Abstract
Background
A substantial proportion of patients with Escherichia coli-hemolytic uremic syndrome (STEC-HUS) evolve to chronic kidney disease (CKD). The objectives of this study were to evaluate long-term kidney outcomes and to identify CKD predictors.
Methods
In this single-center retrospective study, long-term outcomes of patients were analyzed according to the presence of complete recovery (CR) or CKD at last visit. Then, they were grouped into favorable (CR + CKD1) or poor (CKD2–5) outcome to compare predictors at diagnosis (sex, age, leukocytes, creatinine, hemoglobin, HUS severity score), dialysis duration, and follow-up time between them.
Results
Of 281 patients followed up for a median of 12 years, 139 (49%) had CR, 104 (37%) CKD1, 27 (10%) CKD2–4, and 11 (4%) CKD5. Thirty-eight patients progressed to CKD2–5 after a median of 4.8 years, 7% in the first 5 years, increasing to 8%, 10%, and 14% after 5–10 years, 10–15 years, and > 15 years, respectively. They were younger, had higher baseline hemoglobin and leukocytes, and required longer dialysis and follow-up than those with favorable outcome. By multivariate analysis, days of dialysis and follow-up time remained as independent predictors of poor outcome. The best cutoff for days of dialysis was 10 days. After 5 years, 20% of those dialyzed ≥ 10 days evolved to CKD2–5 versus 1% of those non-dialyzed or dialyzed < 10 days.
Conclusions
Fifty-one percent of patients evolved to CKD after 12 years of follow-up and 14% to CKD2–5. Ten days of dialysis was the best cutoff to recognize outcomes. In some cases, kidney damage was evident after 15 years of surveillance, highlighting the need for follow-up until adulthood in all STEC-HUS patients.
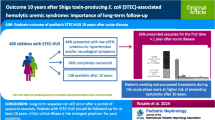
Graphical Abstract

A higher resolution version of the Graphical abstract is available as Supplementary information




Similar content being viewed by others
Data Availability
The data are available from the corresponding author on reasonable request
References
Balestracci A, Meni Battaglia L, Toledo I, Martin SM, Puyol I, Beaudoin L, Robledo NL (2021) Diagnostic sensitivity of extended renal and hematologic criteria to define hemolytic uremic syndrome. Arch Argent Pediatr 119:238–244. https://doi.org/10.5546/aap.2021.eng.238
Alconcher LF, Balestracci A, Coccia PA, Suarez ADC, Ramírez FB, Monteverde ML, Perez Y Gutiérrez MG, Carlopio PM, Principi I, Estrella P, Micelli S, Leroy DC, Quijada NE, Seminara C, Giordano MI, Hidalgo Solís SB, Saurit M, Caminitti A, Arias A, Liern M, Rivas M (2021) Hemolytic uremic syndrome associated with Shiga toxin-producing Escherichia coli infection in Argentina: update of serotypes and genotypes and their relationship with severity of the disease. Pediatr Nephrol 36:2811–2817. https://doi.org/10.1007/s00467-021-04988-y
Alconcher LF, Coccia PA, Suarez ADC, Monteverde ML, Perez Y, Gutiérrez MG, Carlopio PM, Missoni ML, Balestracci A, Principi I, Ramírez FB, Estrella P, Micelli S, Leroy DC, Quijada NE, Seminara C, Giordano MI, Hidalgo Solís SB, Saurit M, Caminitti A, Arias A, Rivas M, Risso P, Liern M (2018) Hyponatremia: a new predictor of mortality in patients with Shiga toxin-producing Escherichia coli hemolytic uremic syndrome. Pediatr Nephrol 33:1791–1798. https://doi.org/10.1007/s00467-018-3991-6
Mody RK, Gu W, Griffin PM, Jones TF, Rounds J, Shiferaw B, Tobin-D’Angelo M, Smith G, Spina N, Hurd S, Lathrop S, Palmer A, Boothe E, Luna-Gierke RE, Hoekstra RM (2015) Postdiarrheal hemolytic uremic syndrome in United States children: clinical spectrum and predictors of in-hospital death. J Pediatr 166:1022–1029. https://doi.org/10.1016/j.jpeds.2014.12.064
Grisaru S, Morgunov MA, Samuel SM, Midgley JP, Wade AW, Tee JB, Hamiwka LA (2011) Acute renal replacement therapy in children with diarrhea-associated hemolytic uremic syndrome: a single center 16 years of experience. Int J Nephrol 2011:930539. https://doi.org/10.4061/2011/930539
National System of Procurement and Transplant Information of the Argentine Republic. Report of patients registered on the waiting list. Available from: http://www.sintra.incucai.gov.ar. Accessed 1 July 2017
Spizzirri FD, Rahman RC, Bibiloni N, Ruscasso JD, Amoreo OR (1997) Childhood hemolytic uremic syndrome in Argentina: long-term follow-up and prognostic features. Pediatr Nephrol 11:156–160. https://doi.org/10.1007/s004670050248
Siegler RL, Milligan MK, Burningham TH, Christofferson RD, Chang SY, Jorde LB (1991) Long-term outcome and prognostic indicators in the hemolytic-uremic syndrome. J Pediatr 118:195–200. https://doi.org/10.1016/s0022-3476(05)80482-2
Fitzpatrick MM, Shah V, Trompeter RS, Dillon MJ, Barratt TM (1991) Long term renal outcome of childhood haemolytic uraemic syndrome. BMJ 303:489–492. https://doi.org/10.1136/bmj.303.6801.489
Gagnadoux MF, Habib R, Gubler MC, Bacri JL, Broyer M (1996) Long-term (15–25 years) outcome of childhood hemolytic-uremic syndrome. Clin Nephrol 46:39–41
Spinale JM, Ruebner RL, Copelovitch L, Kaplan BS (2013) Long-term outcomes of Shiga toxin hemolytic uremic syndrome. Pediatr Nephrol 28:2097–2105. https://doi.org/10.1007/s00467-012-2383-6
Oakes RS, Kirkham JK, Nelson RD, Siegler RL (2008) Duration of oliguria and anuria as predictors of chronic renal-related sequelae in post-diarrheal hemolytic uremic syndrome. Pediatr Nephrol 23:1303–1308. https://doi.org/10.1007/s00467-008-0799
Alconcher LF, Lucarelli LI, Bronfen S (2023) Long-term kidney outcomes in non-dialyzed children with Shiga-toxin Escherichia coli associated hemolytic uremic syndrome. Pediatr Nephrol 38:2131–2136. https://doi.org/10.1007/s00467-022-05851-4
Ardissino G, Tel F, Testa S, Paglialonga F, Longhi S, Martelli L, Consolo S, Picicco D, Dodaro A, Daprai L, Colombo R, Arghittu M, Perrone M, Chidini G, Scalia Catenacci S, Cropanese I, Consonni D; ItalKid-HUS Network (2018) A simple prognostic index for Shigatoxin-related hemolytic uremic syndrome at onset: data from the ItalKid-HUS network. Eur J Pediatr 177:1667–1674. https://doi.org/10.1007/s00431-018-3198-7
Loos S, Oh J, van de Loo L, Kemper MJ, Blohm M, Schild R (2021) Hemoconcentration and predictors in Shiga toxin-producing E. coli-hemolytic uremic syndrome (STEC-HUS). Pediatr Nephrol 36:3777–3783. https://doi.org/10.1007/s00467-021-05108-6
Ardissino G, Possenti I, Tel F, Testa S, Paglialonga F (2014) Time to change the definition of hemolytic uremic syndrome. Eur J Intern Med 25:e29. https://doi.org/10.1016/j.ejim.2013.12.002
Coccia P, Ramírez F, Suárez A, Alconcher L, Balestracci A et al (2021) Acute peritoneal dialysis, complications and outcomes in 389 children with STEC-HUS: a multicenter experience. Pediatr Nephrol 36:1597–1606. https://doi.org/10.1007/s00467-020-04876-x
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263. https://doi.org/10.1542/peds.58.2.259
Hogg RJ, Furth S, Lemley KV, Portman R, Schwartz GJ, Coresh J, Balk E, Lau J, Levin A, Kausz AT, Eknoyan G, Levey AS; National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (2003) National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics 111:1416–1421. https://doi.org/10.1542/peds.111.6.1416
Cubillos CMP, Del Salas P, Zambrano PO (2015) Microalbuminuria in pediatric patients diagnosed with hemolytic uremic syndrome. Rev Chil Pediatr 86:92–96. https://doi.org/10.1016/j.rchipe.2015.04.019
Flynn JT, Kaelber DC, Baker-Smith CM, Subcommittee on Screening and Management of High Blood Pressure in Children et al (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140:e20171904. https://doi.org/10.1542/peds.2017-3035
KDIGO CKD Work Group (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1–150 (https://www.kisupplements.org/article/S2157-1716(16)30005-3/fulltext)
VanSickle JS, Srivastava T, Alon US (2018) Risk factors for short- and long-term outcomes in children with STEC-HUS/D+ HUS: a single-center experience. Glob Pediatr Health 5:2333794X18816920. https://doi.org/10.1177/2333794X18816920
Robitaille P, Clermont MJ, Mérouani A, Phan V, Lapeyraque AL (2012) Hemolytic uremic syndrome: late renal injury and changing incidence-a single centre experience in Canada. Scientifica (Cairo) 2012:341860. https://doi.org/10.6064/2012/341860
Monet-Didailler C, Godron-Dubrasquet A, Madden I, Delmas Y, Llanas B, Harambat J (2019) Long-term outcome of diarrhea-associated hemolytic uremic syndrome is poorly related to markers of kidney injury at 1-year follow-up in a population-based cohort. Pediatr Nephrol 34:657–662. https://doi.org/10.1007/s00467-018-4131-z
Rosales A, Hofer J, Zimmerhackl LB, Jungraithmayr TC, Riedl M, Giner T, Strasak A, Orth-Höller D, Würzner R, Karch H, German-Austrian HUS Study Group (2012) Need for long-term follow-up in enterohemorrhagic Escherichia coli-associated hemolytic uremic syndrome due to late-emerging sequelae. Clin Infect Dis 54:1413–1421. https://doi.org/10.1093/cid/cis196
Lou-Meda R, Oakes RS, Gilstrap JN, Williams CG, Siegler RL (2007) Prognostic significance of microalbuminuria in postdiarrheal hemolytic uremic syndrome. Pediatr Nephrol 22:117–120. https://doi.org/10.1007/s00467-006-0283-3
Caletti MG, Missoni M, Vezzani C, Grignoli M, Piantanida JJ, Repetto HA, Exeni R, Rasse SM (2011) Effect of diet, enalapril, or losartan in post-diarrheal hemolytic uremic syndrome nephropathy. Pediatr Nephrol 26:1247–1254. https://doi.org/10.1007/s00467-011-1867-0
Caletti MG, Balestracci A, Missoni M, Vezzani C (2013) Additive antiproteinuric effect of enalapril and losartan in children with hemolytic uremic syndrome. Pediatr Nephrol 28:745–750. https://doi.org/10.1007/s00467-012-2374-7
Pundzienė B, Dobilienė D, Čerkauskienė R, Mitkienė R, Medzevičienė A, Darškuvienė E, Jankauskienė A (2015) Long-term follow-up of children with typical hemolytic uremic syndrome. Medicina 51:146–151. https://doi.org/10.1016/j.medici.2015.06.004
Repetto HA (2005) Long-term course and mechanisms of progression of renal disease in hemolytic uremic syndrome. Kidney Int 97:S102–S106. https://doi.org/10.1111/j.1523-1755.2005.09717.x
Monteverde ML, Panero N, Chaparro AB, Locane F, Sarkis C, Mattio SA, Ibañez JP (2023) A decrease in the incidence of Shiga toxin-related hemolytic uremic syndrome as a cause of kidney transplantation at an argentine referral center. Pediatr Transplant 27:e14489. https://doi.org/10.1111/petr.14489
Ardissino G, Testa S, Daccò V, Paglialonga F, Viganò S, Felice-Civitillo C, Battaglino F, Bettinelli A, Bordugo A, Cecchetti V, De Pascale S, La Manna A, Li Volti S, Maringhini S, Montini G, Pennesi M, Peratoner L (2012) Puberty is associated with increased deterioration of renal function in patients with CKD: data from the ItalKid Project. Arch Dis Child 97:885–888. https://doi.org/10.1136/archdischild-2011-300685
Vaterodt L, Holle J, Hüseman D, Müller D, Thumfart J (2018) Short- and long-term renal outcome of hemolytic-uremic syndrome in childhood. Front Pediatr 6:220. https://doi.org/10.3389/fped.2018.00220
Cobeñas CJ, Alconcher LF, Spizzirri AP, Rahman RC (2007) Long-term follow-up of Argentinean patients with hemolytic uremic syndrome who had not undergone dialysis. Pediatr Nephrol 22:1343–1347. https://doi.org/10.1007/s00467-007-0522-2
Acknowledgements
The authors gratefully acknowledge the assistance of Alejandro Balestracci, MD Ph.D., for his valuable observations during the preparation of this paper and María Eugenia Elorza, Ph.D. in Economics, for the statistical analysis done at Universidad Nacional del Sur.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is an observational, retrospective study. The Review Boards and Ethics Committees approved this study. The requirement to obtain informed consent was waived by the institutional review boards.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alconcher, L.F., Lucarelli, L.I., Bronfen, S. et al. Kidney sequelae in 281 Shiga toxin–producing Escherichia coli-hemolytic uremic syndrome patients after a median follow-up of 12 years. Pediatr Nephrol 39, 1221–1228 (2024). https://doi.org/10.1007/s00467-023-06183-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06183-7