Abstract
In 2018, the Emergency, Disasters and Ambulatory Transportation General Department at the Ministry of Health in Saudi Arabia established hospital emergency planning and preparation units (HEPPUs) to improve hospitals’ ability to respond to disasters. This study aimed to gain an in-depth understanding of the functioning of HEPPUs within hospitals in the western region of Saudi Arabia. Qualitative research methodology and semistructured interviews with emergency managers were employed. Four key themes emerged from the data: establishment and evolution, roles and responsibilities, communication and coordination, and challenges and limitations. The findings emphasize the importance of interdisciplinary collaboration, effective communication, and responses to challenges in enhancing healthcare resilience and disaster management. This study contributes insights and offers practical recommendations for improving the preparedness and performance of HEPPUs within Saudi Arabian hospitals.
Similar content being viewed by others
1 Introduction
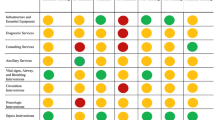
In an era marked by growing uncertainties and the escalating frequency of disasters, both natural and human-made, the critical role of hospitals in disaster planning and preparedness cannot be overstated (Yadav and Barve 2015). As frontline providers of essential healthcare services, hospitals are vital for community resilience during times of crisis (Patel et al. 2017). To respond effectively to a diverse range of scenarios, from mass casualty incidents to infectious disease outbreaks and chemical or radiation hazards, hospitals must adopt a comprehensive and well-coordinated approach to disaster planning and preparedness (Veenema 2018). This multifaceted strategy encompasses infrastructure resilience, resource management, staff training, and collaboration with other stakeholders. Additionally, hospitals must have the capacity to adapt their operations and services to the evolving needs of affected populations, ensuring continuity of care and optimal utilization of resources. At the hospital level, successful disaster management hinges on the resilience of these institutions, which involves implementing various strategies (such as absorbing capacity, buffering capacity, and response capacity) throughout different stages of a disaster, including before the event, during the event, and after the event (Table 1). This comprehensive and robust approach is crucial for addressing potential crises and maintaining the delivery of essential healthcare services.
Pre-event hospital disaster preparedness encompasses risk assessment and hazard vulnerability analysis (HVA), emergency operations planning, and staff training and education, all of which are crucial for effective response and resilience. A risk assessment and an HVA enable hospitals to identify threats, prioritize resources, and develop preparedness measures, addressing risks such as vulnerable patients and limited space (Hu et al. 2017; Al Thobaity et al. 2019; Phuspa et al. 2019). A comprehensive emergency operations plan (EOP) must address critical hospital emergency management components, including a hospital emergency incident command system, collaboration with law enforcement, childcare protocols for staff members’ children, designated overflow areas, command systems, volunteer credentialing policies, multi-agency drills, and resource and space augmentation plans (Kaji and Lewis 2006; Al Thobaity et al. 2019; Ali et al. 2021). Finally, staff training and education should be implemented before a disaster event, acquainting healthcare workers with disaster protocols, communication, and triage, and providing essential knowledge and skills through institutions and medical schools. Regular multidisciplinary training exercises and simulations ensure staff readiness for emergencies and disasters (Khorram-Manesh et al. 2016; Olivieri et al. 2017; Brinjee et al. 2021; Sultan et al. 2023).
During-event preparedness strategies have three major components: a hospital incident command system (HICS), surge capacity, and communication and coordination. An HICS is a management system that streamlines incident handling in unexpected situations and fosters coordination between hospitals and associated institutions, utilizing a structured, integrated approach with clear responsibilities, reporting channels, and simplified terminology (Larson and Raney 2008; Bahrami et al. 2020). This system provides a clear command structure, ensures efficient information flow, and protects patients, staff, and hospital infrastructure during disasters while also playing a role in preparedness through action plans and staff training (Shooshtari et al. 2017). Medical surge preparedness is essential, particularly in disaster-prone countries, as it helps manage sudden influxes of patients with the available resources (Sheikhbardsiri et al. 2017; Marcozzi et al. 2020). Primary evaluation and risk assessment of surge capacity components, including staff, supplies and equipment, physical space, and integrated management policies and processes, are crucial before implementation (Shabanikiya et al. 2019; Hasan et al. 2022). Effective communication and coordination among healthcare providers, emergency management agencies, and other stakeholders are critical during a disaster (Wang et al. 2021). Hospitals should establish communication protocols and employ communication technologies for situational awareness and coordinated response efforts, focusing on clear communication, resource coordination, and crowd control during mass causality incidents (El Sayed et al. 2018; Ali et al. 2021; Wang et al. 2021).
Post-event, known as recovery from a disaster, strategies must plan for recovery and restoration, incorporating after-action reviews and lessons learned as well as ensuring psychological support for healthcare workers. Recovery and restoration planning is a vital yet often overlooked aspect of disaster preparedness, which plays a critical role in maintaining the functionality, safety, and resilience of hospitals as the backbone of health systems (Stoto et al. 2019). To promote resilience and sustainable development, hospitals must engage in multi-sectoral recovery efforts that embrace the “build back better” principle and prioritize efficient, resilient recovery approaches (El Sayed et al. 2018; Ali et al. 2021; Hasan et al. 2022). This includes conducting after-action reviews to evaluate and enhance disaster preparedness, as well as providing psychological support to healthcare workers, who often experience significant stress and psychological trauma during and after a disaster (Brooks et al. 2019; Søvold et al. 2021). By integrating lessons learned, addressing the mental health and well-being of staff, and fostering a supportive environment, hospitals can build stronger, more efficient, and adaptable institutions that effectively manage and recover from various types of disasters while ensuring the continued provision of high-quality care to patients.
In the international literature on hospital planning and preparedness, the importance of effective frameworks, guidelines, and strategies for healthcare systems that respond to various disasters and emergencies is emphasized (Zhong et al. 2014; Bradley et al. 2016; Khorram-Manesh et al. 2016). Researchers have focused on evaluating current disaster management strategies, identifying gaps and challenges, and proposing best practices for enhancing hospital resilience, which encompasses infrastructure resilience, resource management, staff training, and interagency coordination (Aitsi-Selmi and Murray 2015; Olivieri et al. 2017). Cross-national comparisons have revealed shared challenges and unique contextual factors, highlighting the need for flexible, adaptable, and evidence-based approaches to disaster planning and preparedness (Bayram and Zuabi 2012; Chen et al. 2013; Sultan et al. 2023). As global disaster risks continue to evolve, additional research, collaboration, and knowledge-sharing among stakeholders are crucial to refine existing strategies, foster community resilience, and ensure the safety and well-being of populations worldwide.
In Saudi Arabia, the most frequent causes of disasters include accidents, floods, and transportation accidents, followed by industrial accidents, epidemics, and storms (Guha-Sapir et al. 2009). These events highlight the need for targeted preparedness and response strategies that effectively address the specific risks associated with each type of disaster, ensuring the safety and well-being of the population, and strengthening the country’s overall disaster management capabilities. During the Hajj pilgrimage in Saudi Arabia, several tragic incidents involving stampedes and fires have occurred over the years, resulting in a significant loss of life and numerous injuries (Al-Wathinani et al. 2021). Notable events include a fire caused by an exploding gas cylinder in December 1975, which led to the deaths of 200 pilgrims, and a stampede inside the Al-Ma’aism tunnel on 2 July 1990, during which 1426 pilgrims lost their lives. Other incidents include a tent fire in Mina in 1997, which resulted in 343 deaths and 1500 injuries, and multiple stampedes during the stoning of the Devil ritual and at Jamarat Bridge, with the most recent tragedy occurring in Mina on 24 September 2015, causing 769 fatalities and 934 injuries (Al-Wathinani et al. 2021). These events serve as critical reminders of the need for robust safety measures and effective crowd management during the Hajj pilgrimage.
Given the frequency and variety of disasters in Saudi Arabia, including events during the Hajj pilgrimage, it is essential that all hospitals, particularly those in the western cities of Makkah, Jeddah, and Taif, are well prepared to respond to such emergencies. Hospital preparedness in Saudi Arabia faces unique challenges and opportunities because the country’s healthcare system addresses disaster risks, emergencies, and large-scale events, such as the annual Hajj event pilgrimage (Al-Tawfiq and Memish 2014; Al Thobaity et al. 2015; Al Thobaity et al. 2019; Al Harthi et al. 2020; Al Harthi et al. 2021; Alruwaili et al. 2022). Studies have investigated various preparedness aspects, including HICS implementation, staff training and capacity building, and resource management in response to mass casualty incidents, infectious disease outbreaks, and other crises. Additionally, researchers have evaluated the current preparedness state in Saudi hospitals using evaluation tools and frameworks, identifying gaps in knowledge, resources, and coordination, and recommending improvements (Bajow and Alkhalil 2014; Al Thobaity et al. 2016; Khan et al. 2021). These findings emphasize the need for a tailored approach to hospital preparedness in Saudi Arabia, accounting for the nation’s unique sociocultural, economic, and environmental context. In 2018, the Emergency, Disasters and Ambulatory Transportation General Department established the hospital emergency planning and preparation units (HEPPUs) as a procedural guide for hospitals (MOH 2019). Despite its importance, no studies have assessed the awareness of the roles and responsibilities of HEPPUs in Saudi Arabia. It is essential to understand the functioning of these units within hospitals to enhance the resilience of Saudi hospitals and the communities they serve. Therefore, the aim of this study was to gain an in-depth understanding of the functioning of HEPPUs within hospitals in Saudi Arabia.
2 Methods
In this study, a rigorous qualitative research methodology was employed to gain an in-depth understanding of emergency preparedness and response practices in the western region of Saudi Arabia, focusing on three prominent hospitals in Makkah, Jeddah, and Al Taif. Semistructured interviews served as the cornerstone of data collection, enabling researchers to explore the perspectives and experiences of emergency managers and members of emergency preparedness and response committees. Five participants from each hospital were carefully selected, ensuring that data collection continued until saturation was achieved. The inclusion and exclusion criteria for hospitals and participants are listed in Table 2.
After the study received ethical approval from the Research Department in the Directorate of Health Affairs, Makkah region (number H-02-K-076-0522-723) on 23 May 2022, data collection was initiated through personal site visits and in-depth interviews incorporating open- and closed-ended questions. Verbatim transcriptions of participants’ responses were generated and securely stored in a Microsoft Word file on the researcher’s personal computer, organized by interview questions. The semistructured interviews continued until data saturation was achieved, with each session lasting between 30 and 45 min. The interviews were conducted in quiet rooms within the emergency departments of the selected hospitals to ensure an optimal environment for meaningful dialogue. Before the data were collected, the interview questions were rigorously assessed for validity and reliability by experts. The central themes of the interviews revolved around the viability of the HEPPU system in hospitals, its primary functions, collaboration with other disaster response units, contribution to patient care processes, and the challenges faced by HEPPU teams within the hospital setting.
The collected data were meticulously analyzed using thematic analysis, a process that began with the identification of themes, followed by the coding of the interview transcripts. To ensure the confidentiality and protection of participant information, all interview transcripts were securely stored on the researcher’s personal computer. To validate the findings and establish credibility, the original authors and academic experts reviewed the thematic analysis results. This rigorous approach to data analysis not only reinforced the trustworthiness of the results but also provided valuable insights into the complex dynamics of emergency preparedness and response within the sample hospitals.
3 Results
Fifteen participants were interviewed (Table 3). The diverse participants held various positions in the emergency and healthcare sectors. Most were male (14) and Saudi (13); 1 was Palestinian, and 1 was Syrian. The participants’ ages ranged from 26 to 56 years; therefore, they had different levels of experience. The group included emergency department (ED) directors, HEPPU directors, HEPPU team members, paramedics, ED team leaders, ED consultants, ED supervisors, and ED leaders. The two female participants held important positions as ambulance transportation supervisor/member of the HEPPU and as HEPPU director. This composition reflects a wide array of backgrounds and expertise, suggesting a comprehensive understanding of the challenges and opportunities faced by the emergency and healthcare sectors. The analysis of the interviews led to the identification of four themes: establishment and evolution of the HEPPU, roles and responsibilities of the HEPPU, communication and coordination, and challenges and limitations.
3.1 Theme 1: Establishment and Evolution of the Hospital Emergency Planning and Preparation Unit (HEPPU)
The first theme highlights the establishment and evolution of the HEPPU. The interview data revealed that the HEPPU is a relatively new addition to the hospital structure (Table 4). The findings suggest that the hospital had recently recognized the need for a dedicated unit to handle emergency planning and preparedness (P12). The establishment of the HEPPU coincided with the pandemic, which indicates that the pandemic likely served as a catalyst for the creation of the unit, as hospitals realized the importance of having a specialized team to address emergency situations (P9). Before the HEPPU was established, responsibility for emergency planning and preparedness was limited to the nursing department (P9). The expansion of the unit to include all hospital departments signified a more comprehensive and holistic approach to emergency management.
3.2 Theme 2: Roles and Responsibilities of the Hospital Emergency Planning and Preparation Unit (HEPPU)
The second theme focuses on the roles and responsibilities of the HEPPU. The interview data shed light on the various tasks and functions that the unit undertakes to ensure the efficient management of emergencies and disasters within the hospital (Table 5). One of the primary responsibilities is to develop plans for internal and external disasters and determine how to deal with them (P1). These plans include routine and disaster-specific tasks (P2), ensuring that the hospital is well prepared for various emergency scenarios. The HEPPU also plays a significant role in staff training, particularly in evacuating patients and handling internal and external disasters (P3). This training is essential for responding efficiently to emergencies and minimizing potential harm to patients and staff. The unit is responsible for upgrading the readiness of ambulance transportation and implementing rapid response systems inside and outside the facility (P14). This includes collaborating with external organizations, such as the Red Crescent, to implement an air evacuation system (P14). Another critical aspect of the HEPPU’s role is managing the recovery stage following a disaster, ensuring that the hospital can return to normal operations and integrating the results of their response (P2). This includes preparing final reports on disasters or events (P15) to evaluate the effectiveness of the response and inform future planning. The HEPPU plays a crucial role in patient care during disasters. This includes ensuring continuous treatment (P7), receiving new cases without neglecting existing ones (P9), and properly evacuating and distributing patients while maintaining treatment continuity (P10). Training medical teams for specific disaster scenarios, such as radiation disasters, is also an essential responsibility of the unit (P15). Furthermore, the HEPPU strives to maintain the quality of patient care before, during, and after disasters by developing comprehensive evacuation plans and supervising patient evacuations (P2). Finally, the unit has been reported to be effective in educating staff on how to deal with infectious cases (P1), demonstrating the HEPPU’s commitment to enhancing the hospital’s overall competence in managing various emergency situations.
3.3 Theme 3: Communication and Coordination
The third theme highlights the importance of communication and coordination for the HEPPU. The interview data revealed various aspects of communication and coordination within the unit, as well as with external organizations and other hospital departments (Table 6). One participant mentioned that coordination depends on the type of incident or crisis and the necessary procedures for each type (P11). This suggests that the HEPPU’s approach to communication and coordination is adaptive and tailored to the specific emergency situation at hand. The HEPPU also plays a role in providing support to other hospitals or centers, such as providing ambulances for transportation and collaborating with volunteer initiatives during disasters (P15). This demonstrates the unit’s commitment to working with external organizations to ensure a coordinated and efficient response to emergencies. Effective communication within the HEPPU involves coordination with all responsible parties during an event (P12) and using various levels of communication (P2). This includes holding regular meetings, utilizing network communication, and operating through emergency response centers (P13). Additionally, the unit follows up on the readiness for communication using hotline systems or other tools in healthcare areas (P5).
However, some challenges in communication and coordination were also identified in the interviews. One participant mentioned limited knowledge about the unit’s communication, stating that they communicated mainly with the hospital administration (P8). Another participant pointed out that hospitals tend to operate independently and suggested that there needs to be more communication or support between different units (P6). Furthermore, it was noted that crisis management communicates effectively with the hospital through a command room, which is separate from the HEPPU (P9). This separation may contribute to a gap in communication between the emergency planning and preparation unit and other departments or units within the hospital.
3.4 Theme 4: Challenges and Limitations
The fourth theme highlights the various challenges and limitations faced by the HEPPU. The interview data revealed several areas in which the unit had encountered difficulties, including a lack of understanding, staffing issues, approval challenges, and coordinating efforts (Table 7). One significant challenge is the lack of understanding surrounding the unit’s role (P6, P9, and P13). This might be due to the relatively recent establishment of the HEPPU, which has led to some confusion about its existence and functions among other hospital departments (P13). Another issue is the lack of suitable and experienced individuals to work in the unit (P6, P9). This, coupled with staff shortages (P3, P4, and P9), may hinder the unit’s ability to function effectively and efficiently in emergency situations. Staff training challenges also contribute to these limitations (P3).
The HEPPU faces approval challenges, with some participants mentioning that there is no support from the crisis and disaster management department, and plans and drills had not been approved (P7). This lack of support may impede the unit’s ability to develop and implement effective emergency plans. Unclear roles for the unit (P9) and reliance on personal effort (P9) also contribute to the challenges faced by the HEPPU. Additionally, the lack of centralized case coordination within the region leads to insufficient health services for patients (P11). The newness of the unit is another factor leading to staff shortages, with more time and effort needed for everyone to become familiar with the HEPPU (P4). This may contribute to the unclear roles mentioned earlier. Departmental interference in the planning unit and its functions (P15) and insufficient availability of resources, such as decontamination tents (P15), add to these challenges. Furthermore, fragmentation within the system due to institutional transformation (P1) may negatively impact the unit’s efficiency. Finally, unclear roles for employees in the departments and those in the unit (P9), as well as the absence of clear mechanisms and reference points for consultation (P9), contributed to the challenges faced by the unit. This lack of clarity may lead to mistakes during disaster management, some of which could be easily corrected with better guidance (P9).
4 Discussion
In the face of increasing disasters, hospitals play a critical role in disaster planning and preparedness, requiring a comprehensive and well-coordinated approach. To enhance our understanding of the roles and challenges facing Saudi HEPPUs, this study explored four major themes: establishment and evolution of the HEPPU, the roles and responsibilities of the HEPPU, communication and coordination, and challenges and limitations. Strategies include infrastructure resilience, resource management, staff training, and collaboration. Hospitals must be adaptable to address potential crises and maintain essential healthcare services. Key components of preparedness involve pre-event planning, during-event response, and post-event recovery, addressing risk assessment, emergency operations, staff training, incident command systems, surge capacity, communication, coordination, restoration, after-action reviews, and psychological support for healthcare workers. By examining the various facets of the HEPPU, this study sheds light on the importance of these units in enhancing resilience and ensuring effective disaster management across healthcare systems.
The COVID-19 pandemic unquestionably exposed significant weaknesses and vulnerabilities across numerous healthcare systems, thus emphasizing the need for specialized units, such as HEPPUs, to bolster emergency preparedness and response capabilities (Al-Wathinani et al. 2020). The creation of these units emerged as a solution to the growing need for a unified approach to emergency planning and preparedness, ensuring that hospitals and healthcare facilities were better equipped to manage crises and deliver optimal patient care. Although the initial focus of the HEPPU centered on the nursing department, due to the essential role nurses play during emergencies, it became apparent that a broader, more inclusive strategy was needed for effective emergency management (Al Harthi et al. 2021; Abuadas and Albikawi 2022). Consequently, the unit was expanded to include all hospital departments, fostering a coordinated and integrated approach to emergency planning and preparedness across the entire healthcare spectrum. This shift toward a more holistic approach underscores the significance of interdepartmental collaboration in addressing emergencies, allowing HEPPUs to cater to the distinct needs and challenges of each department, ultimately leading to more efficient emergency planning and response efforts (Bayram and Zuabi 2012; Djalali et al. 2015; Hendrickx et al. 2016; Ali et al. 2021). The implications of this study’s findings suggest that fostering such interdisciplinary collaboration is vital for healthcare systems, and recommendations include continued development and support for units such as HEPPUs to enhance preparedness and resilience for future emergencies.
The multifaceted roles and responsibilities of the HEPPU highlight its essential and integral contribution to various facets of emergency management, including pivotal areas such as thorough emergency planning, specialized staff training, exceptional patient care, and efficient recovery management (Al Thobaity et al. 2019; Bahrami et al. 2020). The unit’s all-encompassing approach to addressing emergencies ensures that healthcare facilities remain adept and ready to handle a diverse array of emergency situations (Timbie et al. 2013; Prakash Narain et al. 2021). The HEPPU’s commitment to collaborating with external organizations further bolsters its capacity to deliver prompt and comprehensive emergency responses. The wide range of the unit’s responsibilities, from emergency planning to recovery management, exemplifies the importance of adopting a holistic strategy for emergency preparedness in healthcare settings (Timbie et al. 2013; Prakash Narain et al. 2021). The conclusions drawn from these observations indicate that the versatile nature of HEPPUs is crucial for effectively managing various aspects of emergencies. Thus, it is recommended that healthcare systems prioritize the growth and support of HEPPUs, focusing on fostering interdisciplinary collaboration and an all-encompassing approach to emergency preparedness. By embracing a well-rounded strategy for emergency management, healthcare facilities can strengthen their resilience and capacity to respond rapidly and effectively to diverse emergency situations.
The results underscore the importance of communication and coordination for the HEPPU in navigating emergency scenarios. Although the unit generally exhibits proficiency in collaborating with a diverse array of internal and external stakeholders, some communication hurdles remain. Surmounting these barriers and encouraging increased collaboration among diverse units and organizations is vital to increase the overall efficacy and efficiency of the HEPPU’s emergency response endeavors (Chen et al. 2013; Chirico et al. 2023). The implications derived from these insights indicate that robust communication and coordination are indispensable components of a successful emergency management approach. To further optimize the HEPPU’s performance, it is advised that healthcare systems focus on fine-tuning communication pathways, advocating for transparency, and nurturing a collaborative atmosphere among all participating parties (Chen et al. 2013; Chirico et al. 2023). By tackling these communication issues and prioritizing cross-departmental and cross-organizational alignment, HEPPUs and analogous units can enhance their capacity to react promptly and effectively to a range of emergency situations, leading to improved patient outcomes and strengthened healthcare resilience (Chen et al. 2013; Chirico et al. 2023).
This study further explored obstacles and constraints faced by the HEPPU, such as lack of understanding of their role by other hospital personnel, personnel issues, approval difficulties, and synchronization efforts. Addressing these impediments is critical to increase the overall efficacy and efficiency of the unit in emergency planning and preparedness. Resolving these challenges may involve improving communication across departments, assigning additional resources, and defining roles and responsibilities to establish a more cohesive and systematic approach to emergency management (Bajow and Alkhalil 2014; Al Harthi et al. 2020; Alruwaili et al. 2022). The implications derived from these insights suggest that a comprehensive understanding of the hurdles encountered by the HEPPU is essential for refining the unit’s performance in emergency situations. Suggestions for surmounting these challenges include devising focused strategies for better communication and resource distribution, as well as offering extensive training to staff members to demystify their roles and responsibilities within the unit (Schultz et al. 2012; Veenema et al. 2016; Brinjee et al. 2021). By adopting these initiatives, healthcare systems can enable HEPPUs to overcome existing constraints, ultimately resulting in a more proficient and unified response to diverse emergency scenarios and strengthening the overall resilience of healthcare facilities.
5 Recommendations
Based on the results of this study, we make the following recommendations: (1) Hospitals should further develop specialized emergency planning units that bring together different departments. This can improve coordination and make hospitals better prepared for crises. (2) Hospitals should prioritize building emergency preparedness units that get input from all relevant departments and take a big-picture approach to planning. (3) To make emergency planning units work better, hospitals should improve communication between departments, be transparent, and promote teamwork. (4) Hospitals can optimize emergency planning by improving communication, distributing resources effectively, and training staff.
6 Conclusion
In conclusion, this study highlighted the critical role and challenges faced by HEPPUs in enhancing healthcare system resilience and ensuring effective disaster management. The study identified four key themes: establishment and evolution of the HEPPU, roles and responsibilities, communication and coordination, and challenges and limitations. The Covid-19 pandemic emphasized the need for specialized units, such as the HEPPU, and the importance of interdisciplinary collaboration and an all-encompassing approach to emergency preparedness. Robust communication and coordination among stakeholders are crucial to enhance the unit’s capacity to react effectively in various emergency situations, ultimately leading to improved patient outcomes and strengthened healthcare resilience. Furthermore, addressing challenges such as comprehension deficiencies, personnel issues, approval difficulties, and synchronization efforts through focused strategies for better communication, resource distribution, and extensive staff training is essential for refining the performance of HEPPUs in emergency situations. This study contributes valuable knowledge and offers practical recommendations for enhancing preparedness and resilience for future emergencies, emphasizing the importance of continued development and support for the HEPPU in ensuring effective disaster management across healthcare systems.
References
Abuadas, M.H., and Z.F. Albikawi. 2022. Predictors of disaster preparedness among registered nurses in Saudi Arabia: A structural equation modelling analysis. Australasian Emergency Care 25(2): 132–139.
Aitsi-Selmi, A., and V. Murray. 2015. The Sendai framework: Disaster risk reduction through a health lens. Bulletin of the World Health Organization 93(6): 362–362.
Al Harthi, M., A. Al Thobaity, W. Al Ahmari, and M. Almalki. 2020. Challenges for nurses in disaster management: A scoping review. Risk Management and Healthcare Policy 13: 2627–2634.
Al Harthi, M., A. Al Thobaity, M. Almalki, and W. Al Ahmari. 2021. Improving disaster readiness and the response of nurses in Saudi Arabia. Risk Management and Healthcare Policy 14: 4537–4544.
Al Thobaity, A., V. Plummer, K. Innes, and B. Copnell. 2015. Perceptions of knowledge of disaster management among military and civilian nurses in Saudi Arabia. Australasian Emergency Nursing Journal 18(3): 156–164.
Al Thobaity, A., B. Williams, and V. Plummer. 2016. A new scale for disaster nursing core competencies: Development and psychometric testing. Australasian Emergency Nursing Journal 19(1): 11–19.
Al Thobaity, A., S. Alamri, V. Plummer, and B. Williams. 2019. Exploring the necessary disaster plan components in Saudi Arabian hospitals. International Journal of Disaster Risk Reduction 41: Article 101316.
Ali, H.M., C. Desha, J. Ranse, and A. Roiko. 2021. Planning and assessment approaches towards disaster resilient hospitals: A systematic literature review. International Journal of Disaster Risk Reduction 61: Article 102319.
Alruwaili, A., M.S. Islam, and K. Usher. 2022. Hospitals disaster preparedness and management in the Eastern Province of the Kingdom of Saudi Arabia: A cross-sectional study. Disaster Medicine and Public Health Preparedness 16(3): 1038–1045.
Al-Tawfiq, J.A., and Z.A. Memish. 2014. Mass gathering medicine: 2014 Hajj and Umra preparation as a leading example. International Journal of Infectious Diseases 27: 26–31.
Al-Wathinani, A., A.J. Hertelendy, S. Alhurishi, A. Mobrad, R. Alhazmi, M. Altuwaijri, M. Alanazi, R. Alotaibi, and K. Goniewicz. 2020. Increased emergency calls during the COVID-19 pandemic in Saudi Arabia: A national retrospective study. Healthcare 9(1): Article 14.
Al-Wathinani, A., A.J. Hertelendy, A.M. Mobrad, R. Alhazmi, S. Althunayyan, M.S. Molloy, and K. Goniewicz. 2021. Emergency medical providers’ knowledge regarding disasters during mass gatherings in Saudi Arabia. Sustainability 13(6): Article 3342.
Bahrami, P., A. Ardalan, A. Nejati, A. Ostadtaghizadeh, and A. Yari. 2020. Factors affecting the effectiveness of hospital incident command system; findings from a systematic review. Bulletin of Emergency & Trauma 8(2): Article 62.
Bajow, N.A., and S.M. Alkhalil. 2014. Evaluation and analysis of hospital disaster preparedness in Jeddah. Health 6(19): Article 2668.
Bayram, J.D., and S. Zuabi. 2012. Disaster metrics: Quantification of acute medical disasters in trauma-related multiple casualty events through modeling of the acute medical severity index. Prehospital and Disaster Medicine 27(2): 130–135.
Bradley, D.T., M. McFarland, and M. Clarke. 2016. The effectiveness of disaster risk communication: A systematic review of intervention studies. PLoS Currents Disasters 81–120.
Brinjee, D., A. Al Thobaity, M. Almalki, and W. Alahmari. 2021. Identify the disaster nursing training and education needs for nurses in Taif City, Saudi Arabia. Risk Management and Healthcare Policy 14: 2301–2310.
Brooks, S.K., G.J. Rubin, and N. Greenberg. 2019. Traumatic stress within disaster-exposed occupations: Overview of the literature and suggestions for the management of traumatic stress in the workplace. British Medical Bulletin 129(1): 25–34.
Chen, J., T.H.Y. Chen, I. Vertinsky, L. Yumagulova, and C. Park. 2013. Public–private partnerships for the development of disaster resilient communities. Journal of Contingencies and Crisis Management 21(3): 130–143.
Chirico, F., G. Nucera, L. Szarpak, and S. Zaffina. 2023. The cooperation between occupational and public health stakeholders and its decisive role in the battle against the COVID-19 pandemic. Disaster Medicine and Public Health Preparedness 17: Article e100.
Djalali, A., V. Hosseinijenab, M. Peyravi, M. Nekoei-Moghadam, B. Hosseini, L. Schoenthal, and K.L. Koenig. 2015. The hospital incident command system: Modified model for hospitals in Iran. PLoS Currents 7. https://doi.org/10.1371/currents.dis.45d66b5258f79c1678c6728dd920451a.
El Sayed, M., A.F. Chami, and E. Hitti. 2018. Developing a hospital disaster preparedness plan for mass casualty incidents: Lessons learned from the downtown Beirut bombing. Disaster Medicine and Public Health Preparedness 12(3): 379–385.
Guha-Sapir, D., R. Below, and P. Hoyois. 2009. EM-DAT: The CRED/OFDA International Disaster Database. www.emdat.be. Brussels, Belgium: Université Catholique de Louvain.
Hasan, M.K., S.M. Nasrullah, A. Quattrocchi, P. Arcos González, and R. Castro Delgado. 2022. Hospital surge capacity preparedness in disasters and emergencies: Protocol for a systematic review. International Journal of Environmental Research and Public Health 19(20): Article 13437.
Hendrickx, C., S. D’Hoker, G. Michiels, and M. Sabbe. 2016. Principles of hospital disaster management: An integrated and multidisciplinary approach. B-ENT Supplements 26(2): 139–148.
Hu, H., Y. Ma, L. Kong, J. Guo, J. Wang, M. Liu, Y. Li, and J. Wang et al. 2017. Application of hazard vulnerability analysis risk assessment for hospital acquired infection management. Chinese Journal of Hospital Administration 12: 822–825.
Kaji, A.H., and R.J. Lewis. 2006. Hospital disaster preparedness in Los Angeles County. Academic Emergency Medicine 13(11): 1198–1203.
Khan, A., J. Alowais, A. Nofal, and T. Alama. 2021. Assessment of disaster preparedness at general hospitals in Al-Madinah Al-Munawarah Province, Western region of Saudi Arabia: A study of pre intervention and post intervention test scores from 2017 to 2019. Saudi Medical Journal 42(5): Article 537.
Khorram-Manesh, A., O. Lupesco, T. Friedl, G. Arnim, K. Kaptan, A.R. Djalali, M. Foletti, and P.L. Ingrasia et al. 2016. Education in disaster management: What do we offer and what do we need? Proposing a new global program. Disaster Medicine and Public Health Preparedness 10(6): 854–873.
Larson, E., and L.H. Raney. 2008. Emergency incident management systems: Fundamentals and applications. Hoboken, NJ: Wiley.
Marcozzi, D.E., R. Pietrobon, J.V. Lawler, M.T. French, C. Mecher, J. Peffer, N.E. Baehr, and B.J. Browne. 2020. Development of a hospital medical surge preparedness index using a national hospital survey. Health Services and Outcomes Research Methodology 20(1): 60–83.
MOH (Ministry of Health). 2019. Emergency, Disasters and Ambulatory Transportation General Department. https://www.moh.gov.sa/en/Ministry/Forms/EDATGD/Pages/default.aspx. Accessed 9 Jan 2023.
Olivieri, C., P.L. Ingrassia, F. Della Corte, L. Carenzo, J.-M. Sapori, L. Gabilly, F. Segond, and F. Grieger et al. 2017. Hospital preparedness and response in CBRN emergencies: TIER assessment tool. European Journal of Emergency Medicine 24(5): 366–370.
Patel, S.S., M.B. Rogers, R. Amlôt, and G.J. Rubin. 2017. What do we mean by “community resilience”? A systematic literature review of how it is defined in the literature. PLoS Currents Disasters 9. https://doi.org/10.1371/currents.dis.db775aff25efc5ac4f0660ad9c9f7db2.
Phuspa, S.M., M. Kamal, and E. Rosanti. 2019. Hospital fire risk analysis with hazard, vulnerability, capacity, risk assessment model. KEMAS Jurnal Kesehatan Masyarakat 14(3): 353–358.
Prakash Narain, J., P. Sodani, and L. Kant. 2021. COVID-19 pandemic: Lessons for the health systems. Journal of Health Management 23(1): 74–84.
Schultz, C.H., K.L. Koenig, M. Whiteside, R. Murray, and National Standardized All-Hazard Disaster Core Competencies Task. Force. 2012. Development of national standardized all-hazard disaster core competencies for acute care physicians, nurses, and EMS professionals. Annals of Emergency Medicine 59(3): 196–208.
Shabanikiya, H., M. Jafari, H.A. Gorgi, H. Seyedin, and A. Rahimi. 2019. Developing a practical toolkit for evaluating hospital preparedness for surge capacity in disasters. International Journal of Disaster Risk Reduction 34: 423–428.
Sheikhbardsiri, H., A.R. Raeisi, M. Nekoei-Moghadam, and F. Rezaei. 2017. Surge capacity of hospitals in emergencies and disasters with a preparedness approach: A systematic review. Disaster Medicine and Public Health Preparedness 11(5): 612–620.
Shooshtari, S., S. Tofighi, and S. Abbasi. 2017. Benefits, barriers, and limitations on the use of hospital incident command system. Journal of Research in Medical Sciences 22: Article 36.
Søvold, L.E., J.A. Naslund, A.A. Kousoulis, S. Saxena, M.W. Qoronfleh, C. Grobler, and L. Münter. 2021. Prioritizing the mental health and well-being of healthcare workers: An urgent global public health priority. Frontiers in Public Health 9: Article 679397.
Stoto, M.A., C. Nelson, R. Piltch-Loeb, L.N. Mayigane, F. Copper, and S. Chungong. 2019. Getting the most from after action reviews to improve global health security. Globalization and Health 15: 1–10.
Sultan, M.A.S., A. Khorram-Manesh, J.L. Sørensen, J. Berlin, and E. Carlström. 2023. Disaster collaborative exercises for healthcare teamwork in a Saudi context. International Journal of Disaster Risk Science 14(2): 183–193.
Timbie, J.W., J.S. Ringel, D.S. Fox, F. Pillemer, D.A. Waxman, M. Moore, C.K. Hansen, and A.R. Knebel et al. 2013. Systematic review of strategies to manage and allocate scarce resources during mass casualty events. Annals of Emergency Medicine 61(6): 677–689.
Veenema, T.G. 2018. Disaster nursing and emergency preparedness. Berlin: Springer.
Veenema, T.G., A. Griffin, A.R. Gable, L. MacIntyre, R.N. Simons, M.P. Couig, J.J. Walsh, and R.P. Lavin et al. 2016. Nurses as leaders in disaster preparedness and response—A call to action. Journal of Nursing Scholarship 48(2): 187–200.
Wang, Y., H. Hao, and L.S. Platt. 2021. Examining risk and crisis communications of government agencies and stakeholders during early-stages of COVID-19 on Twitter. Computers in Human Behavior 114: Article 106568.
Yadav, D.K., and A. Barve. 2015. Analysis of critical success factors of humanitarian supply chain: An application of interpretive structural modeling. International Journal of Disaster Risk Reduction 12: 213–225.
Zhong, S., X.-Y. Hou, M. Clark, Y.-L. Zang, L. Wang, L.-Z. Xu, and G. FitzGerald. 2014. Disaster resilience in tertiary hospitals: A cross-sectional survey in Shandong Province, China. BMC Health Services Research 14(1): 1–10.
Acknowledgments
The authors express their gratitude to the deanship of scientific research at Taif University for funding this study. They also acknowledge the continuous support provided by the Deanship of Postgraduate Studies at Taif University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alharazi, A., Al Thobaity, A. From Planning to Execution: Delving into the Crucial Role and Challenges of HEPPUs in Hospital Emergency Management. Int J Disaster Risk Sci 14, 858–867 (2023). https://doi.org/10.1007/s13753-023-00522-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13753-023-00522-w