Abstract
Purpose
To examine the association of marital status with prostate cancer outcomes in a racially-diverse cohort.
Methods
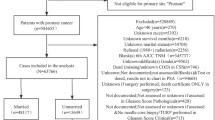
The study population consisted of men (1010 Black; 1070 White) with incident prostate cancer from the baseline North Carolina-Louisiana Prostate Cancer (PCaP) cohort. Marital status at time of diagnosis and screening history were determined by self-report. The binary measure of marital status was defined as married (including living as married) vs. not married (never married, divorced/separated, or widowed). High-aggressive tumors were defined using a composite measure of PSA, Gleason Score, and stage. Definitive treatment was defined as receipt of radical prostatectomy or radiation. Multivariable logistic regression was used to examine the association of marital status with (1) high-aggressive tumors, (2) receipt of definitive treatment, and (3) screening history among Black and White men with prostate cancer.
Results
Black men were less likely to be married than White men (68.1% vs. 83.6%). Not being married (vs. married) was associated with increased odds of high-aggressive tumors in the overall study population (adjusted Odds Ratio (aOR): 1.56; 95% Confidence Interval (CI): 1.20–2.02) and both Black and White men in race-stratified analyses. Unmarried men were less likely to receive definitive treatment in the overall study population (aOR: 0.68; 95% CI: 0.54–0.85). In race-stratified analyses, unmarried Black men were less likely to receive definitive treatment. Both unmarried Black and White men were less likely to have a history of prostate cancer screening than married men.
Conclusion
Lower rates of marriage among Black men might signal decreased support for treatment decision-making, symptom management, and caregiver support which could potentially contribute to prostate cancer disparities.
Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from PCaP management team. Restrictions apply to the availability of these data.
References
National Cancer Institute (2021) Cancer stat facts: prostate cancer. https://seer.cancer.gov/statfacts/html/prost.html. Accessed May 6,
DeSantis CE, Siegel RL, Sauer AG et al (2016) Cancer statistics for African americans, 2016: progress and opportunities in reducing racial disparities. CA Cancer J Clin 66:290–308
Khan S, Hicks V, Rancilio D, Langston M, Richardson K, Drake BF (2018) Predictors of Follow-Up visits Post Radical Prostatectomy. Am J Men’s Health 12:760–765
Akinyemiju T, Wiener H, Pisu M (2017) Cancer-related risk factors and incidence of major cancers by race, gender and region; analysis of the NIH-AARP diet and health study. BMC Cancer 17:597
Kinsella N, Stattin P, Cahill D et al (2018) Factors influencing men’s choice of and adherence to active surveillance for low-risk Prostate Cancer: a mixed-method systematic review. Eur Urol 74:261–280
O’Shaughnessy PK, Laws TA, Esterman AJ (2015) The Prostate cancer journey: results of an online survey of men and their partners. Cancer Nurs 38:E1–E12
Capistrant BD, Lesher L, Kohli N et al (2018) Social Support and Health-Related Quality of Life among Gay and bisexual men with Prostate Cancer. Oncol Nurs Forum 45:439–455
Drake BF, Lewis-Thames MW, Brown A, Rancilio D, Hicks V (2019) An evaluation of Follow-Up activities of participants from an urban Prostate Cancer screening event. Am J Men’s Health 13:1557988319844353
Chen Z-H, Yang K-B, Zhang Y-Z et al (2021) Assessment of Modifiable Factors for the Association of Marital Status with Cancer-Specific Survival. JAMA Netw Open 4:e2111813
Xiao H, Tan F, Goovaerts P (2011) Racial and geographic disparities in late-stage Prostate cancer diagnosis in Florida. J Health Care Poor Underserved 22:187–199
Schymura MJ, Kahn AR, German RR et al (2010) Factors associated with initial treatment and survival for clinically localized Prostate cancer: results from the CDC-NPCR patterns of Care Study (PoC1). BMC Cancer 10:152
Kan CK, Qureshi MM, Gupta A et al (2018) Risk factors involved in treatment delays and differences in treatment type for patients with Prostate cancer by risk category in an academic safety net hospital. Adv Radiat Oncol 3:181–189
Denberg TD, Beaty BL, Kim FJ, Steiner JF (2005) Marriage and ethnicity predict treatment in localized prostate carcinoma. Cancer 103:1819–1825
Aizer AA, Chen MH, McCarthy EP et al (2013) Marital status and survival in patients with cancer. J Clin Oncol 31:3869–3876
Xiao H, Warrick C, Huang Y (2009) Prostate cancer treatment patterns among racial/ethnic groups in Florida. J Natl Med Assoc 101:936–943
Montiel Ishino FA, Rowan C, Das R et al (2020) Identifying risk profiles of malignant Prostate Cancer Surgical Delay using a person-centered Approach to understand Prostate Cancer disparities: the Constellation of Health determinants using latent class analysis on Cancer Registry Data. Am J Mens Health 14:1557988320984282
Khan S, Nepple KG, Kibel AS et al (2019) The association of marital status and mortality among men with early-stage Prostate cancer treated with radical prostatectomy: insight into post-prostatectomy survival strategies. Cancer Causes Control 30:871–876
Abdollah F, Sun M, Thuret R et al (2011) The effect of marital status on stage and survival of Prostate cancer patients treated with radical prostatectomy: a population-based study. Cancer Causes Control 22:1085–1095
Burns RM, Sharp L, Sullivan FJ, Deady SE, Drummond FJ, C ON (2014) Factors driving inequality in Prostate cancer survival: a population based study. PLoS ONE 9:e106456
Du KL, Bae K, Movsas B, Yan Y, Bryan C, Bruner DW (2012) Impact of marital status and race on outcomes of patients enrolled in Radiation Therapy Oncology Group Prostate cancer trials. Support Care Cancer 20:1317–1325
King AJ, Evans M, Moore TH et al (2015) Prostate cancer and supportive care: a systematic review and qualitative synthesis of men’s experiences and unmet needs. Eur J Cancer Care (Engl) 24:618–634
Tyson MD, Andrews PE, Etzioni DA et al (2013) Marital status and Prostate cancer outcomes. Can J Urol 20:6702–6706
Donachie K, Cornel E, Pelgrim T et al (2022) What interventions affect the psychosocial burden experienced by Prostate cancer patients undergoing active surveillance? A scoping review. Support Care Cancer 30:4699–4709
Kaufman G, Goldscheider F (2007) Do men need a spouse more than women? Perceptions of the importance of marriage for men and women. Sociol Q 48:29–46
Umberson D, Donnelly R, Pollitt AM (2018) Marriage, Social Control, and Health Behavior: a dyadic analysis of same-sex and different-sex couples. J Health Soc Behav 59:429–446
Schroeder JC, Bensen JT, Su LJ et al (2006) The North Carolina-Louisiana Prostate Cancer Project (PCaP): methods and design of a multidisciplinary population-based cohort study of racial differences in Prostate cancer outcomes. Prostate 66:1162–1176
Weinberg CR, Sandler DP (1991) Randomized recruitment in case-control studies. Am J Epidemiol 134:421–432
Salmon C, Song L, Muir K et al (2021) Marital status and Prostate cancer incidence: a pooled analysis of 12 case-control studies from the PRACTICAL consortium. Eur J Epidemiol 36:913–925
Hanske J, Meyer CP, Sammon JD et al (2016) The influence of marital status on the use of breast, cervical, and Colorectal cancer screening. Prev Med 89:140–145
Tangen CM, Goodman PJ, Till C, Schenk JM, Lucia MS, Thompson IM Jr (2016) Biases in recommendations for and acceptance of prostate biopsy significantly affect assessment of Prostate cancer risk factors: results from two large randomized clinical trials. J Clin Oncol 34:4338
Zhang J, Xu H, Zheng L et al (2020) Determinants of participation and detection rate of Colorectal cancer from a population-based screening program in China. Front Oncol 10:1173
Salmon C, Parent M, Quesnel-Vallée A, Barnett TA (2022) A scoping review of social relationships and Prostate cancer screening. Prev Med 154:106892
Franks MM, Stephens MAP, Rook KS, Franklin BA, Keteyian SJ, Artinian NT (2006) Spouses’ provision of health-related support and control to patients participating in cardiac rehabilitation. J Fam Psychol 20:311
Harlan LC, Potosky A, Gilliland FD et al (2001) Factors associated with initial therapy for clinically localized Prostate cancer: Prostate cancer outcomes study. J Natl Cancer Inst 93:1864–1871
Hoffman RM, Harlan LC, Klabunde CN et al (2003) Racial differences in initial treatment for clinically localized Prostate cancer. J Gen Intern Med 18:845–853
Okoro O, Rutherford C, Witherspoon S (2018) Leveraging the family influence of women in Prostate cancer efforts targeting African American men. J Racial Ethnic Health Disparities 5:820–830
Allen JD, Akinyemi IC, Reich A, Fleary S, Tendulkar S, Lamour N (2018) African American women’s involvement in promoting informed decision-making for Prostate cancer screening among their partners/spouses. Am J Men’s Health 12:884–893
Bergner EM, Cornish EK, Horne K, Griffith DM (2018) A qualitative meta-synthesis examining the role of women in African American men’s Prostate cancer screening and treatment decision making. Psycho‐oncology 27:781–790
Aughinbaugh A, Robles O, Sun H (2013) Marriage and divorce: patterns by gender, race, and educational attainment. Monthly Lab Rev 136:1
Stevenson B, Wolfers J (2007) Marriage and divorce: changes and their driving forces. J Economic Perspect 21:27–52
Griffith DM, Mason MA, Rodela M et al (2007) A structural approach to examining Prostate cancer risk for rural southern African American men. J Health Care Poor Underserved 18:73–101
Hammond WP, Mohottige D, Chantala K, Hastings JF, Neighbors HW, Snowden L (2011) Determinants of usual source of care disparities among African American and Caribbean Black men: findings from the National Survey of American Life. J Health Care Poor Underserved 22:157–175
Hammond WP, Matthews D, Corbie-Smith G (2010) Psychosocial factors associated with routine health examination scheduling and receipt among African American men. J Natl Med Assoc 102:276–289
Imm KR, Williams F, Housten AJ et al (2017) African American Prostate cancer survivorship: exploring the role of social support in quality of life after radical prostatectomy. J Psychosoc Oncol 35:409–423
Acknowledgements
The authors thank the staff, advisory committees and research subjects participating in the PCaP study for their important contributions.
Funding
The North Carolina-Louisiana Prostate Cancer Project (PCaP) is carried out as a collaborative study supported by the Department of Defense contract DAMD 17-03-2-0052. SK is supported by the Foundation of Barnes-Jewish Hospital and Siteman Cancer Center.
Author information
Authors and Affiliations
Contributions
SK: conceptualization, data curation, formal analysis, methodology, writing-original draft, writing-review and editing. LF: conceptualization, writing-original draft, writing-review and editing. ML: conceptualization, writing-original draft, writing-review and editing. YH: conceptualization, writing-original draft, writing-review and editing. JXM: conceptualization, writing-original draft, writing-review and editing. KG: conceptualization, writing-original draft, writing-review and editing. SS: methodology, writing-original draft, writing-review and editing. JTB: funding acquisition, project administration, resources, writing-review and editing. JLM: funding acquisition, resources, writing-review and editing. ETHF: funding acquisition, writing-review and editing. LS: conceptualization, project administration, writing-review and editing. MWL-T: conceptualization, writing-original draft, writing-review and editing.
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khan, S., Fuzzell, L., Langston, M. et al. The impact of marital status on tumor aggressiveness, treatment, and screening among black and white men diagnosed with prostate cancer. Cancer Causes Control 35, 531–539 (2024). https://doi.org/10.1007/s10552-023-01821-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01821-9