drug class, dosage, pharmacokinetic properties, regulatory information, adverse events, pharmacologic actions, indications, bioactivity profile and MoA targets, external identifiers, and pharmaceutical formulations. Briefly, the description tab includes:
-
1.
The chemical structure of warfarin (downloadable in several formats).
-
2.
A list of synonyms.
-
3.
A short description extracted from the drug label.
-
4.
Calculated physicochemical properties.
-
5.
The drug’s status (Off Patent) shows that, while currently marketed, warfarin has expired composition-of-matter patents (see US patent US3077481A). This classification can help prioritize compounds in drug repositioning studies.
Nine pharmacokinetic parameters (manually curated from the scientific literature) are shown for Warfarin in the ADMET properties table. The Approvals table includes the first approval date of Warfarin (June 8, 1954) and other regulatory information. See Fig. 8.
DrugCentral provides information about FDA post-market adverse drug events for Warfarin, separated by sex (Fig. 9). Significant signals can be encountered for adverse effects with log-likelihood larger than the threshold values. For warfarin, gastrointestinal hemorrhage is frequently encountered in both men and women but has a significantly higher (almost double) occurrence in males (Fig. 9). Reports of a higher risk of gastrointestinal bleeding in men versus women under treatment with warfarin [56] confirm the results from DrugCentral. Such information can be used by healthcare professionals to assess the risks associated with Warfarin treatment and adjust the treatment plan accordingly for different patient populations [56].
The therapeutic uses of warfarin cover various sorts of venous thromboembolisms (embolisms due to prosthetic heart valves) and atrial fibrillation (Fig. 10). Off-label uses and contraindications are also provided in the Drug Use panel. Indications and contraindications for Warfarin are extracted from drug labels and linked to clinical terminology dictionaries, such as SNOMED-CT and Disease-Ontology. DrugCentral enables efficient information retrieval and seamless integration with other medical data sources by mapping these terms to standardized vocabularies. This information is crucial for healthcare providers to make informed decisions when prescribing Warfarin, as it provides an overview of the approved and non-approved treatment scenarios where the drug can be used or should be avoided.
The bioactivity profile of warfarin is captured in the Bioactivity summary panel (Fig. 10). The target names are provided with links to Pharos and Uniprot databases, offering users easy access to more in-depth information about the target proteins. A checkbox annotates Vitamin K epoxide reductase complex subunit 1 (VKORC1) as the MoA target for Warfarin, based on information from ChEMBL. By enabling such user-friendly access, DrugCentral provides a comprehensive overview of drug-protein interactions. Such information is essential for understanding the molecular basis of therapeutic and off-target effects, which can be relevant for drug repurposing efforts or developing new therapeutic agents with similar mechanisms of action.
Drug repurposing use-case: pharmacokinetics considerations
Drug repurposing projects aim to discover new therapeutic applications for existing drugs. Over the past few years, there has been a significant increase in drug repurposing studies [57, 58], which include various computational approaches [59, 60]. For example, docking and molecular dynamics (MD) studies of ~ 2000 drugs against the main protease (Mpro) of SARS-CoV-2 led to the identification of 5 drugs (manidipine, boceprevir, lercanidipine, bedaquiline, and efonidipine) with IC50 values between 4.8 and 38.5 μM [61]. Such concentrations are relatively high in comparison to the drug plasma concentration, e.g., oral administration of 10 mg lercanidipine results in a Cmax (the highest concentration in the blood) of 0.015 uM (~ 9.2 ng/mL) [62], raising concerns regarding the true repurposing potential of these drugs to treat COVID-19. Such studies have been criticized for not taking into account essential drug development factors, such as pharmacokinetics [57, 63]. In this use-case example, we will use the data available in DrugCentral to establish an activity threshold based on pharmacokinetic parameters, which can help guide drug repurposing efforts.
Out of 1156 drugs with defined MoA human targets and available activity values, 822 are categorized as OFP/OFM/ONP, as described in Table 7. The activity values for these targets (expressed as − log[ACT/M], further denoted as pACT) are the highest for ONP with a mean of 8.30 and decrease to 7.62 for OFP and to 7.42 for OFM drugs. This indicates that more recently approved drugs tend to have increased potency (Table 7). Moreover, ONP drugs tend to show different pharmacokinetic properties as encoded by the Biopharmaceutics Drug Disposition Classification System (BDDCS) parameter. BDDCS classifies drugs into four categories according to water solubility and extent of metabolism, EoM: Class 1—high solubility and high EoM; Class 2—low solubility and high EoM; Class 3—high solubility and low EoM; and Class 4—low solubility and low EoM, respectively [15, 64]. BDDCS properties are also driven by the subcellular localization of the biomolecular drug targets [65].
DrugCentral BDDCS annotations were updated with data from Bocci et al. [15], with 342 novel BDDCS-drug annotations and 82 updates. Out of a total of 1391 drugs with BDDCS, 715 have MoA targets. Of these, 81% are classified as BDDCS 1 and 2. OFP and OFM drugs are predominantly BDDCS 1 (45 and 52%, respectively), i.e., high solubility, whereas 56% of ONP drugs are BDDCS class 2, i.e., low solubility and extensive metabolism (Fig. 11). Since water solubility data is captured in DrugCentral we further investigated its influence on target bioactivity.
Most drugs (87%) show pACT > 6 on human MoA targets, a reasonable activity threshold (tpACT) a drug should exceed against a potential MoA target for drug repurposing. DrugCentral currently contains 1146 drugs with solubility information. Of these, 468 are drugs with MoA pACT > 6. For illustrative purposes, we examined only the lowest bioactivity value (the lowest MoA potency when multiple targets were annotated), and converted solubility values to logS. The Δ = log(S/ACT) computation shows the log difference between bioactivity and solubility. For 84% of the cases, Δ > 3. For any drug D we can define tpACT_sol_D = 3 − logSD. In other words, for a drug to be successfully repurposed, its activity against a novel (repurposed) target should be at least 3 − logS.
Poorly soluble drugs (lower logS) would require higher pACT values compared to highly soluble drugs with lower tpACT_D. This is consistent with our earlier observation that ONP drugs are, on average, more potent and less water-soluble than OFP and OFM drugs. Given the activity threshold introduced earlier (tpACT of 6), the “3 − logS” is more useful for drugs with logS < − 3. Thus, a novel drug-target activity could be considered “viable” for repurposing when tpACT = tpACT_sol if tpACT_sol > 6 and logS < − 3. We caution that this rule is derived from a limited dataset and ignores other factors critical for drug repurposing candidates [57, 63], and should be considered in the appropriate context. Further validation is required to confirm its applicability in drug repurposing.
Water solubility for warfarin is 0.02 mg/mL, i.e., logS of − 4.23 (logS < − 3), which results in a tpACT_sol of 7.23 (0.06 µM). This value can serve as a de minimis bioactivity (tpACT) guideline, should one consider warfarin as a repurposing candidate. BDDCS in general, and water solubility in particular, highlight the importance of considering pharmacokinetics information when repurposing drugs. The argument for prescribing warfarin for an unmet medical condition has to outweigh its potentially severe side effects given its on-target medical use (anticoagulant). Thus, scientists should consider the intended on-target effects and safety profile before proposing repurposing candidates.
Data availability
DrugCentral database is available at https://drugcentral.org/, free of charge, without registration.
Change history
02 December 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10822-023-00545-x
Abbreviations
- MoA:
-
Mechanism-of-action
- FDA:
-
U.S. food and drug administration
- EMA:
-
European medicines agency
- PMDA:
-
Japan pharmaceutical and medical devices agency
- ADMET:
-
Absorption, distribution, metabolism, excretion, and toxicity
- FAERS:
-
FDA’s adverse event reporting system
- MeSH:
-
Medical subject headings
- mAb:
-
Monoclonal antibodies
- GPCRs:
-
G-protein coupled receptors
References
Ursu O, Holmes J, Knockel J et al (2016) DrugCentral: online drug compendium. Nucleic Acids Res 45:D932–D939
Ursu O, Holmes J, Bologa CG et al (2019) DrugCentral 2018: an update. Nucleic Acids Res 47:D963–D970
Avram S, Bologa CG, Holmes J et al (2021) DrugCentral 2021 supports drug discovery and repositioning. Nucleic Acids Res 49:D1160–D1169
Avram S, Wilson TB, Curpan R et al (2023) DrugCentral 2023 extends human clinical data and integrates veterinary drugs. Nucleic Acids Res 51:D1276–D1287
FDA U.S. Food and Drug Administration. https://www.fda.gov/. Accessed 31 Dec 2022
EMA European Medicines Agency. In: European medicines agency. https://www.ema.europa.eu/en. Accessed 31 Dec 2022
Pharmaceuticals and Medical Devices Agency. https://www.pmda.go.jp/english/. Accessed 31 Dec 2022
World Health Organization—international nonproprietary names programme and classification of medical products. https://www.who.int/teams/health-product-and-policy-standards/inn/. Accessed 22 Nov2022
AMA Finder. https://searchusan.ama-assn.org/finder/usan/search/*/relevant/1/. Accessed 12 Jan 2023
Lipinski CA, Lombardo F, Dominy BW, Feeney PJ (1997) Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv Drug Deliv Rev 23:3–25
Oprea TI (2000) Property distribution of drug-related chemical databases. J Comput Aided Mol Des 14:251–264
Leo AJ (1993) Calculating log Poct from structures. Chem Rev 93:1281–1306
Ertl P, Rohde B, Selzer P (2000) Fast calculation of molecular polar surface area as a sum of fragment-based contributions and its application to the prediction of drug transport properties. J Med Chem 43:3714–3717
Milletti F, Storchi L, Goracci L et al (2010) Extending pKa prediction accuracy: high-throughput pKa measurements to understand pKa modulation of new chemical series. Eur J Med Chem 45:4270–4279
Bocci G, Oprea TI, Benet LZ (2022) State of the art and uses for the biopharmaceutics drug disposition classification system (BDDCS): new additions, revisions, and citation references. AAPS J 24:37
Hastings J, Owen G, Dekker A et al (2016) ChEBI in 2016: improved services and an expanding collection of metabolites. Nucleic Acids Res 44:D1214–D1219
Nelson SJ (2009) Medical terminologies that work: the example of MeSH. In: 2009 10th International symposium on pervasive systems, algorithms, and networks. pp 380–384
U.S Food & Drug Administration Pharmacologic Class. https://www.fda.gov/industry/structured-product-labeling-resources/pharmacologic-class. Accessed 11 Jan 2023
Avram S, Curpan R, Halip L et al (2020) Off-patent drug repositioning. J Chem Inf Model 60:5746–5753
Chemical Abstract Service (CAS). In: CAS. https://www.cas.org/cas-data. Accessed 11 Jan 2023
KEGG: Kyoto encyclopedia of genes and genomes. https://www.genome.jp/kegg/. Accessed 10 Jan 2023
Lin Y, Mehta S, Küçük-McGinty H et al (2017) Drug target ontology to classify and integrate drug discovery data. J Biomed Semant 8:50
Santos R, Ursu O, Gaulton A et al (2017) A comprehensive map of molecular drug targets. Nat Rev Drug Discov 16:19–34
Mendez D, Gaulton A, Bento AP et al (2019) ChEMBL: towards direct deposition of bioassay data. Nucleic Acids Res 47:D930–D940
Olah M, Rad R, Ostopovici L et al (2007) WOMBAT and WOMBAT-PK: bioactivity databases for lead and drug discovery. Chemical biology. Wiley, Hoboken, pp 760–786
Ganter B, Tugendreich S, Pearson CI et al (2005) Development of a large-scale chemogenomics database to improve drug candidate selection and to understand mechanisms of chemical toxicity and action. J Biotechnol 119:219–244
Armstrong JF, Faccenda E, Harding SD et al (2020) The IUPHAR/BPS guide to pharmacology in 2020: extending immunopharmacology content and introducing the IUPHAR/MMV guide to malaria pharmacology. Nucleic Acids Res 48:D1006–D1021
Roth BL, Lopez E, Patel S, Kroeze WK (2000) The multiplicity of serotonin receptors: uselessly diverse molecules or an embarrassment of riches? Neuroscientist 6:252–262
The UniProt Consortium, Bateman A, Martin M-J et al (2020) UniProt: the universal protein knowledgebase in 2021. Nucleic Acids Res 49:D480–D489
Knight ZA, Shokat KM (2005) Features of selective kinase inhibitors. Chem Biol 12:621–637
Avram S, Curpan R, Bora A et al (2018) Enhancing molecular promiscuity evaluation through assay profiles. Pharm Res 35:240
Ursu O, Glick M, Oprea T (2019) Novel drug targets in 2018. Nat Rev Drug Discov 18:328
Avram S, Halip L, Curpan R, Oprea TI (2020) Novel drug targets in 2019. Nat Rev Drug Discov 19:300
Avram S, Halip L, Curpan R, Oprea TI (2021) Novel drug targets in 2020. Nat Rev Drug Discov 20:333
Avram S, Halip L, Curpan R, Oprea TI (2022) Novel drug targets in 2021. Nat Rev Drug Discov 21:328
Avram S, Halip L, Curpan R, Oprea TI (2023) Novel drug targets in 2022. Nat Rev Drug Discov 22:437
Oprea TI, Bologa CG, Brunak S et al (2018) Unexplored therapeutic opportunities in the human genome. Nat Rev Drug Discov 17:317–332
Sheils TK, Mathias SL, Kelleher KJ et al (2021) TCRD and Pharos 2021: mining the human proteome for disease biology. Nucleic Acids Res 49:D1334–D1346
Sheils T, Mathias SL, Siramshetty VB et al (2020) How to illuminate the druggable genome using pharos. Curr Protoc Bioinform 69:e92
FDA Adverse Event Reporting System (FAERS). https://open.fda.gov/data/faers/. Accessed 22 Nov 2022
OHDSI—Observational health data sciences and informatics. https://www.ohdsi.org/. Accessed 15 Aug 2018
Donnelly K (2006) SNOMED-CT: the advanced terminology and coding system for eHealth. Stud Health Technol Inform 121:279–290
Bodenreider O (2004) The unified medical language system (UMLS): integrating biomedical terminology. Nucleic Acids Res 32:D267–D270
Disease Ontology—Institute for genome sciences @ University of Maryland. https://disease-ontology.org/. Accessed 12 Jan 2023
FDA’s Global Substance Registration System. https://precision.fda.gov/uniisearch. Accessed 22 Nov 2022
Medical Dictionary for Regulatory Activities (MedDRA). https://www.meddra.org/
Huang L, Zalkikar J, Tiwari RC (2011) A likelihood ratio test based method for signal detection with application to FDA’s drug safety data. J Am Stat Assoc 106:1230–1241
National Library of Medicine (NLM)’s DailyMed. https://dailymed.nlm.nih.gov/dailymed/. Accessed 23 Nov 2022
Orange Book: Approved drug products with therapeutic equivalence evaluations. Accessed 22 Nov 2022
National Institute of Health’s Library of Integrated Network-Based Cellular Signatures (LINCS) Program. https://lincsproject.org/
Subramanian A, Narayan R, Corsello SM et al (2017) A next generation connectivity map: L1000 platform and the first 1,000,000 profiles. Cell 171:1437-1452.e17
Kc GB, Bocci G, Verma S et al (2021) A machine learning platform to estimate anti-SARS-CoV-2 activities. Nat Mach Intell 3:527–535
National Center for Advancing Translational Sciences—OpenData portal: SARS-CoV-2 screening data. https://opendata.ncats.nih.gov/covid19/assays. Accessed 22 Nov 2022
Brimacombe KR, Zhao T, Eastman RT, et al. (2020) An OpenData portal to share COVID-19 drug repurposing data in real time. bioRxivorg. https://doi.org/10.1101/2020.06.04.135046
Pedregosa F, Varoquaux G, Gramfort A et al (2011) Scikit-learn: machine learning in python. J Mach Learn Res 12:2825–2830
Ingason AB, Hreinsson JP, Agustsson AS et al (2022) Warfarin is associated with higher rates of upper but not lower gastrointestinal bleeding compared to direct oral anticoagulants: a population-based propensity-weighted cohort study. Clin Gastroenterol Hepatol. https://doi.org/10.1016/j.cgh.2022.06.033
Sourimant J, Aggarwal M, Plemper RK (2021) Progress and pitfalls of a year of drug repurposing screens against COVID-19. Curr Opin Virol 49:183–193
Ghosh D, Sehgal K, Sodnar B et al (2022) Drug repurposing for stroke intervention. Drug Discov Today 27:1974–1982
Karaman B, Sippl W (2019) Computational drug repurposing: current trends. Curr Med Chem 26:5389–5409
Mullins JGL (2022) Drug repurposing in silico screening platforms. Biochem Soc Trans 50:747–758
Ghahremanpour MM, Tirado-Rives J, Deshmukh M et al (2020) Identification of 14 known drugs as inhibitors of the main protease of SARS-CoV-2. ACS Med Chem Lett 11:2526–2533
Chaudhary DV, Patel DP, Shah PA et al (2016) Determination of lercanidipine in human plasma by an improved UPLC-MS/MS method for a bioequivalence study. J Pharm Anal 6:87–94
Lewis RA (2021) Best practices for repurposing studies. J Comput Aided Mol Des 35:1189–1193
Wu C-Y, Benet LZ (2005) Predicting drug disposition via application of BCS: transport/absorption/elimination interplay and development of a biopharmaceutics drug disposition classification system. Pharm Res 22:11–23
Bocci G, Benet LZ, Oprea TI (2019) Can BDDCS illuminate targets in drug design? Drug Discov Today 24:2299–2306
Acknowledgements
We thank ChemAxon Ltd. for providing access to their software.
Funding
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number U24CA224370. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Conceptualization: TIO, SA; Formal analysis and investigation: LH, SA, RC, CB, AB, AB; Writing—original draft preparation: SA, LH, RC; Writing—review and editing: TIO; Funding acquisition: TIO; Supervision: TIO, CB. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
T.I.O. is a full-time employee of Expert Systems Inc. He was a full-time employee of AstraZeneca and Roivant Sciences. He served on the Scientific Advisory Board of ChemDiv Inc. and InSilico Medicine. The other authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Copyright was changed to Open Access.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Halip, L., Avram, S., Curpan, R. et al. Exploring DrugCentral: from molecular structures to clinical effects. J Comput Aided Mol Des 37, 681–694 (2023). https://doi.org/10.1007/s10822-023-00529-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10822-023-00529-x