Abstract
End-stage kidney disease and mild cognitive impairment (ESKD-MCI) affect the quality of life and long-term treatment outcomes of patients affected by these diseases. Clarifying the morphological changes from brain injuries in ESKD-MCI and their relationship with clinical features is helpful for the early identification and intervention of MCI before it progresses to irreversible dementia. This study gathered data from 23 patients with ESKD-MCI, 24 patients with ESKD and non-cognitive impairment (NCI), and 27 health controls (HCs). Structural magnetic resonance studies, cognitive assessments, and general clinical data were collected from all participants. Voxel-based morphometry analysis was performed to compare grey matter (GM) volume differences between the groups. The patients’ GM maps and clinical features were subjected to univariate regression to check for possible correlations. Patients with ESKD-MCI displayed significantly more impairments in multiple cognitive domains, including global cognition, visuospatial and executive function, and memory, compared to patients with ESKD-NCI. Using a more liberal threshold (P < 0.001, uncorrected), we found that compared to patients with ESKD-NCI, patients with ESKD-MCI exhibited clusters of regions with lower GM volumes, including the right hippocampus (HIP), parahippocampal gyrus (PHG), Rolandic operculum, and supramarginal gyrus. The volumes of the right HIP and PHG were negatively correlated with serum calcium levels. ESKD-MCI was associated with a subtle volume reduction of GM in several brain areas known to be involved in memory, language, and auditory information processing. We speculate that these slight morphometric impairments may be associated with disturbed calcium metabolism.
Similar content being viewed by others
Introduction
End-stage kidney disease (ESKD) is a progressive, incurable, and systemic disease (Collaboration et al., 2020). Although continuous advances in renal replacement therapy have effectively prolonged the survival of patients with ESKD, cognitive impairment (CI) is an important factor affecting the quality of life and prognosis of these patients (Kurella Tamura and Yaffe 2011). Mild cognitive impairment (MCI) can be identified in approximately 16–60% of patients with ESKD, which is two or three times higher than that in the age-matched general population (Viggiano et al. 2020a). Identifying MCI early, and exploring its underlying neuropathological mechanisms, may allow for early intervention, before irreversible damage occurs in patients with ESKD.
Recently, the role of imaging features and biological markers in the diagnosis of MCI has garnered increased interest (Albert et al. 2011). With the popularity and development of neuroimaging techniques, including magnetic resonance imaging (MRI) and positron emission tomography, patients with CI who may have been misdiagnosed or neglected can be diagnosed earlier and more accurately (Ellis et al. 2011). Structural MRI (sMRI) is inherently stable, radiation-free, non-invasive, and easy to perform. In the last decade, many studies have investigated macrostructural features of the brain in patients with ESKD using sMRI, with inconsistent results. However, a more consistent finding was that patients with ESKD had significantly abnormal grey matter (GM) volumes in areas associated with advanced cognitive functions, including attention and executive function (Qiu et al. 2014; Li et al. 2018; Wang et al. 2022), memory (Chiu et al. 2019; Gu et al. 2021; Jin et al. 2020; Li et al. 2018; Qiu et al. 2014; Wang et al. 2022), and auditory processing (Chai et al. 2015; Li et al. 2018; Wang et al. 2022) compared to healthy controls (HCs). The pattern of alterations in brain morphology in patients with ESKD and MCI remains unclear. Additionally, it should be noted that many of these studies included patients with ESKD who were on dialysis, whereas dialysis treatment itself had an impact on cognition, and did not stratify the degree of cognitive decline.
Among the various sMRI analysis techniques, voxel-based morphometry (VBM) has become popular because of its simplicity in operation and relatively stable and reliable results. VBM is an automated technique that calculates volume differences between groups by performing statistical tests for all voxels in the image. It can also be used to regress across voxels to assess the neuroanatomical correlates of cognitive deficits and clinical features (Whitwell 2009).
The purpose of the present study was to utilize VBM for comparing brain GM volumes among patients with ESKD and MCI, patients with ESKD and non-cognitive impairment (NCI) before the initiation of dialysis, as well as HCs. Additionally, we aimed to explore whether a relationship existed between morphological patterns and clinical features (cognitive function and biochemical blood indicators) in patients with ESKD and MCI.
Materials and methods
Participants and enrollment criteria
This study protocol was registered at ClinicalTrials.gov (NCT03961724, https://clinicaltrials.gov/ct2/show/NCT03961724) and received local ethics committee approval (XJTU1AF-CRF-2018-006). Figure 1 presents a flowchart depicting the selection criteria. Patients with ESKD who had never received dialysis were recruited from the Department of Nephrology at the local hospital. HCs with no history of neurologic, psychiatric, or other major medical illnesses were recruited by posting advertisements in the local community, and those with Montreal Cognitive Assessment (MoCA) scores < 26 were excluded.
The inclusion criteria for patients with ESKD were as follows: (1) aged 18–50 years; (2) estimated glomerular filtration rate (eGFR) < 15 mL/min/1.73m2; (3) not yet on dialysis or recipient of a kidney transplant. The exclusion criteria were as follows: (1) history of neurological or psychiatric disease, organic brain disease, or diabetes; (2) history of drug abuse or alcohol addiction; (3) macroscopic brain T2-visible lesions on MRI scans; (4) previously confirmed dementia, including Alzheimer’s disease (AD), frontotemporal dementia, or Parkinson’s disease dementia; (5) MoCA scores < 18; (6) contraindications to MRI examination; and (7) inability to cooperate with the completion of the MRI examination or cognitive function assessments.
Cognitive function assessments and biochemical blood tests
All subjects completed a series of standardized cognitive function assessments before undergoing the MRI scan. The Montreal Cognitive Assessment (MoCA) test, Beijing version, was used for assessing global cognitive function. It included visuospatial/executive function (5 points), naming (3 points), attention (6 points), language (3 points), abstraction (2 points), delayed recall(5 points) and orientation(6 points), with a total possible score of 30 points. If the education level was ≤ 12 years, 1 point was added to reduce educational bias (Nasreddine et al. 2005). The Auditory Verbal Learning Test, Huashan version (AVLT-H), was used for evaluating memory. It included an immediate recall total score (IR-S), short-term delayed recall score (SR-S), long-term delayed recall score (LR-S), and recognition score (REC-S) (Guo et al., 2009). The Trail Making Test part A (TMT-A) was used to evaluate processing speed (Bowie and Harvey 2006).
Biochemical blood tests were conducted for all patients with ESKD, including haemoglobin (g/L), haematocrit (%), blood urea nitrogen (BUN, mmol/L), serum creatinine (SCr, µmol/L), uric acid (µmol/L), cystatin C (CysC, mg/L), calcium (mmol/L), phosphorus (mmol/L), potassium (mmol/L), sodium (mmol/L), and parathyroid hormone (PTH, pg/mL), up to 24 h prior to the MRI scans.
Groups
Patients with ESKD who met the inclusion criteria were divided into two groups: patients with ESKD and MCI (ESKD-MCI), and those with ESKD and NCI (ESKD-NCI). The former was defined as ESKD patients who met the 2003 International Working Group criteria for a diagnosis of MCI (Winblad et al. 2004), while the latter were those with no evidence of CI. The MoCA was specifically designed to detect MCI, using a cut-off score point of 25/26, with a sensitivity of 80–100% and specificity of 50–76% (Nasreddine et al. 2005; Lin et al. 2013). Patients with MoCA scores ≥ 18 and < 26 were classified as ESKD-MCI, while those with scores ≥ 26 were classified as ESKD-NCI.
Image protocols
A 3 Tesla GE Excite MRI scanner (GE Medical Systems, Milwaukee, WI, USA) was employed to acquire images for all subjects. Structural image data for each participant were obtained using a T1-weighted three dimensional fast spoiled gradient echo sequence with the following parameters: 140 axial slices; slice thickness = 1.0 mm; echo time = 4.8 ms; repetition time = 10.8 ms; flip angle = 9°; no gap; matrix = 256 × 256; and field of view = 256 × 256 mm2.
Image data processing
Structural image data were processed using the Computational Anatomy Toolbox 12 software (CAT12, http://www.neuro.uni-jena.de/cat/), an extension of Statistical Parametric Mapping 12 (SPM12, http://www.fil.ion.ucl.ac.uk/spm/software/spm12/), in MATLAB 2021a (MathWorks Inc., Natick, USA). Initially, we checked the sample homogeneity in CAT12 to identify poor-quality images and incorrect pre-processing. No abnormalities were observed in the acquired or pre-processed images. Subsequently, each participant’s images were reoriented to share the same anterior commissure point of origin and spatial orientation. SPM12 tissue probability maps were used for the initial spatial registration and segmentation. GM, white matter (WM), and cerebrospinal fluid data were obtained using spatial segmentation to calculate the overall tissue volume and total intracranial volume (TIV). Next, the standard Montreal Neurological Institute (MNI) template in CAT12 was used to normalize the standard space, with the Diffeomorphic Anatomical Registration through the Exponentiated Lie algebra (DARTEL) toolbox used for GM and WM. After completion of the pre-processing steps, quality checks were performed using the CAT12 toolbox to assess the homogeneity of the GM tissues. Finally, the modulated and normalized GM tissue segments were smoothed with an 8-mm full width at half maximum Gaussian filter.
Statistical analysis
Intergroup differences in subjects’ demographics were analyzed using SPSS software (version 26.0; IBM Corp, Armonk, NY, USA). Additionally, differences in cognitive data between the groups were compared using one-way analysis of covariance (ANCOVA) adjusted for sex, age, and education level. A p-value < 0.05 indicated a significant difference. A statistical power analysis was performed on sample size.
Voxel-wise group comparisons (ESKD-MCI vs. HCs, ESKD-NCI vs. HCs, and ESKD-MCI vs. ESKD-NCI) of smoothed GM volumes were performed using two-sample t-tests within SPM 12, with age, sex, and TIV as covariates. Family-wise error (FWE) correction was applied for multiple comparison corrections with a threshold of p < 0.05. Meanwhile, an exploratory analysis was conducted using less conservative uncorrected thresholds of p < 0.001 for the entire brain.
Multiple univariate regression analyses were carried out using the SPM12 model design tool to access whether regional GM volume changes (ESKD-MCI vs. ESKD-NCI) were associated with clinical features (cognitive tests and biochemical blood indicators) in ESKD-MCI, with age, sex, education level, and TIV as covariates. These analyses were performed with a threshold of p < 0.001 and were uncorrected.
Results
Demographic data and clinical profiles
A total of 47 patients with ESKD, who had never received dialysis (23 ESKD-MCI, 24 ESKD-NCI) and 27 HCs were included in the present study. Intergroup differences in demographic data and clinical profiles are presented in Table 1. No significant differences were observed in pairwise comparisons among the three groups in terms of sex, age, or education level. Furthermore, no differences in the biochemical blood indicators were noted between the ESKD-MCI and ESKD-NCI groups. Group differences in cognitive function assessments, adjusted for age, sex, and education level, are detailed in Table 2 and illustrated in Fig. 2. Compared to HCs, the ESKD-MCI group showed poorer global cognitive function (p < 0.001, effect size = 3.64, two-sided α = 0.05, 1-β = 0.95, actual power = 100%), visuospatial/executive function, attention, memory, and processing speed, while compared to HCs, the ESKD-NCI group demonstrated poorer global cognitive function (p < 0.001, effect size = 1.07, two-sided α = 0.05, 1-β = 0.95, actual power = 96%), memory, and processing speed. When compared to the ESKD-NCI group, the ESKD-MCI group exhibited inferior global cognitive function (p < 0.001, effect size = 2.66, two-sided α = 0.05, 1-β = 0.95, actual power = 100%), visuospatial/executive function, and memory.
The violin plot depicts intergroup differences in cognitive function assessments between the patients with end-stage kidney disease and mild cognitive impairment (ESKD-MCI), those with ESKD and non-cognitive impairment (ESKD-NCI), and healthy controls (HCs), adjusted for age, sex, and education level
MoCA, Montreal Cognitive Assessment; V/E, visuospatial/executive; A, attention; DR, delayed recall; IR-S, immediate recall total score; SR-S, short-term delayed recall score; LR-S, long-term delayed recall score; REC-S, recognition score; TMT-A, trail-making test, part A. * p ≤ 0.05; ** p ≤ 0.01; *** p ≤ 0.001
Intergroup differences in GM volumes
Differences in GM volumes between the ESKD-MCI group and HCs are presented in Table 3 and illustrated in Fig. 3. Reduced GM volumes were observed in the right opercular part of the inferior frontal gyrus (IFGoperc), right triangular part of the IFG (IFGtriang), left orbital part of the superior frontal gyrus (ORBsup), left postcentral gyrus (PoCG), left precentral gyrus (PreCG), left superior temporal gyrus (STG), left middle temporal gyrus (MTG), right inferior temporal gyrus (ITG), right fusiform gyrus (FFG), left gyrus rectus (REC), right parahippocampal gyrus (PHG), right cerebellum_crus1 (CE_Crus1), right cerebellum_4_5 (CE_4_5), and right cerebellum_6 (CE_6) in the ESKD-MCI group, compared to HCs (p < 0.05 FWE-corrected). No significant increases in GM volumes were observed in the ESKD-MCI group compared to HCs.
Statistical parametric mapping regions superimposed on a high-resolution T1-weighted scan show decreased grey matter volumes in patients with end-stage kidney disease and mild cognitive impairment, compared to the healthy controls (p < 0.05, family-wise error-corrected)
R, right; L, left; IFGoperc, opercular part of inferior frontal gyrus; IFGtriang, triangular part of inferior frontal gyrus; PreCG, precentral gyrus; PoCG, postcentral gyrus; STG, superior temporal gyrus; MTG, middle temporal gyrus; PHG, parahippocampal gyrus; REC, gyrus rectus; FFG, fusiform gyrus; CE_Crus1, cerebellum_crus1; CE_4_5, cerebellum_4_5; CE_6, cerebellum_6; ORBsup, orbital part of superior frontal gyrus; ITG, inferior temporal gyrus
Differences in GM volumes between the ESKD-NCI group and HCs are shown in Table 4 and depicted in Fig. 4. Decreased GM volumes were observed in the left inferior parietal but supramarginal and angular gyri (IPL), left PoCG, left ORBsup, left temporal pole: MTG (TPOmid), right FFG, right ITG, right lingual gyrus (LING), right CE_Crus1, and right CE_6 in the ESKD-NCI group, compared to HCs (p < 0.05 FWE-corrected). No significant increases in GM volumes were found in the ESKD-NCI group compared to HCs.
Statistical parametric mapping regions superimposed on a high-resolution T1-weighted scan show decreased grey matter volumes in patients with end-stage kidney disease and non-cognitive impairment, compared to the healthy controls (p < 0.05, family-wise error-corrected)
R, right; L, left; IPL, inferior parietal but supramarginal and angular gyri; PoCG, postcentral gyrus, ORBsup, orbital part of superior frontal gyrus; FFG, fusiform gyrus; ITG, inferior temporal gyrus; LING, lingual gyrus; CE_6, cerebellum_6; CE_Crus1, cerebellum_crus1; TPOmid, temporal pole: middle temporal gyrus
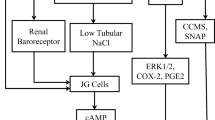
Differences in GM volumes between the ESKD-MCI and ESKD-NCI groups are displayed in Table 5 and visualized in Fig. 5. Decreased GM volumes were observed in the right hippocampus (HIP), right PHG, right rolandic operculum (ROL), and right supramarginal gyrus (SMG) in the ESKD-MCI group, compared to the ESKD-NCI group (p < 0.001 uncorrected). No significant increases in GM volumes were found in the ESKD-MCI group compared to the ESKD-NCI group.
Statistical parametric mapping regions superimposed on a high-resolution T1-weighted scan show decreased grey matter volumes in patients with end-stage kidney disease and mild cognitive impairment, compared to those with end-stage kidney disease and non-cognitive impairment (p < 0.001, uncorrected)
R, right; L, left; SMG, supramarginal gyrus; ROL, rolandic operculum; HIP, hippocampus; PHG, parahippocampal gyrus
Association of decreased GM volume with clinical features
Multiple univariate regression analyses demonstrated a negative correlation between the volumes of the right HIP and PHG and the serum calcium level in the ESKD-MCI group, utilizing uncorrected maps at p < 0.001 (Table 6). However, no correlation was observed between these brain regions and the cognitive scale tests or other biochemical blood indicators.
Discussion
The findings of the present study suggested that ESKD-MCI results in more impairments in multiple cognitive domains, including global cognition, visuospatial and executive function, and memory, when compared to ESKD-NCI. VBM analysis revealed that both the ESKD-MCI and ESKD-NCI groups presented with diffuse reductions in GM volumes compared to HCs. Notably, the extent of compromised GM was broader in the ESKD-MCI group compared to the ESKD-NCI group. The GM volumes of the right HIP, right PHG, right ROL, and right SMG were lower in the ESKD-MCI than the ESKD-NCI group, using a more liberal uncorrected statistical threshold. Moreover, in the ESKD-MCI group, the volumes of the right HIP and PHG were found to have a negatively correlation with serum calcium levels.
We observed that in comparison to HCs, patients with ESKD-MCI exhibited poorer performance across various cognitive domains, including global cognition, visuospatial and executive function, attention, memory, and processing speed. Compared to patients with ESKD-NCI, patients with ESKD-MCI performed poorly in global cognition, visuospatial and executive function, delayed recall, and immediate recall. These findings align with the hallmark features of MCI, characterized by subtle deficits in one or more crucial cognitive domains (Petersen 2011). While MCI does not interfere with patients’ activities of daily life, it may reduce adherence to complex regimens routinely prescribed to patients with ESKD, and influence the decision-making of ESKD treatment options (Kurella Tamura and Yaffe 2011). Consequently, it becomes imperative for clinicians to heighten their focus on screening for cognitive function among individuals with ESKD. Medical history and neuropsychological examinations are the primary tools used to diagnose MCI. Among the neuropsychological methods, the MoCA stands out as a specifically designed tool for MCI screening (Nasreddine et al. 2005). It is widely used in the auxiliary diagnosis of MCI-related disease entities such as AD-MCI (Julayanont et al. 2014), PD-MCI (Dalrymple-Alford et al. 2010), and hypertension-MCI (Mehra et al. 2020), due to its high sensitivity and superiority over the Mini-Mental State Examination (MMSE) (Pinto et al. 2019). A previous research had indicated that CI, including MCI and dementia, is prevalent among young (21–44 years, approximately 10%) and middle-aged (45–54 years, nearly 20%) hemodialysis patients with ESKD (Kurella Tamura and Yaffe 2011). To mitigate the potential influence of age and dialysis treatment on morphological brain changes, our study deliberately selected young and middle-aged patients with ESKD who had not undergone dialysis. Furthermore, delving into the neurobiological mechanisms underpinning the development of MCI in patients with ESKD would offer valuable insights.
We actually observed that patients with ESKD are not clinically screened for MCI among patients with ESKD, potentially attributed to the lack of effective interventions. A previous study’s findings underscored the significant role played by ESKD-related vascular factors and uraemic neurotoxins in CI (Viggiano et al. 2020b). Although there are no effective drugs for treating MCI, vascular risk factors control and physical and mental activities present promising avenues for patients with ESKD. These strategies can enhance the well-being of patients and caregivers and reduce the risk of poor outcomes (Kurella Tamura and Yaffe 2011; Langa and Levine 2014). Furthermore, our study’s results indicated that patients categorized as having with ESKD-NCI were considered to lack cognitive decline, still differed from HCs in global cognition, memory, and processing speed. These results indicate that patients with ESKD who rely on clinical symptoms and cognitive scales to be divided into groups without CI still may have mild cognitive decline and should be closely monitored.
The VBM analysis revealed that in comparison to HCs, both the ESKD-MCI and ESKD-NCI groups presented a reduction in diffuse GM volumes. As expected, the ESKD-MCI group had a greater extent of brain damage than the ESKD-NCI group. Specifically, the ESKD-MCI group displayed lower GM volume in the right IFG, left ORBsup, left PreCG, left PoCG, left STG, left MTG, left ROL, right ITG, right FFG, left REC, right PHG, and certain right cerebellar regions. These brain regions are implicated in various aspects of cognitive function. For instance, the FFG is primarily responsible for advanced visual functions like face perception and object recognition (Rapcsak 2019). The REC, also called the straight gyrus, situated at the base of the prefrontal cortex, and although its specific function has not yet been elucidated, it may be involved in higher cognitive functioning (e.g., personality) (Selden et al. 1998). The cerebellum plays a role in cognitive and emotional functions, with right-lateralised observed for language and left-lateralised for spatial functions (Schmahmann 2019). Neurodegeneration and direct neuronal injury caused by shared risk factors for the brain and kidney, nephrogenic risk factors, and ESKD treatment-associated risk factors are the primary pathophysiological mechanisms of CI in patients with ESKD (Kurella Tamura and Yaffe 2011). The findings of our study indicate that patients with ESKD-MCI exhibit diffuse structural brain damage that may underlie impairments in multiple cognitive domains.
Previous studies have shown extensive changes in GM volumes alterations among patients with ESKD (Qiu et al. 2014; Li et al. 2018; Wang et al. 2022; Chiu et al. 2019; Gu et al. 2021; Chai et al. 2015), although the results of these studies may vary depending on the sample selection and analytical methodologies. Few studies, however, have stratified the degree of CI among patients with ESKD. Zhang et al. divided patients with ESKD receiving dialysis into minimal nephro-encephalopathy (MNE) and non-nephro-encephalopathy groups, based on their clinical symptoms and attention function (Zhang et al. 2013). This study showed GM volume reduction in the right middle frontal gyrus, right PoCG, right occipital lobe, and left insula in ESRD patients with MNE. These patients receiving dialysis and different evaluation criteria for CI may be the reasons that the results differed from our findings. Recently, a study using diffusion kurtosis imaging found that disrupted brain micro-structures in patients with ESKD-MCI (Zheng et al. 2022). However, this result was based on comparisons between ESKD-MCI and HCs. In the context of our study, it is noteworthy that the observed subtle decrease in GM volume in the right HIP, right PHG, right SMG, and right ROL may signify brain regions in susceptible to damage in patients with ESKD-MCI, in contrast to patients with ESKD-NCI. It is well known that the HIP plays a critical role in episodic memory and navigation (Lisman et al. 2017), and the right HIP is more involved in the memory of locations within the environment (Burgess et al. 2002). An animal study using adult male Sprague − Dawley rats indicated that ESKD can induce cell death in HIP CA1 (Kim et al. 2014). Adjacent to the hippocampus, the PHG is a part of the limbic system. This region plays an important role in memory encoding and retrieval, scene recognition, and social context identification (Squire et al. 2004). The SMG within the inferior parietal lobule plays a role in visual word recognition (Stoeckel et al. 2009). One study showed that the right SMG may also be associated with the maintenance of the ability to recognize emotion (Wada et al. 2021). Therefore, specific damaged regions of the brain in patients with ESKD-MCI may be involved in memory, spatial localisation, visual word recognition, and auditory information processing, which is consistent with the cognitive test results in the present study. The results suggested imaging markers may be provide a relatively objective entry point for the diagnosis of MCI in ESKD patients. Unfortunately, we did not find a direct correlation between these abnormal brain regions and the cognitive scales, possibly due to the small sample size in our study. This underscores the need for larger-scale investigations to unveil potential relationships between structural brain changes and cognitive performance in the context of ESKD-MCI.
Initially, our study did not find significant correlations between the different regions of the brain and clinical measures (p < 0.05, FWE-corrected). However, using a more liberal uncorrected threshold (p < 0.001), we observed the right HIP and PHG volumes were negatively correlated with serum calcium levels in the ESKD-MCI group. Serum calcium plays critical physiological and biochemical roles in the human body, including neurotransmitter release, signal transduction, muscle contraction, and the electrophysiological stabilisation of cell membranes (Obi et al. 2018), and calcium homeostasis in the human body plays a critical role in many underlying neurological dysfunctions in chronic brain diseases during the aging process (Khachaturian 1994). Excessive calcium entry into the cell leads to an intracellular calcium overload and nerve death. Disturbances in calcium metabolism in patients with ESKD can lead to impaired neuronal Ca2+ handling, which in turn causes a series of downstream outcomes, such as synapse loss, amyloid β-peptide accumulation, mitochondrial dysfunction, oxidative stress, and inflammation (Alzheimer's Association Calcium Hypothesis Workgroup 2017), ultimately leading to CI. One study showed that calcium channel blockers have therapeutic effects on CI, due to a variety of causes (López-Arrieta and Birks 2000). These mechanisms include the inhibition of Ca2+ overload in neural cells and the blocking of the common channel of neural cell death. The authors hypothesized that the correlation between the decrease in HIP/PHG volumes and increased serum calcium in patients with ESKD-MCI may be due to increased intracellular calcium influx, leading to neuronal death in the HIP/PHG. The findings underscored the significance of maintaining calcium homeostasis as a critical factor in the prevention of CI among patients with ESKD. This insight not only highlights the potential contribution of calcium dysregulation to cognitive decline but also underscores the importance of investigating and optimizing calcium-related interventions to improve CI in this population.
Limitations
The present study has several limitations. Firstly, it was a cross-sectional study with a small sample size. Sample size expansion and further longitudinal studies are needed to evaluate the changes in brain morphology and CI in patients with ESKD. Additionally, animal studies may better explore the molecular mechanisms of GM volume changes and elucidate their causal relationships. Moreover, the diagnosis of MCI in patients with ESKD requires more comprehensive diagnostic criteria. Therefore, objective and stable imaging diagnostic markers need to be explored further. Incorporating such markers might improve the precision of identifying CI and tracking their progression.
Conclusion
In summary, the results of the present study indicated that ESKD-MCI was associated with subtle GM volume reductions in several areas of the brain known to be involved in memory, language, and auditory information processing. Notably, serum calcium levels appear to play a role in influencing these subtle morphological alterations. Importantly, even individuals diagnosed with ESKD-NCI, relying on clinical symptoms and cognitive assessments, still shows some cognitive domains impairments. More sensitive imaging methods are needed to explore key brain regions injuries in patients with ESKD-MCI.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
References
Albert MS, DeKosky ST, Dickson D et al (2011) The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):270–279. https://doi.org/10.1016/j.jalz.2011.03.008
Alzheimer’s Association Calcium Hypothesis Workgroup (2017) Calcium hypothesis of Alzheimer’s disease and brain aging: a framework for integrating new evidence into a comprehensive theory of pathogenesis. Alzheimers Dement 13(2):178–182e17. https://doi.org/10.1016/j.jalz.2016.12.006
Bowie CR, Harvey PD (2006) Administration and interpretation of the trail making test. Nat Protoc 1(5):2277–2281. https://doi.org/10.1038/nprot.2006.390
Burgess N, Maguire EA, O’Keefe J (2002) The human hippocampus and spatial and episodic memory. Neuron 35(4):625–641. https://doi.org/10.1016/s0896-6273(02)00830-9
Chai C, Zhang M, Long M et al (2015) Increased brain iron deposition is a risk factor for brain atrophy in patients with haemodialysis: a combined study of quantitative susceptibility mapping and whole brain volume analysis. Metab Brain Dis 30(4):1009–1016. https://doi.org/10.1007/s11011-015-9664-2
Chiu YL, Tsai HH, Lai YJ et al (2019) Cognitive impairment in patients with end-stage renal disease: accelerated brain aging? J Formos Med Assoc 118(5):867–875. https://doi.org/10.1016/j.jfma.2019.01.011
Dalrymple-Alford JC, MacAskill MR, Nakas CT et al (2010) The MoCA: well-suited screen for cognitive impairment in Parkinson disease. Neurology 75(19):1717–1725. https://doi.org/10.1212/WNL.0b013e3181fc29c9
Ellis KA, Rowe CC, Szoeke CE et al (2011) Advances in structural and molecular neuroimaging in Alzheimer’s disease. Med J Aust 194(4):S20–S23. https://doi.org/10.5694/j.1326-5377.2011.tb02938.x
GBD Chronic Kidney Disease Collaboration (2020) Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet (London England) 395(10225):709–733. https://doi.org/10.1016/S0140-6736(20)30045-3
Gu W, He R, Su H et al (2021) Changes in the shape and volume of subcortical structures in patients with end-stage renal disease. Front Hum Neurosci 15:778807. https://doi.org/10.3389/fnhum.2021.778807
Guo Q, Zhao Q, Chen M et al (2009) A comparison study of mild cognitive impairment with 3 memory tests among chinese individuals. Alzheimer Dis Assoc Disord 23(3):253–259. https://doi.org/10.1097/WAD.0b013e3181999e92
Jin M, Wang L, Wang H et al (2020) Structural and functional alterations in Hemodialysis Patients: a voxel-based morphometry and functional connectivity study. Front Hum Neurosci 14:80. https://doi.org/10.3389/fnhum.2020.00080
Julayanont P, Brousseau M, Chertkow H et al (2014) Montreal Cognitive Assessment Memory Index score (MoCA-MIS) as a predictor of conversion from mild cognitive impairment to Alzheimer’s disease. J Am Geriatr Soc 62(4):679–684. https://doi.org/10.1111/jgs.12742
Khachaturian ZS (1994) Calcium hypothesis of Alzheimer’s disease and brain aging. Ann N Y Acad Sci 747:1–11. https://doi.org/10.1111/j.1749-6632.1994.tb44398
Kim JW, Ha GY, Jung YW (2014) Chronic renal failure induces cell death in rat hippocampal CA1 via upregulation of αCaMKII/NR2A synaptic complex and phosphorylated GluR1-containing AMPA receptor cascades. Kidney Res Clin Pract 33(3):132–138. https://doi.org/10.1016/j.krcp.2014.07.003
Kurella Tamura M, Yaffe K (2011) Dementia and cognitive impairment in ESRD: diagnostic and therapeutic strategies. Kidney Int 79(1):14–22. https://doi.org/10.1038/ki.2010.336
Langa KM, Levine DA (2014) The diagnosis and management of mild cognitive impairment: a clinical review. JAMA 312(23):2551–2561. https://doi.org/10.1001/jama.2014.13806
Li A, Mu J, Huang M et al (2018) Altered amygdala-related structural covariance and resting-state functional connectivity in end-stage renal disease patients. Metab Brain Dis 33(5):1471–1481. https://doi.org/10.1007/s11011-018-0254-y
Lin JS, O’Connor E, Rossom RC et al (2013) Screening for cognitive impairment in older adults: an evidence update for the U.S. Preventive Services Task Force. Agency for Healthcare Research and Quality (US)
Lisman J, Buzsáki G, Eichenbaum H et al (2017) Viewpoints: how the hippocampus contributes to memory, navigation and cognition. Nat Neurosci 20(11):1434–1447. https://doi.org/10.1038/nn.4661
López-Arrieta JM, Birks J (2000) Nimodipine for primary degenerative, mixed and vascular dementia. Cochrane Database Syst Rev 2CD000147. https://doi.org/10.1002/14651858.CD000147
Mehra A, Suri V, Kumari S et al (2020) Association of mild cognitive impairment and metabolic syndrome in patients with hypertension. Asian J Psychiatr 53:102185. https://doi.org/10.1016/j.ajp.2020.102185
Nasreddine ZS, Phillips NA, Bédirian V et al (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr So 53(4):695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x
Obi Y, Park C, Soohoo M et al (2018) Association of Pre-ESRD serum calcium with Post-ESRD mortality among Incident ESRD Patients: a Cohort Study. J Bone Miner Res 33(6):1027–1036. https://doi.org/10.1002/jbmr.3391
Petersen RC (2011) Clinical practice. Mild cognitive impairment. N Engl J Med 364(23):2227–2234. https://doi.org/10.1056/NEJMcp0910237
Pinto TCC, Machado L, Bulgacov TM et al (2019) Is the Montreal Cognitive Assessment (MoCA) screening superior to the Mini-Mental State Examination (MMSE) in the detection of mild cognitive impairment (MCI) and Alzheimer’s Disease (AD) in the elderly? Int Psychogeriatr 31(4):491–504. https://doi.org/10.1017/S1041610218001370
Qiu Y, Lv X, Su H et al (2014) Structural and functional brain alterations in end stage renal disease patients on routine hemodialysis: a voxel-based morphometry and resting state functional connectivity study. PLoS ONE 9(5):e98346. https://doi.org/10.1371/journal.pone.0098346
Rapcsak SZ (2019) Face Recognition. Curr Neurol Neurosci Rep 19(7):41. https://doi.org/10.1007/s11910-019-0960-9
Schmahmann JD (2019) The cerebellum and cognition. Neurosci Lett 688:62–75. https://doi.org/10.1016/j.neulet.2018.07.005
Selden NR, Gitelman DR, Salamon-Murayama N et al (1998) Trajectories of cholinergic pathways within the cerebral hemispheres of the human brain. Brain 121(Pt 12):2249–2257. https://doi.org/10.1093/brain/121.12.2249
Squire LR, Stark CE, Clark RE (2004) The medial temporal lobe. Annu Rev Neurosci 27:279–306. https://doi.org/10.1146/annurev.neuro.27.070203.144130
Stoeckel C, Gough PM, Watkins KE et al (2009) Supramarginal gyrus involvement in visual word recognition. Cortex 45(9):1091–1096. https://doi.org/10.1016/j.cortex.2008.12.004
Viggiano D, Wagner CA, Martino G et al (2020) Mechanisms of cognitive dysfunction in CKD. Nat Rev Nephrol 16(8):452–469. https://doi.org/10.1038/s41581-020-0266-9
Viggiano D, Wagner CA, Blankestijn PJ et al (2020a) Mild cognitive impairment and kidney disease: clinical aspects. Nephrol Dial Transplant 35(1):10–17. https://doi.org/10.1093/ndt/gfz051
Wada S, Honma M, Masaoka Y et al (2021) Volume of the right supramarginal gyrus is associated with a maintenance of emotion recognition ability. PLoS ONE 16(7):e0254623. https://doi.org/10.1371/journal.pone.0254623
Wang H, Huang L, Wu G et al (2022) Regional cerebral gray matter atrophy is associated with cognitive impairment in hemodialysis patients: a cross-sectional and longitudinal voxel-based morphological MRI study. Brain Imaging Behav 16(3):1284–1293. https://doi.org/10.1007/s11682-021-00602-9
Whitwell JL (2009) Voxel-based morphometry: an automated technique for assessing structural changes in the brain. J Neurosci 29(31):9661–9664. https://doi.org/10.1523/JNEUROSCI.2160-09.2009
Winblad B, Palmer K, Kivipelto M et al (2004) Mild cognitive impairment–beyond controversies, towards a consensus: report of the International Working Group on mild cognitive impairment. J Intern Med 256(3):240–246. https://doi.org/10.1111/j.1365-2796.2004.01380.x
Zhang LJ, Wen J, Ni L et al (2013) Predominant gray matter volume loss in patients with end-stage renal disease: a voxel-based morphometry study. Metab Brain Dis 28(4):647–654. https://doi.org/10.1007/s11011-013-9438-7
Zheng J, Jiao Z, Dai J et al (2022) Abnormal cerebral micro-structures in end-stage renal disease patients related to mild cognitive impairment. Eur J Radiol 157:110597. https://doi.org/10.1016/j.ejrad.2022.110597
Acknowledgements
We thank the all participants and staff involved in this study.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 82071879) and the Natural Science Basis Research Plan in Shaanxi Province of China (No. 2023-JC-QN-0984).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by Huijie Yuan, Zhaoyao Luo, Junya Mu, and Ming Zhang. Analysis was performed by Huijie Yuan, Zhaoyao Luo, Wen Gu, Shaohui Ma, and Guangyu Li. Data collection was performed by Dun Ding, Xueying Ma, Peng Li, Jing Yang, and Xiaoling Xu. The first draft of the manuscript was written by Huijie Yuan and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by ethics committee of the First Affiliated Hospital of Xi’an Jiaotong University (ID: XJTU1AF2018LSL-006).
Consent to participate
Written informed consent was obtained in accordance with the Declaration of Helsinki (1964) from each patient or their guardians.
Consent for publication
Not applicable.
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yuan, H., Luo, Z., Gu, W. et al. Abnormal grey matter structural changes in patients with end-stage kidney disease and mild cognitive impairment: correlations with clinical features. Metab Brain Dis 38, 2817–2829 (2023). https://doi.org/10.1007/s11011-023-01293-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-023-01293-5