Abstract
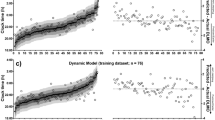
We aimed to establish a method for estimating dim light melatonin onset (DLMO) using mathematical slopes calculated from melatonin concentrations at three sampling points before and after sleep in children. The saliva of 30 children (mean age ± SD: 10.2 ± 1.3 years old) was collected under dim-light conditions up to six times every hour starting at 17:30 (t17), namely, 18:30 (t18), 19:30 (t19), 20:30 (t20), 21:30 (t21), 22:30 (t22), and 23:30 (t23), in the evening, and at 6:00 (t30) the following morning. We calculated \({SLOPE}_{on}\) (mathematical slope between melatonin concentrations at t18 and t20, t21 or t22), \({SLOPE}_{off}\) (the slope between t20, t21 or t22, and t30), and \(\Delta SLOPE\), which is generated by subtracting \({SLOPE}_{on}\) from \({SLOPE}_{off}\). DLMO was estimated by multiple regression analysis with the leave-one-out cross-validation (LOOCV) method using \({SLOPE}_{on}\) and \({SLOPE}_{off}\), and \(\Delta SLOPE\). The intraclass correlation coefficient (ICC) between the estimated and measured DLMOs was used as the index of estimation accuracy. DLMOs estimated using multiple regression equations with \({SLOPE}_{on}\) and \({SLOPE}_{off}\) yielded significant ICCs for the measured DLMOs, with the largest ICC at t20 (ICC = 0.634). Additionally, the ICC between the estimated and measured DLMOs using the equation with \(\Delta SLOPE\) was significant, with a larger ICC at t20 (ICC = 0.726) than that of the equation with \({SLOPE}_{on}\) and \({SLOPE}_{off}\). Our results showed that DLMO could be estimated with a certain level of accuracy from salivary melatonin levels at three time points before and after sleep in children.



Similar content being viewed by others
Abbreviations
- DLMO:
-
Dim light melatonin onset
- t18, t20, t21, t22, and t30:
-
Salivary melatonin measured at 18:30, 20:30, 21:30, 22:30 and 6:00 (the next morning)
- Mel1st :
-
Melatonin concentration at t18
- Mel2nd :
-
Melatonin concentration at t20, t21, or t22
- Mel3rd :
-
Melatonin concentration at t30
- \({SLOPE}_{on}\) :
-
Slope between Mel1st and Mel2nd
- \({SLOPE}_{off}\) :
-
Slope between Mel2nd and Mel3rd
- \(\Delta SLOPE\) :
-
Difference between \({SLOPE}_{on}\) and \({SLOPE}_{off}\)
- DLMOact :
-
Measured DLMO value
- DLMOest :
-
Estimated DLMO value
- LOOCV:
-
Leave-one-out cross-validation
- RMSE:
-
Root mean square error
- MAE:
-
Mean absolute error
- ICC:
-
Intraclass correlation coefficient
- LoA:
-
Limit of agreement
References
Lewy AJ, Cutler NL, Sack RL. The endogenous melatonin profile as a marker for circadian phase position. J Biol Rhythms. 1999;14:227–36.
Arendt J. Melatonin: characteristics, concerns, and prospects. J Biol Rhythms. 2005;20:291–303.
Benloucif S, Burgess HJ, Klerman EB, Lewy AJ, Middleton B, Murphy PJ, et al. Measuring melatonin in humans. J Clin Sleep Med. 2008;4:66–9.
Glacet R, Reynaud E, Robin-Choteau L, Reix N, Hugueny L, Ruppert E, et al. A comparison of four methods to estimate dim light melatonin onset: a repeatability and agreement study. Chronobiol Int. 2022;40:123–31.
Wever RA. Internal interactions within the human circadian system: the masking effect. Experientia. 1985;41:332–42.
Czeisler CA, Duffy JF, Shanahan TL, Brown EN, Mitchell JF, Rimmer DW, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science. 1999;284:2177–81.
Minors DS, Waterhouse JM. The use of constant routines in unmasking the endogenous component of human circadian rhythms. Chronobiol Int. 1984;1:205–16.
Kennaway DJ. Measuring melatonin by immunoassay. J Pineal Res. 2020;69:1–25.
Crowley SJ, Suh C, Molina TA, Fogg LF, Sharkey KM, Carskadon MA. Estimating the dim light melatonin onset of adolescents within a 6-h sampling window: the impact of sampling rate and threshold method. Sleep Med. 2016;20:59–66.
Werner H, Lebourgeois MK, Geiger A, Jenni OG. Assessment of chronotype in four- to eleven-year-old children: reliability and validity of the Children’s Chronotype Questionnaire (CCTQ). Chronobiol Int. 2009;26:992–1014.
Ishihara K, Doi Y, Uchiyama M. The reliability and validity of the Japanese version of the Children’s ChronoType Questionnaire (CCTQ) in preschool children. Chronobiol Int. 2014;31:947–53.
Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: Daily temporal patterns of human chronotypes. J Biol Rhythms. 2003;18:80–90.
Kitamura S, Hida A, Aritake S, Higuchi S, Enomoto M, Kato M, et al. Validity of the Japanese version of the Munich ChronoType Questionnaire. Chronobiol Int. 2014;31:845–50.
Carskadon MA, Acebo C, Richardson GS, Tate BA, Seifer R. An approach to studying circadian rhythms of adolescent humans. J Biol Rhythms. 1997;12:278–89.
Crowley SJ, Acebo C, Fallone G, Carskadon MA. Estimating dim light melatonin onset (DLMO) phase in adolescents using summer or school-year sleep/wake schedules. Sleep. 2006;29:1632–41.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Gamer M, Lemon J, Fellows I, Singh P. IRR: Various coefficients of interrater reliability and agreement [Internet]. 2019. Available from: https://CRAN.R-project.org/package=irr
Kasukawa T, Sugimoto M, Hida A, Minami Y, Mori M, Honma S, et al. Human blood metabolite timetable indicates internal body time. Proc Natl Acad Sci USA. 2012;109:15036–41.
Laing EE, Möller-Levet CS, Poh N, Santhi N, Archer SN, Dijk D-J. Blood transcriptome based biomarkers for human circadian phase. Elife. 2017;6: e20214.
Hughey JJ. Machine learning identifies a compact gene set for monitoring the circadian clock in human blood. Genome Med. 2017;9:19.
Braun R, Kath WL, Iwanaszko M, Kula-Eversole E, Abbott SM, Reid KJ, et al. Universal method for robust detection of circadian state from gene expression. Proc Natl Acad Sci USA. 2018;115:E9247–56.
Wittenbrink N, Ananthasubramaniam B, Münch M, Koller B, Maier B, Weschke C, et al. High-accuracy determination of internal circadian time from a single blood sample. J Clin Invest. 2018;128:3826–39.
Kolodyazhniy V, Späti J, Frey S, Götz T, Wirz-Justice A, Kräuchi K, et al. Estimation of human circadian phase via a multi-channel ambulatory monitoring system and a multiple regression model. J Biol Rhythms. 2011;26:55–67.
Kolodyazhniy V, Späti J, Frey S, Götz T, Wirz-Justice A, Kräuchi K, et al. An improved method for estimating human circadian phase derived from multichannel ambulatory monitoring and artificial neural networks. Chronobiol Int. 2012;29:1078–97.
Stone JE, Phillips AJK, Ftouni S, Magee M, Howard M, Lockley SW, et al. Generalizability of a neural network model for circadian phase prediction in real-world conditions. Sci Rep. 2019;9:11001.
Wright H, Lack L, Bootzin R. Relationship between dim light melatonin onset and the timing of sleep in sleep onset insomniacs. Sleep Biol Rhythms. 2006;4:78–80.
Reiter AM, Sargent C, Roach GD. Finding DLMO: estimating dim light melatonin onset from sleep markers derived from questionnaires, diaries and actigraphy. Chronobiol Int. 2020;37:1412–24.
Zeitzer JM, Dijk DJ, Kronauer RE, Brown EN, Czeisler CA. Sensitivity of the human circadian pacemaker to nocturnal light: Melatonin phase resetting and suppression. J Physiol. 2000;526:695–702.
Komada Y, Aoki K, Gohshi S, Ichioka H, Shibata S. Effects of television luminance and wavelength at habitual bedtime on melatonin and cortisol secretion in humans. Sleep Biol Rhythms. 2015;13:316–22.
Kubota N, Tamori Y, Baba K, Yamanaka Y. Effects of different light incident angles via a head-mounted device on the magnitude of nocturnal melatonin suppression in healthy young subjects. Sleep Biol Rhythms. 2022;20:247–54.
Eto T, Higuchi S. Review on age-related differences in non-visual effects of light: melatonin suppression, circadian phase shift and pupillary light reflex in children to older adults. J Physiol Anthropol. 2023;42:11.
Lockley SW, Brainard GC, Czeisler CA. High sensitivity of the human circadian melatonin rhythm to resetting by short wavelength light. J Clin Endocrinol Metab. 2003;88:4502–5.
Rahman SA, St Hilaire MA, Gronfier C, Chang AM, Santhi N, Czeisler CA, et al. Functional decoupling of melatonin suppression and circadian phase resetting in humans. J Physiol. 2018;596:2147–57.
Moreno JP, Dadabhoy H, Musaad S, Baranowski T, Thompson D, Alfano CA, et al. Evaluation of a circadian rhythm and sleep-focused mobile health intervention for the prevention of accelerated summer weight gain among elementary school-age children: protocol for a randomized controlled feasibility study. JMIR Res Protoc. 2022;11: e37002.
Eto T, Kitamura S, Nishimura K, Takeoka K, Nishimura Y, Lee S-I, et al. Circadian phase advances in children during camping life according to the natural light-dark cycle. J Physiol Anthropol. 2022;41:1–10.
van Maanen A, Meijer AM, Smits MG, van der Heijden KB, Oort FJ. Effects of melatonin and bright light treatment in childhood chronic sleep onset insomnia with late melatonin onset: a randomized controlled study. Sleep. 2017;40:zsw038.
Higuchi S, Lee S-I, Kozaki T, Harada T, Tanaka I. Late circadian phase in adults and children is correlated with use of high color temperature light at home at night. Chronobiol Int. 2016;33:448–52.
Acknowledgements
We thank the participants for their participation in this study.
Funding
This study was supported in part by the JSPS KAKENHI (JP19K21785). The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
SK, AS, and SN designed the study. AS and SN acquired the samples. TE, SK, and SH analyzed the data. TE and SK drafted the manuscript. AS, KT, SH, and SN reviewed the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethical approval
This study was approved by the Institutional Review Board of Nippon Sport Science University, Japan (Approval No. 019-H057). All procedures involving human participants were conducted in accordance with the ethical standards of institutional and/or national research committees. All participants provided informed consent.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Eto, T., Kitamura, S., Shikano, A. et al. Estimating dim light melatonin onset time in children using delta changes in melatonin. Sleep Biol. Rhythms 22, 239–246 (2024). https://doi.org/10.1007/s41105-023-00493-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-023-00493-x