Abstract
Purpose
Whether long-term aspirin usage is associated with colorectal cancer (CRC) risk needs more evidence. The study evaluated the association between long-term aspirin use and prevalence of CRC in a large, nationally representative database.
Methods
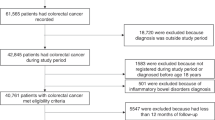
Hospitalized patients aged ≥ 50 years during 2018 were identified in the United States (US) National Inpatient Sample (NIS). Patients without complete information of age, sex, race, income, and insurance status were excluded, as well as those with inflammatory bowel disease (IBD) or malignancies other than CRC. Propensity score matching (PSM) was applied to balance the characteristics between patients with and without long-term aspirin use. Logistic regressions were performed to determine the relationship between long-term aspirin use and the presence of CRC. CRC and aspirin use were identified through the administrative International Classification of Diseases (ICD) codes.
Results
Data from 3,490,226 patients were included, in which 688,018 (19.7%) had a record of long-term aspirin use. After 1:1 PSM, there remained 1,376,006 patients, representing 6,880,029 individuals in the US after weighting. After adjusting for confounders, long-term aspirin use was significantly associated with lower CRC odds (adjusted odds ratio [aOR] = 0.64, 95% confidence interval [CI] 0.62, 0.67). This association was not changed when stratified by age, sex, race, body mass index (BMI), and smoking.
Conclusions
From a national inpatient dataset, US adults ≥ 50 years on long-term aspirin are less likely to have CRC, regardless of age, sex, race, BMI, and smoking status.

Similar content being viewed by others
Data availability
All data use to support the findings of this study are included within the article.
References
Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB (2019) Colorectal cancer. Lancet 394:1467–1480
Siegel RL, Miller KD, Goding Sauer A et al (2020) Colorectal cancer statistics, 2020. CA Cancer J Clin 70:145–164
Arnold M, Sierra MS, Laversanne M et al (2017) Global patterns and trends in colorectal cancer incidence and mortality. Gut 66:683–691
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Garcia-Albeniz X, Chan AT (2011) Aspirin for the prevention of colorectal cancer. Best Pract Res Clin Gastroenterol 25:461–472
Mármol I, Sánchez-de-Diego C, Pradilla Dieste A, Cerrada E, Rodriguez Yoldi MJ (2017) Colorectal carcinoma: a general overview and future perspectives in colorectal cancer. Int J Mol Sci 18:197
Botteri E, Iodice S, Bagnardi V et al (2008) Smoking and colorectal cancer: a meta-analysis. JAMA 300:2765–2778
Cai S, Li Y, Ding Y, Chen K, Jin M (2014) Alcohol drinking and the risk of colorectal cancer death: a meta-analysis. Eur J Cancer Prev 23:532–539
Kyrgiou M, Kalliala I, Markozannes G et al (2017) Adiposity and cancer at major anatomical sites: umbrella review of the literature. BMJ 356:j477
Clarke WT, Feuerstein JD (2019) Colorectal cancer surveillance in inflammatory bowel disease: practice guidelines and recent developments. World J Gastroenterol 25:4148–4157
Simon K (2016) Colorectal cancer development and advances in screening. Clin Interv Aging 11:967–976
Soltani G, Poursheikhani A, Yassi M et al (2019) Obesity, diabetes and the risk of colorectal adenoma and cancer. BMC Endocr Disord 19:113
Meeker S, Seamons A, Maggio-Price L, Paik J (2016) Protective links between vitamin D, inflammatory bowel disease and colon cancer. World J Gastroenterol 22:933–948
Dovizio M, Alberti S, Sacco A et al (2015) Novel insights into the regulation of cyclooxygenase-2 expression by platelet-cancer cell cross-talk. Biochem Soc Trans 43:707–714
Rouzer CA, Marnett LJ (2009) Cyclooxygenases: structural and functional insights. J Lipid Res 50(Suppl):S29-34
Ricciotti E, FitzGerald GA (2011) Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol 31:986–1000
Bauersachs R, Zeymer U, Brière JB et al (2019) Burden of coronary artery disease and peripheral artery disease: a literature review. Cardiovasc Ther. https://doi.org/10.1155/2019/8295054
De Caterina R, Renda G (2012) Clinical use of aspirin in ischemic heart disease: past, present and future. Curr Pharm Des 18:5215–5223
Smith DK, Demetriou T, Weber C (2019) Aspirin for primary prevention: USPSTF recommendations for CVD and colorectal cancer. J Fam Pract 68:146–151
Andreotti F, De Caterina R, Crea F (2017) Aspirin and the prevention of a common disease: colorectal cancer. Int J Cardiol 248:394–395
Drew DA, Cao Y, Chan AT (2016) Aspirin and colorectal cancer: the promise of precision chemoprevention. Nat Rev Cancer 16:173–186
Rodríguez-Miguel A, García-Rodríguez LA, Gil M et al (2019) Clopidogrel and low-dose aspirin, alone or together, reduce risk of colorectal cancer. Clin Gastroenterol Hepatol 17:2024-2033.e2022
Singh Ranger G (2016) The role of aspirin in colorectal cancer chemoprevention. Crit Rev Oncol Hematol 104:87–90
Hollestein LM, van Herk-Sukel MP, Ruiter R et al (2014) Incident cancer risk after the start of aspirin use: results from a Dutch population-based cohort study of low dose aspirin users. Int J Cancer 135:157–165
Kim B, Park SJ, Hong SP et al (2015) The effect of prediagnostic aspirin use on the prognosis of stage III colorectal cancer. Int J Clin Exp Med 8:13435–13445
Dasenbrock HH, Yan SC, Gross BA et al (2017) The impact of aspirin and anticoagulant usage on outcomes after aneurysmal subarachnoid hemorrhage: a Nationwide Inpatient Sample analysis. J Neurosurg 126(2):537–547
Chaudhry H, Sohal A, Dukovic D et al (2023) Does use of long-term aspirin impact outcomes in patients with acute pancreatitis? Eur J Gastroenterol Hepatol 35(7):721–727
Li P, Ning Y, Li M et al (2020) Aspirin is associated with reduced rates of venous thromboembolism in older patients with cancer. J Cardiovasc Pharmacol Ther 25(5):456–465
Fitzpatrick FA (2004) Cyclooxygenase enzymes: regulation and function. Curr Pharm Des 10:577–588
Sankaranarayanan R, Kumar DR, Altinoz MA, Bhat GJ (2020) Mechanisms of colorectal cancer prevention by aspirin-A literature review and perspective on the role of COX-dependent and -independent pathways. Int J Mol Sci. https://doi.org/10.3390/ijms21239018
Kirkby NS, Lundberg MH, Harrington LS et al (2012) Cyclooxygenase-1, not cyclooxygenase-2, is responsible for physiological production of prostacyclin in the cardiovascular system. Proc Natl Acad Sci U S A 109:17597–17602
Patrono C (2016) Cardiovascular effects of cyclooxygenase-2 inhibitors: a mechanistic and clinical perspective. Br J Clin Pharmacol 82:957–964
Simmons DL, Botting RM, Hla T (2004) Cyclooxygenase isozymes: the biology of prostaglandin synthesis and inhibition. Pharmacol Rev 56:387–437
Dubois RN (2000) Review article: cyclooxygenase–a target for colon cancer prevention. Aliment Pharmacol Ther 14(Suppl 1):64–67
Yu Y, Stubbe J, Ibrahim S et al (2010) Cyclooxygenase-2-dependent prostacyclin formation and blood pressure homeostasis: targeted exchange of cyclooxygenase isoforms in mice. Circ Res 106:337–345
Gurram B, Zhang S, Li M et al (2018) Celecoxib conjugated fluorescent probe for identification and discrimination of cyclooxygenase-2 enzyme in cancer cells. Anal Chem 90:5187–5193
van Rees BP, Ristimäki A (2001) Cyclooxygenase-2 in carcinogenesis of the gastrointestinal tract. Scand J Gastroenterol 36:897–903
Sano H, Kawahito Y, Wilder RL et al (1995) Expression of cyclooxygenase-1 and -2 in human colorectal cancer. Cancer Res 55:3785–3789
Negi RR, Rana SV, Gupta V et al (2019) Over-expression of cyclooxygenase-2 in colorectal cancer patients. Asian Pac J Cancer Prev 20:1675–1681
Roelofs HM, Te Morsche RH, van Heumen BW, Nagengast FM, Peters WH (2014) Over-expression of COX-2 mRNA in colorectal cancer. BMC Gastroenterol 14:1
Raber I, McCarthy CP, Vaduganathan M et al (2019) The rise and fall of aspirin in the primary prevention of cardiovascular disease. Lancet 393:2155–2167
Dasa O, Jun I, Sajdeya R et al (2021) Gender and racial disparities in aspirin use for primary prevention: temporal trends from the national health and nutrition examination surveys, 2011–2018. Circulation 143:AP078
Yerman T, Gan WQ, Sin DD (2007) The influence of gender on the effects of aspirin in preventing myocardial infarction. BMC Med 5:29
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
K-CL and K-CC: conception and design; acquisition of data; analysis and interpretation of data; critical revision of the manuscript; final approval of the manuscript; drafting of the manuscript; definition of intellectual content; literature research; supervision. H-HC, K-CC, K-LW, and L-CS: Conception and design; Acquisition of data; Analysis and interpretation of data; Critical revision of the manuscript; Final approval of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing of interest.
Research involving human and animals participants
The study protocol was submitted to the Institutional Review Board (IRB) of Kaohsiung Chang Gung Memorial Hospital and Chang Gung University College of Medicine, and the study was granted an exemption from IRB approval.
Informed consent
Due to the fact that all data in the NIS database is de-identified, informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, KC., Chung, KC., Chen, HH. et al. Potential beneficial effects of long-term aspirin use on the prevalence of colorectal cancer: a population-based study of the US Nationwide Inpatient Sample. Cancer Causes Control 35, 477–486 (2024). https://doi.org/10.1007/s10552-023-01803-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01803-x