Abstract
Acute kidney injury (AKI) has a significant impact on the short-term and long-term clinical outcomes of pediatric and neonatal patients, and it is imperative in these populations to mitigate the pathways leading to AKI and be prepared for early diagnosis and treatment intervention of established AKI. Recently, artificial intelligence (AI) has provided more advent predictive models for early detection/prediction of AKI utilizing machine learning (ML). By providing strong detail and evidence from risk scores and electronic alerts, this review outlines a comprehensive and holistic insight into the current state of AI in AKI in pediatric/neonatal patients. In the pediatric population, AI models including XGBoost, logistic regression, support vector machines, decision trees, naïve Bayes, and risk stratification scores (Renal Angina Index (RAI), Nephrotoxic Injury Negated by Just-in-time Action (NINJA)) have shown success in predicting AKI using variables like serum creatinine, urine output, and electronic health record (EHR) alerts. Similarly, in the neonatal population, using the “Baby NINJA” model showed a decrease in nephrotoxic medication exposure by 42%, the rate of AKI by 78%, and the number of days with AKI by 68%. Furthermore, the “STARZ” risk stratification AI model showed a predictive ability of AKI within 7 days of NICU admission of AUC 0.93 and AUC of 0.96 in the validation and derivation cohorts, respectively. Many studies have reported the superiority of using biomarkers to predict AKI in pediatric patients and neonates as well. Future directions include the application of AI along with biomarkers (NGAL, CysC, OPN, IL-18, B2M, etc.) in a Labelbox configuration to create a more robust and accurate model for predicting and detecting pediatric/neonatal AKI.






Similar content being viewed by others
References
Sethi SK, Bunchman T, Chakraborty R, Raina R (2021) Pediatric acute kidney injury: new advances in the last decade. Kidney Res Clin Pract 40:40–51. https://doi.org/10.23876/j.krcp.20.074
Kellum JA, Prowle JR (2018) Paradigms of acute kidney injury in the intensive care setting. Nat Rev Nephrol 14:217–230. https://doi.org/10.1038/nrneph.2017.184
Meena J, Mathew G, Kumar J, Chanchlani R (2023) Incidence of acute kidney injury in hospitalized children: a meta-analysis. Pediatrics 151:e2022058823. https://doi.org/10.1542/peds.2022-058823
Jetton JG, Boohaker LJ, Sethi SK et al (2017) Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health 1:184–194. https://doi.org/10.1016/S2352-4642(17)30069-X
Starr MC, Charlton JR, Guillet R et al (2021) Advances in neonatal acute kidney injury. Pediatrics 148:e2021051220. https://doi.org/10.1542/peds.2021-051220
Hu Q, Li S-J, Chen Q-L et al (2021) Risk factors for acute kidney injury in critically ill neonates: a systematic review and meta-analysis. Front Pediatr 9:666507. https://doi.org/10.3389/fped.2021.666507
Agrawal G, Wazir S, Sethi SK et al (2021) Incidence, risk factors, and outcomes of neonatal acute kidney injury: protocol of a multicentric prospective cohort study [The Indian Iconic Neonatal Kidney Educational Registry]. Front Pediatr 9:690559. https://doi.org/10.3389/fped.2021.690559
Charlton JR, Boohaker L, Askenazi D et al (2019) Incidence and risk factors of early onset neonatal AKI. Clin J Am Soc Nephrol 14:184–195. https://doi.org/10.2215/CJN.03670318
Uber AM, Sutherland SM (2020) Acute kidney injury in hospitalized children: consequences and outcomes. Pediatr Nephrol 35:213–220. https://doi.org/10.1007/s00467-018-4128-7
Lewington AJP, Cerdá J, Mehta RL (2013) Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int 84:457–467. https://doi.org/10.1038/ki.2013.153
Pollack MM, Holubkov R, Funai T et al (2016) The Pediatric Risk of Mortality Score: Update 2015. Pediatr Crit Care Med 17:2–9. https://doi.org/10.1097/PCC.0000000000000558
Straney L, Clements A, Parslow RC et al (2013) Paediatric Index of Mortality 3: an updated model for predicting mortality in pediatric intensive care*. Pediatr Crit Care Med 14:673–681. https://doi.org/10.1097/PCC.0b013e31829760cf
for the PIM Study Group, Slater A, Shann F, Pearson G (2003) PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med 29:278–285. https://doi.org/10.1007/s00134-002-1601-2
Slater A, Shann F (2004) The suitability of the Pediatric Index of Mortality (PIM), PIM2, the Pediatric Risk of Mortality (PRISM), and PRISM III for monitoring the quality of pediatric intensive care in Australia and New Zealand: Pediatr Crit Care Med 5:447–453. https://doi.org/10.1097/01.PCC.0000138557.31831.65
Richardson DK, Corcoran JD, Escobar GJ, Lee SK (2001) SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr 138:92–100. https://doi.org/10.1067/mpd.2001.109608
Lee S, Aziz K, Dunn M et al (2012) Transport Risk Index of Physiologic Stability, version II (TRIPS-II): a simple and practical neonatal illness severity score. Am J Perinatol 30:395–400. https://doi.org/10.1055/s-0032-1326983
Parry G, Tucker J, Tarnow-Mordi W (2003) CRIB II: an update of the clinical risk index for babies score. Lancet 361:1789–1791. https://doi.org/10.1016/S0140-6736(03)13397-1
Rosenberg RE, Ahmed S, Saha SK et al (2008) Simplified age-weight mortality risk classification for very low birth weight infants in low-resource settings. J Pediatr 153:519-524.e3. https://doi.org/10.1016/j.jpeds.2008.04.051
Wazir S, Sethi SK, Agarwal G et al (2022) Neonatal acute kidney injury risk stratification score: STARZ study. Pediatr Res 91:1141–1148. https://doi.org/10.1038/s41390-021-01573-9
Kelly CJ, Karthikesalingam A, Suleyman M et al (2019) Key challenges for delivering clinical impact with artificial intelligence. BMC Med 17:195. https://doi.org/10.1186/s12916-019-1426-2
Buch VH, Ahmed I, Maruthappu M (2018) Artificial intelligence in medicine: current trends and future possibilities. Br J Gen Pract 68:143–144. https://doi.org/10.3399/bjgp18X695213
Hamet P, Tremblay J (2017) Artificial intelligence in medicine. Metabolism 69:S36–S40. https://doi.org/10.1016/j.metabol.2017.01.011
Ranganathan P, Pramesh CS, Aggarwal R (2017) Common pitfalls in statistical analysis: logistic regression. Perspect Clin Res 8:148–151. https://doi.org/10.4103/picr.PICR_87_17
LeCun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521:436–444. https://doi.org/10.1038/nature14539
Lee J-G, Jun S, Cho Y-W et al (2017) Deep learning in medical imaging: general overview. Korean J Radiol 18:570. https://doi.org/10.3348/kjr.2017.18.4.570
Khwaja A (2012) KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 120:c179–c184. https://doi.org/10.1159/000339789
Sutherland SM, Goldstein SL, Bagshaw SM (2018) Acute kidney injury and big data. Contrib Nephrol 193:55–67. https://doi.org/10.1159/000484963
Alfieri F, Ancona A, Tripepi G et al (2022) External validation of a deep-learning model to predict severe acute kidney injury based on urine output changes in critically ill patients. J Nephrol 35:2047–2056. https://doi.org/10.1007/s40620-022-01335-8
Gottlieb ER, Samuel M, Bonventre JV et al (2022) Machine learning for acute kidney injury prediction in the intensive care unit. Adv Chronic Kidney Dis 29:431–438. https://doi.org/10.1053/j.ackd.2022.06.005
Liu WT, Liu XQ, Jiang TT et al (2022) Using a machine learning model to predict the development of acute kidney injury in patients with heart failure. Front Cardiovasc Med 9:911987. https://doi.org/10.3389/fcvm.2022.911987
Hoste EAJ, Kellum JA, Selby NM et al (2018) Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol 14:607–625. https://doi.org/10.1038/s41581-018-0052-0
Collins GS, Reitsma JB, Altman DG, Moons KGM (2015) Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med 162:55–63. https://doi.org/10.7326/M14-0697
Kate RJ, Perez RM, Mazumdar D et al (2016) Prediction and detection models for acute kidney injury in hospitalized older adults. BMC Med Inform Decis Mak 16:39. https://doi.org/10.1186/s12911-016-0277-4
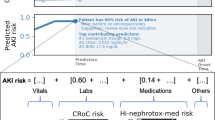
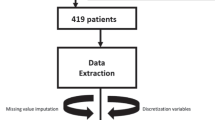
Dong J, Feng T, Thapa-Chhetry B et al (2021) Machine learning model for early prediction of acute kidney injury (AKI) in pediatric critical care. Crit Care 25:288. https://doi.org/10.1186/s13054-021-03724-0
Tomašev N, Glorot X, Rae JW et al (2019) A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 572:116–119. https://doi.org/10.1038/s41586-019-1390-1
Deng Y-H, Luo X-Q, Yan P et al (2022) Outcome prediction for acute kidney injury among hospitalized children via eXtreme Gradient Boosting algorithm. Sci Rep 12:8956. https://doi.org/10.1038/s41598-022-13152-x
Hayward A, Robertson A, Thiruchelvam T et al (2023) Oxygen delivery in pediatric cardiac surgery and its association with acute kidney injury using machine learning. J Thorac Cardiovasc Surg 165:1505–1516. https://doi.org/10.1016/j.jtcvs.2022.05.039
Zeng X, Shi S, Sun Y et al (2022) A time-aware attention model for prediction of acute kidney injury after pediatric cardiac surgery. J Am Med Inform Assoc 30:94–102. https://doi.org/10.1093/jamia/ocac202
Ribeiro-Mourão F, Vaz AC, Azevedo A et al (2021) Assessment of the renal angina index for the prediction of acute kidney injury in patients admitted to a European pediatric intensive care unit. Pediatr Nephrol 36:3993–4001. https://doi.org/10.1007/s00467-021-05116-6
Basu RK, Zappitelli M, Brunner L et al (2014) Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int 85:659–667. https://doi.org/10.1038/ki.2013.349
Basu RK, Kaddourah A, Goldstein SL, AWARE Study Investigators (2018) Assessment of a renal angina index for prediction of severe acute kidney injury in critically ill children: a multicentre, multinational, prospective observational study. Lancet Child Adolesc Health 2:112–120. https://doi.org/10.1016/S2352-4642(17)30181-5
Suárez MDP, Fernández-Sarmiento J, González LE et al (2023) Evaluation of the renal angina index to predict the development of acute kidney injury in children with sepsis who live in middle-income countries. Pediatr Emerg Care. https://doi.org/10.1097/PEC.0000000000002951
McMahon BA, Chawla LS (2021) The furosemide stress test: current use and future potential. Ren Fail 43:830–839. https://doi.org/10.1080/0886022X.2021.1906701
Newton ES, Kurzen EA, Linnemann RW, Shin HS (2021) Use of the NINJA (Nephrotoxic Injury Negated by Just-in-Time Action) program to identify nephrotoxicity in pediatric patients with cystic fibrosis. J Pediatr Pharmacol Ther 26:379–383. https://doi.org/10.5863/1551-6776-26.4.379
Nguyen ED, Menon S (2021) For whom the bell tolls: acute kidney injury and electronic alerts for the pediatric nephrologist. Front Pediatr 9:628096. https://doi.org/10.3389/fped.2021.628096
Koralkar R, Ambalavanan N, Levitan EB et al (2011) Acute kidney injury reduces survival in very low birth weight infants. Pediatr Res 69:354–358. https://doi.org/10.1203/PDR.0b013e31820b95ca
Wu Y, Wang H, Pei J et al (2022) Acute kidney injury in premature and low birth weight neonates: a systematic review and meta-analysis. Pediatr Nephrol 37:275–287. https://doi.org/10.1007/s00467-021-05251-0
Askenazi DJ, Heagerty PJ, Schmicker RH et al (2020) Prevalence of acute kidney injury (AKI) in extremely low gestational age neonates (ELGAN). Pediatr Nephrol 35:1737–1748. https://doi.org/10.1007/s00467-020-04563-x
Saint-Faust M, Boubred F, Simeoni U (2014) Renal development and neonatal adaptation. Am J Perinatol 31:773–780. https://doi.org/10.1055/s-0033-1361831
Hankins G (2002) Neonatal organ system injury in acute birth asphyxia sufficient to result in neonatal encephalopathy. Obstet Gynecol 99:688–691. https://doi.org/10.1016/S0029-7844(02)01959-2
Gupta C, Massaro AN, Ray PE (2016) A new approach to define acute kidney injury in term newborns with hypoxic ischemic encephalopathy. Pediatr Nephrol 31:1167–1178. https://doi.org/10.1007/s00467-016-3317-5
Bozkurt O, Yucesoy E (2021) Acute kidney injury in neonates with perinatal asphyxia receiving therapeutic hypothermia. Am J Perinatol 38:922–929. https://doi.org/10.1055/s-0039-1701024
Van Den Eynde J, Rotbi H, Gewillig M et al (2021) In-hospital outcomes of acute kidney injury after pediatric cardiac surgery: a meta-analysis. Front Pediatr 9:733744. https://doi.org/10.3389/fped.2021.733744
Alten JA, Cooper DS, Blinder JJ et al (2021) Epidemiology of acute kidney injury after neonatal cardiac surgery: a report from the multicenter neonatal and pediatric heart and renal outcomes network. Crit Care Med 49:e941–e951. https://doi.org/10.1097/CCM.0000000000005165
Mohamed TH, Abdi HH, Magers J et al (2022) Nephrotoxic medications and associated acute kidney injury in hospitalized neonates. J Nephrol 35:1679–1687. https://doi.org/10.1007/s40620-022-01264-6
Salerno SN, Liao Y, Jackson W et al (2021) Association between nephrotoxic drug combinations and acute kidney injury in the neonatal intensive care unit. J Pediatr 228:213–219. https://doi.org/10.1016/j.jpeds.2020.08.035
Rhone ET, Carmody JB, Swanson JR, Charlton JR (2014) Nephrotoxic medication exposure in very low birth weight infants. J Matern Fetal Neonatal Med 27:1485–1490. https://doi.org/10.3109/14767058.2013.860522
Stoops C, Stone S, Evans E et al (2019) Baby NINJA (Nephrotoxic Injury Negated by Just-in-Time Action): reduction of nephrotoxic medication-associated acute kidney injury in the neonatal intensive care unit. J Pediatr 215:223-228.e6. https://doi.org/10.1016/j.jpeds.2019.08.046
Sethi SK, Raina R, Rana A et al (2022) Validation of the STARZ neonatal acute kidney injury risk stratification score. Pediatr Nephrol 37:1923–1932. https://doi.org/10.1007/s00467-021-05369-1
Dhooria GS, Nautiyal A, Wazir S et al (2022) Validation of the STARZ neonatal acute kidney injury risk stratification score in an independent prospective cohort. J Neonatal Perinatal Med 15:777–785. https://doi.org/10.3233/NPM-221044
Sethi SK, Raina R, Wazir S et al (2022) STARZ neonatal AKI risk stratification cut-off scores for severe AKI and need for dialysis in neonates. Kidney Int Rep 7:2108–2111. https://doi.org/10.1016/j.ekir.2022.06.020
Yildiz N, Erguven M, Yildiz M et al (2013) Acute peritoneal dialysis in neonates with acute kidney injury and hypernatremic dehydration. Perit Dial Int 33:290–296. https://doi.org/10.3747/pdi.2011.00211
Osswald H, Schnermann J (2011) Methylxanthines and the kidney. Methylxanthines. Springer, Berlin Heidelberg, Berlin, Heidelberg, pp 391–412
Bhatt GC, Gogia P, Bitzan M, Das RR (2019) Theophylline and aminophylline for prevention of acute kidney injury in neonates and children: a systematic review. Arch Dis Child 104:670–679. https://doi.org/10.1136/archdischild-2018-315805
Jetton JG, Guillet R, Askenazi DJ et al (2016) Assessment of worldwide acute kidney injury epidemiology in neonates: design of a retrospective cohort study. Front Pediatr 4:68. https://doi.org/10.3389/fped.2016.00068
Luft FC (2021) Biomarkers and predicting acute kidney injury. Acta Physiol 231:e13479. https://doi.org/10.1111/apha.13479
Bazargani B, Moghtaderi M (2022) New biomarkers in early diagnosis of acute kidney injury in children. Avicenna J Med Biotechnol 14:264–269. https://doi.org/10.18502/ajmb.v14i4.10478
Mishra J, Dent C, Tarabishi R et al (2005) Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet 365:1231–1238. https://doi.org/10.1016/S0140-6736(05)74811-X
Baumert M, Surmiak P, Więcek A, Walencka Z (2017) Serum NGAL and copeptin levels as predictors of acute kidney injury in asphyxiated neonates. Clin Exp Nephrol 21:658–664. https://doi.org/10.1007/s10157-016-1320-6
Sarafidis K, Tsepkentzi E, Diamanti E et al (2014) Urine neutrophil gelatinase-associated lipocalin to predict acute kidney injury in preterm neonates. A pilot study. Pediatr Nephrol 29:305–310. https://doi.org/10.1007/s00467-013-2613-6
Smertka M, Wroblewska J, Suchojad A et al (2014) Serum and urinary NGAL in septic newborns. BioMed Res Int 2014:717318. https://doi.org/10.1155/2014/717318
Sarafidis K, Tsepkentzi E, Agakidou E et al (2012) Serum and urine acute kidney injury biomarkers in asphyxiated neonates. Pediatr Nephrol 27:1575–1582. https://doi.org/10.1007/s00467-012-2162-4
Nakashima T, Inoue H, Fujiyoshi J, Matsumoto N (2016) Longitudinal analysis of serum cystatin C for estimating the glomerular filtration rate in preterm infants. Pediatr Nephrol 31:983–989. https://doi.org/10.1007/s00467-015-3309-x
Washburn KK, Zappitelli M, Arikan AA et al (2007) Urinary interleukin-18 is an acute kidney injury biomarker in critically ill children. Nephrol Dial Transplant 23:566–572. https://doi.org/10.1093/ndt/gfm638
Li Y, Fu C, Zhou X et al (2012) Urine interleukin-18 and cystatin-C as biomarkers of acute kidney injury in critically ill neonates. Pediatr Nephrol 27:851–860. https://doi.org/10.1007/s00467-011-2072-x
Cao X-Y, Zhang H-R, Zhang W, Chen B (2016) Diagnostic values of urinary netrin-1 and kidney injury molecule-1 for acute kidney injury induced by neonatal asphyxia. Zhongguo Dang Dai Er Ke Za Zhi 18:24–28. https://doi.org/10.7499/j.issn.1008-8830.2016.01.006
Askenazi DJ, Montesanti A, Hunley H et al (2011) Urine biomarkers predict acute kidney injury and mortality in very low birth weight infants. J Pediatr 159:907-912.e1. https://doi.org/10.1016/j.jpeds.2011.05.045
Chen J, Sun Y, Wang S et al (2020) The effectiveness of urinary TIMP-2 and IGFBP-7 in predicting acute kidney injury in critically ill neonates. Pediatr Res 87:1052–1059. https://doi.org/10.1038/s41390-019-0698-8
Zhang Y, Zhang B, Wang D et al (2020) Evaluation of novel biomarkers for early diagnosis of acute kidney injury in asphyxiated full-term newborns: a case-control study. Med Princ Pract 29:285–291. https://doi.org/10.1159/000503555
Jalali SZ, Enteshari M, Saadat F (2022) Reciprocal assessment of urinary beta-2-microglobulin and BUN levels in renal dysfunction of neonates with birth asphyxia. J Matern Fetal Neonatal Med 35:6624–6630. https://doi.org/10.1080/14767058.2021.1918667
Abdullah, Kadam P, Yachha M et al (2022) Urinary beta-2 microglobulin as an early predictive biomarker of acute kidney injury in neonates with perinatal asphyxia. Eur J Pediatr 181:281–286. https://doi.org/10.1007/s00431-021-04205-w
Krawczeski CD, Woo JG, Wang Y et al (2011) Neutrophil gelatinase-associated lipocalin concentrations predict development of acute kidney injury in neonates and children after cardiopulmonary bypass. J Pediatr 158:1009-1015.e1. https://doi.org/10.1016/j.jpeds.2010.12.057
Hidayati EL, Utami MD, Rohsiswatmo R, Tridjaja B (2021) Cystatin C compared to serum creatinine as a marker of acute kidney injury in critically ill neonates. Pediatr Nephrol 36:181–186. https://doi.org/10.1007/s00467-020-04668-3
Yang H, Lin C, Zhuang C et al (2022) Serum Cystatin C as a predictor of acute kidney injury in neonates: a meta-analysis. J Pediatr (Rio J) 98:230–240. https://doi.org/10.1016/j.jped.2021.08.005
Kuo J, Akison LK, Chatfield MD et al (2022) Serum and urinary biomarkers to predict acute kidney injury in premature infants: a systematic review and meta-analysis of diagnostic accuracy. J Nephrol 35:2001–2014. https://doi.org/10.1007/s40620-022-01307-y
Ramgopal S, Sanchez-Pinto LN, Horvat CM et al (2023) Artificial intelligence-based clinical decision support in pediatrics. Pediatr Res 93:334–341. https://doi.org/10.1038/s41390-022-02226-1
Coleman C, Tambay Perez A, Selewski DT, Steflik HJ (2022) Neonatal acute kidney injury. Front Pediatr 10:842544. https://doi.org/10.3389/fped.2022.842544
Hu C, Tan Q, Zhang Q et al (2022) Application of interpretable machine learning for early prediction of prognosis in acute kidney injury. Comput Struct Biotechnol J 20:2861–2870. https://doi.org/10.1016/j.csbj.2022.06.003
Menon S, Goldstein SL, Mottes T et al (2016) Urinary biomarker incorporation into the renal angina index early in intensive care unit admission optimizes acute kidney injury prediction in critically ill children: a prospective cohort study. Nephrol Dial Transplant 31:586–594. https://doi.org/10.1093/ndt/gfv457
Cirillo D, Catuara-Solarz S, Morey C et al (2020) Sex and gender differences and biases in artificial intelligence for biomedicine and healthcare. NPJ Digit Med 3:81. https://doi.org/10.1038/s41746-020-0288-5
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Authors Rupesh Raina and Arwa Nada are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Raina, R., Nada, A., Shah, R. et al. Artificial intelligence in early detection and prediction of pediatric/neonatal acute kidney injury: current status and future directions. Pediatr Nephrol (2023). https://doi.org/10.1007/s00467-023-06191-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00467-023-06191-7