Abstract
Purpose of Review
The use of immune checkpoint inhibitors (ICIs) for oncologic indications is associated with immune-related adverse events (irAEs). Patients with pre-existing autoimmune diseases are at increased risk of irAEs and have largely been excluded from clinical trials of ICIs. Therefore, there is limited data on the safety of safety of ICIs in patients with pre-existing neurologic autoimmune diseases (nAIDs) such as myasthenia gravis and multiple sclerosis. This review aims to synthesize the literature on the post-marketing experience with ICI in patients with pre-existing nAID and to discuss possible strategies for mitigating the risk of post-ICI nAID relapses.
Recent Findings
Patients with pre-existing myasthenia gravis (MG), myositis, and paraneoplastic encephalitis appear highly susceptible to neurologic relapses of their underlying neurologic disorder following ICI initiation; these relapses can cause considerable morbidity and mortality. In patients with multiple sclerosis (MS), the risk and severity of MS relapses following ICI appears to be relatively lower compared to MG. Preliminary evidence suggests that older MS patients with no recent focal neuroinflammatory activity may be safely treated with ICI. Among the several case reports of ICI in patients with a history of Guillain–Barre syndrome (GBS), neurologic worsening was only recorded in one patient who was in the acute phase of GBS at the time of ICI start.
Summary
Initiating an ICI in a patient with pre-existing nAID involves a complex risk-benefit discussion between the patient, their oncologist, and neurologist. Relevant issues to consider before ICI include the choice of disease-modifying therapy for nAID (if any) and strategies for promptly identifying and managing nAID relapses should they occur. Currently, the literature consists mainly of case reports and case series, subject to publication bias. Prospective studies of ICI in patients with nAID are needed to improve the level of evidence.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Shiravand Y, Khodadadi F, Kashani SMA, Hosseini-Fard SR, Hosseini S, Sadeghirad H, et al. Immune checkpoint inhibitors in cancer therapy. Curr Oncol. 2022;29(5):3044–60. https://doi.org/10.3390/curroncol29050247.
• Haugh AM, Probasco JC, Johnson DB. Neurologic complications of immune checkpoint inhibitors. Expert Opin Drug Saf. 2020;19(4):479–88. https://doi.org/10.1080/14740338.2020.1738382. The authors provide a comprehensive review of the different neurological complications of ICIs.
Twomey JD, Zhang B. Cancer immunotherapy update: FDA-approved checkpoint inhibitors and companion diagnostics. Aaps j. 2021;23(2):39. https://doi.org/10.1208/s12248-021-00574-0.
Vaddepally R, Doddamani R, Sodavarapu S, Madam NR, Katkar R, Kutadi AP, et al. Review of immune-related adverse events (irAEs) in non-small-cell lung cancer (NSCLC)-their incidence, management, multiorgan irAEs, and rechallenge. Biomedicines. 2022;10(4). https://doi.org/10.3390/biomedicines10040790.
Danlos FX, Voisin AL, Dyevre V, Michot JM, Routier E, Taillade L, et al. Safety and efficacy of anti-programmed death 1 antibodies in patients with cancer and pre-existing autoimmune or inflammatory disease. Eur J Cancer. 2018;91:21–9. https://doi.org/10.1016/j.ejca.2017.12.008.
• Yshii LM, Hohlfeld R, Liblau RS. Inflammatory CNS disease caused by immune checkpoint inhibitors: status and perspectives. Nat Rev Neurol. 2017;13(12):755–63. https://doi.org/10.1038/nrneurol.2017.144. This paper surveys various theories about the pathophysiology and mechanism of CNS disease with ICIs.
Puzanov I, Diab A, Abdallah K, Bingham CO 3rd, Brogdon C, Dadu R, et al. Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer. 2017;5(1):95. https://doi.org/10.1186/s40425-017-0300-z.
Abdel-Wahab N, Shah M, Lopez-Olivo MA, Suarez-Almazor ME. Use of immune checkpoint inhibitors in the treatment of patients with cancer and pre-existing autoimmune disease: a systematic review. Ann Intern Med. 2018;168(2):121–30. https://doi.org/10.7326/m17-2073.
Calvo V, Fernández MA, Collazo-Lorduy A, Franco F, Núñez B, Provencio M. Use of immune checkpoint inhibitors in patients with solid tumors and pre-existing autoimmune or inflammatory disease: real-world data. Lung Cancer Manag. 2021;10(4):Lmt51. https://doi.org/10.2217/lmt-2021-0003.
•• Haanen J, Ernstoff MS, Wang Y, Menzies AM, Puzanov I, Grivas P, et al. Autoimmune diseases and immune-checkpoint inhibitors for cancer therapy: review of the literature and personalized risk-based prevention strategy. Ann Oncol. 2020;31(6):724–44. https://doi.org/10.1016/j.annonc.2020.03.285.T. The authors propose risk-mitigation strategies for patients with pre-existing AID who plan to start ICI therapy
Jordan B, Benesova K, Hassel JC, Wick W, Jordan K. How we identify and treat neuromuscular toxicity induced by immune checkpoint inhibitors. ESMO Open. 2021;6(6):100317. https://doi.org/10.1016/j.esmoop.2021.100317.
Abidoye O, Kim N, Fombi J. An interesting case report of myasthenia gravis exacerbation induced by durvalumab. Cureus. 2022;14(7):e26985. https://doi.org/10.7759/cureus.26985.
Cooper DS, Meriggioli MN, Bonomi PD, Malik R. Severe exacerbation of myasthenia gravis associated with checkpoint inhibitor immunotherapy. J Neuromuscul Dis. 2017;4(2):169–73. https://doi.org/10.3233/jnd-170219.
Earl DE, Loochtan AI, Bedlack RS. Refractory myasthenia gravis exacerbation triggered by pembrolizumab. Muscle Nerve. 2018;57(4):E120-e121.
Zhu J, Li Y. Myasthenia gravis exacerbation associated with pembrolizumab. Muscle Nerve. 2016;54(3):506–7. https://doi.org/10.1002/mus.25055.
Kamien AK, Ana; Santhosh-Kumar, Cheruppolil. Reactivation of myasthenia gravis secondary to nivolumab: case report and literature review. J Hematol Oncol Pharm. 2019;9(1):24–9.
Lau KH, et al. Exacerbation of myasthenia gravis in a patient with melanoma treated with pembrolizumab. Muscle Nerve. 2016;54(1):157–61.
Maeda O, Yokota K, Atsuta N, Katsuno M, Akiyama M, Ando Y. Nivolumab for the treatment of malignant melanoma in a patient with pre-existing myasthenia gravis. Nagoya J Med Sci. 2016;78(1):119–22.
• Snavely A, Pérez-Torres EJ, Weber JS, Sandigursky S, Thawani SP. Immune checkpoint inhibition in patients with inactive pre-existing neuromuscular autoimmune diseases. J Neurol Sci. 2022;438:120275. https://doi.org/10.1016/j.jns.2022.120275. This case series documents neurologic outcomes in patients with pre-existing neuromuscular autoimmune diseases who are treated with ICI
Mitsune A, Yanagisawa S, Fukuhara T, Miyauchi E, Morita M, Ono M, et al. Relapsed myasthenia gravis after nivolumab treatment. Intern Med. 2018;57(13):1893–7. https://doi.org/10.2169/internalmedicine.9153-17.
Phadke SD, Ghabour R, Swick BL, Swenson A, Milhem M, Zakharia Y. Pembrolizumab therapy triggering an exacerbation of pre-existing autoimmune disease: a report of 2 patient cases. J Investig Med High Impact Case Rep. 2016;4(4):2324709616674316. https://doi.org/10.1177/2324709616674316.
Safa H, Johnson DH, Trinh VA, Rodgers TE, Lin H, Suarez-Almazor ME, et al. Immune checkpoint inhibitor-related myasthenia gravis: single center experience and systematic review of the literature. J Immunother Cancer. 2019;7(1):319. https://doi.org/10.1186/s40425-019-0774-y.
Williams S, et al. Outcome of patient with myasthenia gravis with the use of immunotherapy in metastatic Merkel cell carcinoma. Oxf Med Case Reports. 2022;2022(2):omac012.
Zaremba A, et al. Metastatic Merkel cell carcinoma and myasthenia gravis: contraindication for therapy with immune checkpoint inhibitors? J Immunother Cancer. 2019;7(1):141. https://doi.org/10.1186/s40425-019-0626-9
Menzies AM, Johnson DB, Ramanujam S, Atkinson VG, Wong ANM, Park JJ, et al. Anti-PD-1 therapy in patients with advanced melanoma and pre-existing autoimmune disorders or major toxicity with ipilimumab. Ann Oncol. 2017;28(2):368–76. https://doi.org/10.1093/annonc/mdw443.
Johnson DB, Sullivan RJ, Ott PA, Carlino MS, Khushalani NI, Ye F, et al. Ipilimumab therapy in patients with advanced melanoma and pre-existing autoimmune disorders. JAMA Oncol. 2016;2(2):234–40. https://doi.org/10.1001/jamaoncol.2015.4368.
Ishii A, Yokoyama M, Tsuji H, Fujii Y, Tamaoka A. Pembrolizumab treatment of metastatic urothelial cancer without exacerbating myasthenia gravis. eNeurologicalSci. 2020;19:100236. https://doi.org/10.1016/j.ensci.2020.100236.
Sanders DB, Burns TM, Cutter GR, Massey JM, Juel VC, Hobson-Webb L. Does change in acetylcholine receptor antibody level correlate with clinical change in myasthenia gravis? Muscle Nerve. 2014;49(4):483–6. https://doi.org/10.1002/mus.23944.
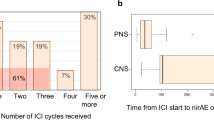
•• Khan E, Shrestha AK, Elkhooly M, Wilson H, Ebbert M, Srivastava S, et al. CNS and PNS manifestation in immune checkpoint inhibitors: a systematic review. J Neurol Sci. 2022;432:120089. https://doi.org/10.1016/j.jns.2021.120089. A well-written, comprehensive review of nirAEs of ICIs.
Thomas R, Patel H, Scott J. Dermatomyositis flare with immune checkpoint inhibitor therapy for melanoma. Cureus. 2021;13(4):e14387. https://doi.org/10.7759/cureus.14387.
Manson G, Maria ATJ, Poizeau F, Danlos FX, Kostine M, Brosseau S, et al. Worsening and newly diagnosed paraneoplastic syndromes following anti-PD-1 or anti-PD-L1 immunotherapies, a descriptive study. J Immunother Cancer. 2019;7(1):337. https://doi.org/10.1186/s40425-019-0821-8.
Uchio N, Unuma A, Kakumoto T, Osaki M, Zenke Y, Sakuta K, et al. Pembrolizumab on pre-existing inclusion body myositis: a case report. BMC Rheumatol. 2020;4:48. https://doi.org/10.1186/s41927-020-00144-5.
Puwanant A, Isfort M, Lacomis D, Živković SA. Clinical spectrum of neuromuscular complications after immune checkpoint inhibition. Neuromuscul Disord. 2019;29(2):127–33. https://doi.org/10.1016/j.nmd.2018.11.012.
Wang C, Sandhu J, Fakih M. Complete response to pembrolizumab in a patient with metastatic colon cancer with microsatellite instability and a history of Guillain-Barre syndrome. J Gastrointest Oncol. 2019;10(1):161–5. https://doi.org/10.21037/jgo.2018.09.19.
Cortellini A, Parisi A, Fargnoli MC, Cannita K, Irelli A, Porzio G, et al. Safe administration of ipilimumab, pembrolizumab, and nivolumab in a patient with metastatic melanoma, psoriasis, and a previous Guillain-Barré syndrome. Case Rep Oncol Med. 2018;2018:2783917. https://doi.org/10.1155/2018/2783917.
Yuen C, Kamson D, Soliven B, Kramer C, Goldenberg F, Rezania K. Severe relapse of vaccine-induced Guillain-Barré syndrome after treatment with nivolumab. J Clin Neuromuscul Dis. 2019;20(4):194–9. https://doi.org/10.1097/cnd.0000000000000230.
Hughes RAC, Brassington R, Gunn AA, van Doorn PA. Corticosteroids for Guillain‐Barré syndrome. Cochrane Database Syst Rev. 2016(10). https://doi.org/10.1002/14651858.CD001446.pub5.
Gettings EJ, Hackett CT, Scott TF. Severe relapse in a multiple sclerosis patient associated with ipilimumab treatment of melanoma. Mult Scler. 2015;21(5):670.
Garcia CR, et al. Multiple sclerosis outcomes after cancer immunotherapy. Clin Transl Oncol. 2019;21(10):1336–42.
Gómez Vicente L, et al. P04.07 Relapse in a paucisymptomatic form of multiple sclerosis in a patient treated with nivolumab. 2016: Soc Neuro Oncol Annual Meeting.
Gerdes LA, Held K, Beltrán E, Berking C, Prinz JC, Junker A, et al. CTLA4 as immunological checkpoint in the development of multiple sclerosis. Ann Neurol. 2016;80(2):294–300. https://doi.org/10.1002/ana.24715.
Lu BY, et al. Intracranial complications from immune checkpoint therapy in a patient with NSCLC and multiple sclerosis: case report. JTO Clin Res Rep. 2021;2(6):100183.
Romeo MAL, Garassino MC, Moiola L, Galli G, Comi G, Martinelli V, et al. Multiple sclerosis associated with pembrolizumab in a patient with non-small cell lung cancer. J Neurol. 2019;266(12):3163–6. https://doi.org/10.1007/s00415-019-09562-z.
Kähler KC, Eigentler TK, Gesierich A, Heinzerling L, Loquai C, Meier F, et al. Ipilimumab in metastatic melanoma patients with pre-existing autoimmune disorders. Cancer Immunol Immunother. 2018;67(5):825–34. https://doi.org/10.1007/s00262-018-2134-z.
Kyi C, et al. Ipilimumab in patients with melanoma and autoimmune disease. J Immunother Cancer. 2014;2(1):35.
Neuzil K, et al. Complete pathologic response to pembrolizumab and axitinib in a patient with sarcomatoid RCC and ocrelizumab-treated multiple sclerosis. Urology. 2022;164:50–4.
Hasan Ali O, et al. Fingolimod and tumor-infiltrating lymphocytes in checkpoint-inhibitor treated cancer patients. Cancer Immunol Immunother. 2021;70(2):563–8.
Liu EK, Chen JJ, Braunstein S. Management of adverse radiation effect associated with stereotactic radiosurgery of brain metastasis in multiple sclerosis. Adv Radiat Oncol. 2023;8(2):101150. https://doi.org/10.1016/j.adro.2022.101150.
Barry B, Erwin AA, Stevens J, Tornatore C. Fingolimod rebound: a review of the clinical experience and management considerations. Neurol Ther. 2019;8(2):241–50. https://doi.org/10.1007/s40120-019-00160-9.
Hatcher SE, Waubant E, Nourbakhsh B, Crabtree-Hartman E, Graves JS. Rebound syndrome in patients with multiple sclerosis after cessation of fingolimod treatment. JAMA Neurol. 2016;73(7):790–4. https://doi.org/10.1001/jamaneurol.2016.0826.
Gill A, Perez MA, Perrone CM, Bae CJ, Pruitt AA, Lancaster E. A case series of PD-1 inhibitor-associated paraneoplastic neurologic syndromes. J Neuroimmunol. 2019;334:576980. https://doi.org/10.1016/j.jneuroim.2019.576980.
Hottinger AF, de Micheli R, Guido V, Karampera A, Hagmann P, Du Pasquier R. Natalizumab may control immune checkpoint inhibitor-induced limbic encephalitis. Neurol Neuroimmunol Neuroinflamm. 2018;5(2):e439. https://doi.org/10.1212/NXI.0000000000000439.
Matsuoka H, Kimura H, Koba H, Tambo Y, Ohkura N, Hara J, et al. Nivolumab-induced limbic encephalitis with anti-Hu antibody in a patient with advanced pleomorphic carcinoma of the lung. Clin Lung Cancer. 2018;19(5):e597–9. https://doi.org/10.1016/j.cllc.2018.04.009.
Nasralla S, Abboud H. Is neuromyelitis optica without AQP4-IgG a T-cell mediated disease? Insights from checkpoint inhibitor immune-related adverse events. Mult Scler Relat Disord. 2020;46:102451. https://doi.org/10.1016/j.msard.2020.102451.
Papadopoulos KP, Romero RS, Gonzalez G, Dix JE, Lowy I, Fury M. Anti-Hu-associated autoimmune limbic encephalitis in a patient with PD-1 inhibitor-responsive myxoid chondrosarcoma. Oncologist. 2018;23(1):118–20. https://doi.org/10.1634/theoncologist.2017-0344.
Raibagkar P, Ho D, Gunturu KS, Srinivasan J. Worsening of anti-Hu paraneoplastic neurological syndrome related to anti-PD-1 treatment: case report and review of literature. J Neuroimmunol. 2020;341:577184. https://doi.org/10.1016/j.jneuroim.2020.577184.
Cao Y, Nylander A, Ramanan S, Goods BA, Ponath G, Zabad R, et al. CNS demyelination and enhanced myelin-reactive responses after ipilimumab treatment. Neurology. 2016;86(16):1553–6. https://doi.org/10.1212/WNL.0000000000002594.
•• Oliveira MCB, de Brito MH, Simabukuro MM. Central nervous system demyelination associated with immune checkpoint inhibitors: review of the literature. Front Neurol. 2020;11:538695. https://doi.org/10.3389/fneur.2020.538695. The authors review rare cases of CNS demyelination that occurred on ICI therapy.
•• Conway SE, Pua DKA, Holroyd KB, Galetta K, Bhattacharyya S. Neurologic disease activity in people with multiple sclerosis treated with immune checkpoint inhibitors. Mult Scler. 2023;29(3):471–4. https://doi.org/10.1177/13524585221117949. An important case series that suggests that ICI may be safe, from a neurologic standpoint, in older patients with stable MS.
Corboy JR, Fox RJ, Kister I, Cutter GR, Morgan CJ, Seale R, et al. Risk of new disease activity in patients with multiple sclerosis who continue or discontinue disease-modifying therapies (DISCOMS): a multicentre, randomised, single-blind, phase 4, non-inferiority trial. Lancet Neurol. 2023;22(7):568–77. https://doi.org/10.1016/S1474-4422(23)00154-0.
Sechi E, Markovic SN, McKeon A, Dubey D, Liewluck T, Lennon VA, et al. Neurologic autoimmunity and immune checkpoint inhibitors: autoantibody profiles and outcomes. Neurology. 2020;95(17):e2442–52. https://doi.org/10.1212/WNL.0000000000010632.
Belkhir R, Burel SL, Dunogeant L, Marabelle A, Hollebecque A, Besse B, et al. Rheumatoid arthritis and polymyalgia rheumatica occurring after immune checkpoint inhibitor treatment. Ann Rheum Dis. 2017;76(10):1747–50. https://doi.org/10.1136/annrheumdis-2017-211216.
Kobayashi T, Iwama S, Yasuda Y, Okada N, Tsunekawa T, Onoue T, et al. Patients with antithyroid antibodies are prone to develop destructive thyroiditis by nivolumab: a prospective study. J Endocr Soc. 2018;2(3):241–51. https://doi.org/10.1210/js.2017-00432.
Acknowledgements
We would like to thank Drs. Omar Hasan Ali, Massimo Filippi, Lisa Ann Gerdes, and Thomas Scott for providing us with additional data regarding their published cases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Raissa Aoun, Daniel Gratch, and David Kaminetzky each declare no potential conflicts of interest.
Ilya Kister served on advisory boards for Biogen, Genentech, Horizon and Alexion Pharmaceuticals, and received research support for investigator-initiated grants from Genentech, Sanofi Genzyme, Biogen, EMD Serono, National MS Society, and Guthy Jackson Charitable Foundation. He received royalties from Walters-Kluwer for “Top 100 Diagnosis in Neurology.”
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aoun, R., Gratch, D., Kaminetzky, D. et al. Immune Checkpoint Inhibitors in Patients with Pre-existing Neurologic Autoimmune Disorders. Curr Neurol Neurosci Rep 23, 735–750 (2023). https://doi.org/10.1007/s11910-023-01306-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-023-01306-x