Abstract
Background
A significant proportion of adults with major depressive disorder (MDD) do not respond to treatments which are currently used in clinical practice such as first-generation monoamine-based antidepressants.
Objectives
The objective of this systematic review was to assess the efficacy, safety, and mechanisms of action of AXS-05, a combination of the NMDA-receptor antagonist dextromethorphan with bupropion, in adults with MDD.
Methods
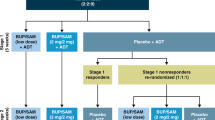
We searched PubMed, Embase, Google Scholar, and ClinicalTrials.gov for current studies reporting on efficacy and/or safety of AXS-05 in patients with MDD. The search terms included: “AXS-05” OR “dextromethorphan and bupropion” AND “depression”. Studies from database inception to January 2023 were evaluated. Risk of bias was assessed using the Cochrane Risk of Bias tool.
Results
The search yielded 54 studies of which 5 were included. All studies had low risk of bias. Depression severity, measured with the Montgomery–Åsberg Depression Rating Scale (MADRS) significantly decreased as early as 1-week post-treatment from baseline when compared to a placebo-controlled group (LS mean difference 2.2; 95% CI 0.6–3.9; p = 0.007) and at 2 weeks compared to an active control group (LS mean difference 4.7; 95% CI 0.6–8.8; p = 0.024). Treatment efficacy could be maintained for up to 12 months with mean MADRS score reduction of 23 points from baseline. Clinical remission and response rates also improved at week 1 and were maintained for 12 months. The treatment was well-tolerated, with some transient adverse events reported.
Conclusion
Current evidence suggests that the combination of dextromethorphan and bupropion is a well-tolerated, rapid-acting treatment option for adults with MDD. Initial success with AXS-05 supports the mechanistic role of glutamatergeric and sigma 1 signaling in the pathophysiology of MDD.


Similar content being viewed by others
References
Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317:1517. https://doi.org/10.1001/jama.2017.3826.
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858. https://doi.org/10.1016/S0140-6736(18)32279-7.
Lam RW, McIntosh D, Wang J, Enns MW, Kolivakis T, Michalak EE, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 1. Disease Burden and Principles of Care. Can J Psychiatry. 2016;61:510–23. https://doi.org/10.1177/0706743716659416.
Maj M, Stein DJ, Parker G, Zimmerman M, Fava GA, De Hert M, et al. The clinical characterization of the adult patient with depression aimed at personalization of management. World Psychiatry. 2020;19:269–93. https://doi.org/10.1002/wps.20771.
Rhee TG, Steffens DC. Major depressive disorder and impaired health-related quality of life among US older adults. Int J Geriatr Psychiatry. 2020;35:1189–97. https://doi.org/10.1002/gps.5356.
McIntyre RS, Millson B, Power GS. Burden of Treatment Resistant Depression (TRD) in patients with major depressive disorder in Ontario using Institute for Clinical Evaluative Sciences (ICES) databases: economic burden and healthcare resource utilization. J Affect Disord. 2020;277:30–8. https://doi.org/10.1016/j.jad.2020.07.045.
Berton O, Nestler EJ. New approaches to antidepressant drug discovery: beyond monoamines. Nat Rev Neurosci. 2006;7:137–51. https://doi.org/10.1038/nrn1846.
Hermida AP, Glass OM, Shafi H, McDonald WM. Electroconvulsive therapy in depression: current practice and future direction. Psychiatr Clin North Am. 2018;41:341–53. https://doi.org/10.1016/j.psc.2018.04.001.
Rhee TG, Shim SR, Forester BP, Nierenberg AA, McIntyre RS, Papakostas GI, et al. Efficacy and safety of ketamine vs electroconvulsive therapy among patients with major depressive episode: a systematic review and meta-analysis. JAMA Psychiat. 2022;79:1162–72. https://doi.org/10.1001/jamapsychiatry.2022.3352.
McIntyre RS, Filteau M-J, Martin L, Patry S, Carvalho A, Cha DS, et al. Treatment-resistant depression: definitions, review of the evidence, and algorithmic approach. J Affect Disord. 2014;156:1–7. https://doi.org/10.1016/j.jad.2013.10.043.
Zhdanava M, Pilon D, Ghelerter I, Chow W, Joshi K, Lefebvre P, et al. The prevalence and national burden of treatment-resistant depression and major depressive disorder in the United States. J Clin Psychiatry. 2021;82:20m13699. https://doi.org/10.4088/JCP.20m13699.
Jaffe DH, Rive B, Denee TR. The humanistic and economic burden of treatment-resistant depression in Europe: a cross-sectional study. BMC Psychiatry. 2019;19:247. https://doi.org/10.1186/s12888-019-2222-4.
Diazgranados N, Ibrahim L, Brutsche NE, Newberg A, Kronstein P, Khalife S, et al. A randomized add-on trial of an N-methyl-D-aspartate antagonist in treatment-resistant bipolar depression. Arch Gen Psychiatry. 2010;67:793–802. https://doi.org/10.1001/archgenpsychiatry.2010.90.
Hofmann SG, Curtiss J, Carpenter JK, Kind S. Effect of treatments for depression on quality of life: a meta-analysis. Cogn Behav Ther. 2017;46:265–86. https://doi.org/10.1080/16506073.2017.1304445.
McIntyre RS, Cha DS, Soczynska JK, Woldeyohannes HO, Gallaugher LA, Kudlow P, et al. Cognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatment interventions. Depress Anxiety. 2013;30:515–27. https://doi.org/10.1002/da.22063.
Alnefeesi Y, Chen-Li D, Krane E, Jawad MY, Rodrigues NB, Ceban F, et al. Real-world effectiveness of ketamine in treatment-resistant depression: a systematic review and meta-analysis. J Psychiatr Res. 2022;151:693–709. https://doi.org/10.1016/j.jpsychires.2022.04.037.
Marcantoni WS, Akoumba BS, Wassef M, Mayrand J, Lai H, Richard-Devantoy S, et al. A systematic review and meta-analysis of the efficacy of intravenous ketamine infusion for treatment resistant depression: January 2009–January 2019. J Affect Disord. 2020;277:831–41. https://doi.org/10.1016/j.jad.2020.09.007.
McIntyre RS, Rosenblat JD, Nemeroff CB, Sanacora G, Murrough JW, Berk M, et al. Synthesizing the evidence for ketamine and esketamine in treatment-resistant depression: an international expert opinion on the available evidence and implementation. Am J Psychiatry. 2021;178:383–99. https://doi.org/10.1176/appi.ajp.2020.20081251.
Yavi M, Lee H, Henter ID, Park LT, Zarate CA. Ketamine treatment for depression: a review. Discov Ment Health. 2022;2:9. https://doi.org/10.1007/s44192-022-00012-3.
Majeed A, Xiong J, Teopiz KM, Ng J, Ho R, Rosenblat JD, et al. Efficacy of dextromethorphan for the treatment of depression: a systematic review of preclinical and clinical trials. Expert Opin Emerg Drugs. 2021;26:63–74. https://doi.org/10.1080/14728214.2021.1898588.
Nguyen L, Thomas KL, Lucke-Wold BP, Cavendish JZ, Crowe MS, Matsumoto RR. Dextromethorphan: an update on its utility for neurological and neuropsychiatric disorders. Pharmacol Ther. 2016;159:1–22. https://doi.org/10.1016/j.pharmthera.2016.01.016.
Hole K, Arnestad M, Molden E, Haslemo T. Dose-dependent inhibition of cYP2D6 by bupropion in patients with depression. J Clin Psychopharmacol. 2021;41:281–5. https://doi.org/10.1097/JCP.0000000000001387.
O’Gorman C, Jones A, Tabuteau H. AXS-05 (Dextromethorphan/Bupropion): psychopharmacology and the potential for therapeutic application in the treatment of neuropsychiatric symptoms. Eur Neuropsychopharmacol. 2019;29:S458. https://doi.org/10.1016/j.euroneuro.2018.11.686.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Tabuteau H, Jones A, Anderson A, Jacobson M, Iosifescu DV. Effect of AXS-05 (Dextromethorphan-Bupropion) in major depressive disorder: a randomized double-blind controlled trial. Am J Psychiatry. 2022;179:490–9. https://doi.org/10.1176/appi.ajp.21080800.
Iosifescu DV, Jones A, O’Gorman C, Streicher C, Feliz S, Fava M, et al. Efficacy and safety of AXS-05 (Dextromethorphan-Bupropion) in patients with major depressive disorder: a phase 3 randomized clinical trial (GEMINI). J Clin Psychiatry. 2022;83:21m14345. https://doi.org/10.4088/JCP.21m14345.
Jones A, O'Gorman C, Clayton AH, Tabuteau H. Analysis of Efficacy of AXS-05 in the Treatment of Major Depressive Disorder Based on Gender, Race, and Prior Antidepressant Use [Poster Presentation]. ISCTM Annual Meeting, New York, NY, USA; April 6-9 2021. https://isctm.org/public_access/17th_Annual/Poster/Jones_poster.pdf.
O'Gorman C, Jones A, Kennon K, Niecestro R, Iosifescu DV, Stahl S, et al. AXS-05 for Neuropsychiatric Disorders: Scientific Rationale and Clinical Development [Poster Presentation]. ASCP Annual Meeting, Miami Beach, FL, USA. May 29-June 1 2018. https://d3dyybxyjb4kyh.cloudfront.net/pdfs/Axsome_AXS_05_Poster_ASCP_5_2018.pdf.
O'Gorman C, Jones A, Tabuteau H. Sustained Efficacy with Long-term Treatment if AXS-05: Results from the COMET Phase 3 Trial, a Long-term, Open-label Study Evaluating the Efficacy and Safety of AXS-05 for the Treatment of MDD [Poster Presentation]. American Society of Clinical Psychopharmacology, Annual Meeting, New York, NY, USA. June 1-4 2021. https://d3dyybxyjb4kyh.cloudfront.net/pdfs/ASCP+2021+COMET+overall+poster+FINAL.pdf
Matveychuk D, Thomas RK, Swainson J, Khullar A, MacKay M-A, Baker GB, et al. Ketamine as an antidepressant: overview of its mechanisms of action and potential predictive biomarkers. Ther Adv Psychopharmacol. 2020;10:2045125320916657. https://doi.org/10.1177/2045125320916657.
Rodrigues NB, McIntyre RS, Lipsitz O, Cha DS, Lee Y, Gill H, et al. Changes in symptoms of anhedonia in adults with major depressive or bipolar disorder receiving IV ketamine: results from the Canadian Rapid Treatment Center of Excellence. J Affect Disord. 2020;276:570–5. https://doi.org/10.1016/j.jad.2020.07.083.
Siu A, Drachtman R. Dextromethorphan: a review of N-methyl-d-aspartate receptor antagonist in the management of pain. CNS Drug Rev. 2007;13:96–106. https://doi.org/10.1111/j.1527-3458.2007.00006.x.
Zanger UM, Raimundo S, Eichelbaum M. Cytochrome P450 2D6: overview and update on pharmacology, genetics, biochemistry. Naunyn Schmiedebergs Arch Pharmacol. 2004;369:23–37. https://doi.org/10.1007/s00210-003-0832-2.
Xue C, Zhang X, Cai W. Prediction of drug–drug interactions with bupropion and its metabolites as CYP2D6 inhibitors using a physiologically-based pharmacokinetic model. Pharmaceutics. 2017;10:1. https://doi.org/10.3390/pharmaceutics10010001.
Garnock-Jones KP. Dextromethorphan/quinidine: in pseudobulbar affect. CNS Drugs. 2011;25:435–45. https://doi.org/10.1016/j.jad.2020.07.083.
Taylor CP, Traynelis SF, Siffert J, Pope LE, Matsumoto RR. Pharmacology of dextromethorphan: relevance to dextromethorphan/quinidine (Nuedexta®) clinical use. Pharmacol Ther. 2016;164:170–82. https://doi.org/10.1016/j.pharmthera.2016.04.010.
Schadel M, Wu D, Otton SV, Kalow W, Sellers EM. Pharmacokinetics of dextromethorphan and metabolites in humans: influence of the CYP2D6 phenotype and quinidine inhibition. J Clin Psychopharmacol. 1995;15:263–9. https://doi.org/10.1097/00004714-199508000-00005.
Pechnick RN, Poland RE. Comparison of the effects of dextromethorphan, dextrorphan, and levorphanol on the hypothalamo-pituitary-adrenal axis. J Pharmacol Exp Ther. 2004;309:515–22. https://doi.org/10.1124/jpet.103.060038.
Miller SC. Dextromethorphan to dextrorphan: a pathway towards abuse liability. Hum Psychopharmacol. 2011;26:89–90. https://doi.org/10.1002/hup.1164. (author reply 91).
Schatzberg AF. Understanding the efficacy and mechanism of action of a dextromethorphan-bupropion combination: where does it fit in the NMDA versus mu-Opioid story? Am J Psychiatry. 2022;179:448–50. https://doi.org/10.1176/appi.ajp.20220434.
Zawertailo LA, Kaplan HL, Busto UE, Tyndale RF, Sellers EM. Psychotropic effects of dextromethorphan are altered by the CYP2D6 polymorphism: a pilot study. J Clin Psychopharmacol. 1998;18:332–7. https://doi.org/10.1097/00004714-199808000-00014.
Schoedel KA, Morrow SA, Sellers EM. Evaluating the safety and efficacy of dextromethorphan/quinidine in the treatment of pseudobulbar affect. Neuropsychiatr Dis Treat. 2014;10:1161–74. https://doi.org/10.2147/NDT.S30713.
Zawertailo LA, Tyndale RF, Busto U, Sellers EM. Effect of metabolic blockade on the psychoactive effects of dextromethorphan. Hum Psychopharmacol. 2010;25:71–9. https://doi.org/10.1002/hup.1086.
Jones A, Anderson A, Tabuteau H. 40. Efficacy and safety of AXS-05 in the prevention of relapse in patients with treatment-resistant depression: results from the MERIT trial. In: Poster presented at: annual meeting of the American Psychiatric Association; 2022 May 20–24; New Orleans (LA).
Moriguchi S, Takamiya A, Noda Y, Horita N, Wada M, Tsugawa S, et al. Glutamatergic neurometabolite leve1ls in major depressive disorder: a systematic review and meta-analysis of proton magnetic resonance spectroscopy studies. Mol Psychiatry. 2019;24:952–64. https://doi.org/10.1038/s41380-018-0252-9.
Onaolapo AY, Onaolapo OJ. Glutamate and depression: reflecting a deepening knowledge of the gut and brain effects of a ubiquitous molecule. World J Psychiatry. 2021;11:297–315. https://doi.org/10.5498/wjp.v11.i7.297.
Sanacora G, Treccani G, Popoli M. Towards a glutamate hypothesis of depression: an emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology. 2012;62:63–77. https://doi.org/10.1016/j.neuropharm.2011.07.036.
Sarawagi A, Soni ND, Patel AB. Glutamate and GABA homeostasis and neurometabolism in major depressive disorder. Front Psychiatry. 2021;12:637863. https://doi.org/10.3389/fpsyt.2021.637863.
Duman RS, Sanacora G, Krystal JH. Altered connectivity in depression: GABA and glutamate neurotransmitter deficits and reversal by novel treatments. Neuron. 2019;102:75–90. https://doi.org/10.1016/j.neuron.2019.03.013.
Banasr M, Dwyer JM, Duman RS. Cell atrophy and loss in depression: reversal by antidepressant treatment. Curr Opin Cell Biol. 2011;23:730–7. https://doi.org/10.1016/j.ceb.2011.09.002.
Adell A. Brain NMDA receptors in schizophrenia and depression. Biomolecules. 2020;10:947. https://doi.org/10.3390/biom10060947.
Chan SY, Matthews E, Burnet PWJ. ON or OFF? Modulating the N-Methyl-D-aspartate receptor in major depression. Front Mol Neurosci. 2016;9:169. https://doi.org/10.3389/fnmol.2016.00169.
Sattar Y, Wilson J, Khan AM, Adnan M, Azzopardi Larios D, Shrestha S, et al. A review of the mechanism of antagonism of N-methyl-D-aspartate receptor by ketamine in treatment-resistant depression. Cureus. 2018;10:e2652. https://doi.org/10.7759/cureus.2652.
Nguyen L, Matsumoto RR. Involvement of AMPA receptors in the antidepressant-like effects of dextromethorphan in mice. Behav Brain Res. 2015;295:26–34. https://doi.org/10.1016/j.bbr.2015.03.024.
Amidfar M, Woelfer M, Réus GZ, Quevedo J, Walter M, Kim Y-K. The role of NMDA receptor in neurobiology and treatment of major depressive disorder: evidence from translational research. Prog Neuropsychopharmacol Biol Psychiatry. 2019;94:109668. https://doi.org/10.1016/j.pnpbp.2019.109668.
Zhou W, Wang N, Yang C, Li X-M, Zhou Z-Q, Yang J-J. Ketamine-induced antidepressant effects are associated with AMPA receptors-mediated upregulation of mTOR and BDNF in rat hippocampus and prefrontal cortex. Eur Psychiatry. 2014;29:419–23. https://doi.org/10.1016/j.eurpsy.2013.10.005.
Lee S-Y, Wang T-Y, Chen S-L, Chang Y-H, Chen P-S, Huang S-Y, et al. Combination of dextromethorphan and memantine in treating bipolar spectrum disorder: a 12-week double-blind randomized clinical trial. Int J Bipolar Disord. 2020;8:11. https://doi.org/10.1186/s40345-019-0174-8.
Nguyen L, Robson MJ, Healy JR, Scandinaro AL, Matsumoto RR. Involvement of sigma-1 receptors in the antidepressant-like effects of dextromethorphan. PLoS ONE. 2014;9:e89985. https://doi.org/10.1371/journal.pone.0089985.
Ren P, Wang J, Li N, Li G, Ma H, Zhao Y, et al. Sigma-1 receptors in depression: mechanism and therapeutic development. Front Pharmacol. 2022;13:925879. https://doi.org/10.3389/fphar.2022.925879.
Wang D, Noda Y, Tsunekawa H, Zhou Y, Miyazaki M, Senzaki K, et al. Role of N-methyl-D-aspartate receptors in antidepressant-like effects of sigma 1 receptor agonist 1-(3,4-dimethoxyphenethyl)-4-(3-phenylpropyl)piperazine dihydrochloride (SA-4503) in olfactory bulbectomized rats. J Pharmacol Exp Ther. 2007;322:1305–14. https://doi.org/10.1124/jpet.107.124685.
Fishback JA, Robson MJ, Xu Y-T, Matsumoto RR. Sigma receptors: potential targets for a new class of antidepressant drug. Pharmacol Ther. 2010;127:271–82. https://doi.org/10.1016/j.pharmthera.2010.04.003.
Mandelli L, Wang S-M, Han C, Lee S-J, Patkar AA, Masand PS, et al. The impact of a single nucleotide polymorphism in SIGMAR1 on depressive symptoms in major depressive disorder and bipolar disorder. Adv Ther. 2017;34:713–24. https://doi.org/10.1124/jpet.107.124685.
Skuza G, Rogóz Z. Antidepressant-like effect of PRE-084, a selective sigma1 receptor agonist, in Albino Swiss and C57BL/6J mice. Pharmacol Rep. 2009;61:1179–83. https://doi.org/10.1016/s1734-1140(09)70181-1.
Rosen DA, Seki SM, Fernández-Castañeda A, Beiter RM, Eccles JD, Woodfolk JA, et al. Modulation of the sigma-1 receptor-IRE1 pathway is beneficial in preclinical models of inflammation and sepsis. Sci Transl Med. 2019;11:eaau5266. https://doi.org/10.1126/scitranslmed.aau5266.
Stahl SM. Dextromethorphan/Bupropion: a novel oral NMDA (N-methyl-d-aspartate) receptor antagonist with multimodal activity. CNS Spectr. 2019;24:461–6. https://doi.org/10.1017/S1092852919001470.
Stahl SM, Pradko JF, Haight BR, Modell JG, Rockett CB, Learned-Coughlin S. A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiatry. 2004;6:159–66. https://doi.org/10.4088/pcc.v06n0403.
Dhir A, Kulkarni SK. Possible involvement of sigma-1 receptors in the anti-immobility action of bupropion, a dopamine reuptake inhibitor. Fundam Clin Pharmacol. 2008;22:387–94. https://doi.org/10.1111/j.1472-8206.2008.00605.x.
Bagdas D, AlSharari S, Roni MA, Campbell VC, Muldoon PP, Carroll FI, et al. Blockade of nicotinic acetylcholine receptor enhances the responsiveness to bupropion in the mouse forced swim test. Behav Brain Res. 2019;360:262–9. https://doi.org/10.1016/j.bbr.2018.12.027.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research did not receive any grants from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
Dr. Taeho Gregory Rhee was supported in part by the National Institute on Aging (NIA) through Yale School of Medicine (#T32AG019134) in the past 3 years. Dr. Rhee has also been funded by the NIA (#R21AG070666), National Institute of Mental Health (#R21MH117438) and Institute for Collaboration on Health, Intervention, and Policy (InCHIP) of the University of Connecticut. Dr. Rhee serves as a review committee member for Patient-Centered Outcomes Research Institute (PCORI) and Substance Abuse and Mental Health Services Administration (SAMHSA) and has received honoraria payments from PCORI and SAMHSA. Dr. Rhee has also served as a stakeholder/consultant for PCORI and received consulting fees from PCORI. Dr. Rhee serves as an advisory committee member for International Alliance of Mental Health Research Funders (IAMHRF). Dr. Rhee is currently a co-editor-in-chief of Mental Health Science and has received honorarium payments annually from the publisher, John Wiley & Sons, Inc. Kayla M. Teopiz has received personal fees from Braxia Scientific Corp. Dr. Roger S. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC) and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes,Neumora Therapeutics, Boehringer Ingelheim,Sage,Biogen,Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals,Viatris, Abbvie, Atai Life Sciences. Dr. Roger McIntyre is a CEO of Braxia Scientific Corp. Drs Akbar, Ceban, Ho, Cao, Subramaniapillai, Kwan and Rosenblat have no conflicts of interest to declare.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Authors’ contributions
DA: data curation, investigation, project administration, visualization, writing—original draft. TGR: writing—review and editing. FC: writing—review and editing. RH: writing—review and editing. KMT: writing—review and editing. BC: writing—review and editing. MS: writing—review and editing. ATHK: writing—review and editing. JDR: writing—review and editing. RSM: conceptualization, project administration, visualization, supervision, writing—review and editing. All authors have read and approve the final version of this manuscript and agree to be accountable for the work.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Akbar, D., Rhee, T.G., Ceban, F. et al. Dextromethorphan-Bupropion for the Treatment of Depression: A Systematic Review of Efficacy and Safety in Clinical Trials. CNS Drugs 37, 867–881 (2023). https://doi.org/10.1007/s40263-023-01032-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-023-01032-5