Abstract
Device therapy is a nonpharmacological approach that presents a crucial advancement for managing patients with atrial fibrillation (AF) and heart failure with preserved ejection fraction (HFpEF). This review investigated the impact of device-based interventions and emphasized their potential for optimizing treatment for this complex patient demographic. Cardiac resynchronization therapy, augmented by atrioventricular node ablation with His-bundle pacing or left bundle-branch pacing, is effective for enhancing cardiac function and establishing atrioventricular synchrony. Cardiac contractility modulation and vagus nerve stimulation represent novel strategies for increasing myocardial contractility and adjusting the autonomic balance. Left ventricular expanders have demonstrated short-term benefits in HFpEF patients but require more investigation for long-term effectiveness and safety, especially in patients with AF. Research gaps regarding complications arising from left ventricular expander implantation need to be addressed. Device-based therapies for heart valve diseases, such as transcatheter aortic valve replacement and transcatheter edge-to-edge repair, show promise for patients with AF and HFpEF, particularly those with mitral or tricuspid regurgitation. Clinical evaluations show that these device therapies lessen AF occurrence, improve exercise tolerance, and boost left ventricular diastolic function. However, additional studies are required to perfect patient selection criteria and ascertain the long-term effectiveness and safety of these interventions. Our review underscores the significant potential of device therapy for improving the outcomes and quality of life for patients with AF and HFpEF.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is a rapid supraventricular arrhythmia characterized by irregular electrical activity and ineffective atrial contractions. The incidence of AF gradually increases with age and has become a major public health concern [1]. Currently, heart failure (HF) is recognized as the most common complication in patients with AF, who have a fourfold higher risk of death from HF than from stroke [2]. Furthermore, AF is the most common type of arrhythmia in patients with HF, occurring in 24 − 44% of patients with acute HF and 33% of those with chronic HF [3]. The correlation between AF and heart failure with preserved ejection fraction (HFpEF) is more pronounced than that between AF and heart failure with reduced ejection fraction (HFrEF) [4, 5]. The incidence of HFpEF in patients with AF is approximately five times higher than that in patients without AF, and women generally have a higher incidence of HFpEF than men [6, 7]. Over 30% of patients with HFpEF experience concomitant AF [8]. The DOSE (Diuretics Optimization Strategies Evaluation) study [9] revealed that in patients with acutely decompensated HFpEF, AF can be prevalent in up to 69% of cases. Furthermore, existing evidence suggests that the presence of AF in HFpEF increases the risk of all-cause mortality and stroke, particularly when AF is incident [10]. These findings indicate a potential interplay between AF and HFpEF, leading to the formation of a vicious cycle.
Considering the observed clinical comorbidity between AF and HFpEF, shared pathophysiological mechanisms likely underlie both conditions. Both AF and HFpEF share common risk factors and comorbidities, such as aging, hypertension, obesity, and sleep apnea [1, 11]. This elevates the risk of developing both conditions. Current studies indicate that specific proinflammatory cytokines, such as tumor necrosis factor, interleukin-1, and interleukin-6, play roles in the pathogenesis of HFpEF [12], suggesting that HFpEF might be an inflammatory disorder. This proinflammatory environment in HFpEF can lead to endothelial dysfunction, oxidative stress, microvascular inflammation, and chronic fibrotic changes [13]. These factors contribute to diastolic dysfunction, which is also a pivotal mechanism in the development and persistence of AF. HFpEF can lead to left atrial enlargement and increased atrial fibrosis, disrupting gap junction distribution and intercellular coupling in fibrotic areas [14, 15]. This contributes to electrical remodeling, fostering the onset of AF. Additionally, HFpEF may elevate the activity of adrenergic and renin-angiotensin-aldosterone systems, promoting atrial fibrosis and AF development [16].
AF itself can lead to atrial dilation, atrial fibrosis, and impaired atrial function, thereby promoting the occurrence of HFpEF [17]. Remodeling of the atrioventricular annular associated with AF, along with the progressive development of mitral and tricuspid regurgitation (TR), may also represent another mechanism for HFpEF [18]. In patients with persistent AF, depletion of atrial natriuretic peptide can facilitate vasoconstriction and edema, providing a potential foundation for the development of HFpEF [19]. Additionally, AF is associated with left ventricular myocardial fibrosis, which contributes to diastolic dysfunction and HFpEF [20].
Currently, novel guideline-directed medical therapy (GDMT), including angiotensin receptor-neprilysin inhibitors, beta-blockers, mineralocorticoid receptor antagonists, and sodium-glucose cotransporter-2 inhibitors, has emerged as the preferred treatment approach for HF [21, 22]. Landmark trials have unequivocally shown significant benefits of this therapeutic regimen in patients with HFrEF [23,24,25]. Historically, certain medications such as sodium-glucose co-transporter-2 inhibitors and angiotensin receptor-neprilysin inhibitors have been spotlighted for their potential effectiveness in HFpEF patients [26,27,28,29,30,31]. However, emerging data from the STEP-HFpEF trial underscores the notable advantages of glucagon-like peptide-1 receptor agonists for obese HFpEF patients, especially in enhancing their quality of life [32]. It is worth noting that despite these advancements, drug treatments for HFpEF still face challenges in efficacy, and a definitive treatment strategy for AF patients complicated by HFpEF remains elusive. This article reviews the latest developments in mechanical treatments for AF and HFpEF and aims to advance the standardized management of this patient population.
Clinical features
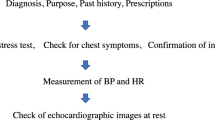
Both AF and HFpEF may present with symptoms such as palpitations, chest tightness, and dyspnea. B-type natriuretic peptide (BNP) levels are increased during AF episodes and rapidly normalize after conversion to sinus rhythm [33]. Diagnosing AF complicated by HFpEF based on clinical presentation and BNP levels alone may be challenging. Diagnosing HFpEF is straightforward in cases of volume overload. However, AF with a capacity imbalance may impact the assessment of left ventricular ejection fraction (LVEF), which may lead to an incorrect HFpEF diagnosis. Therefore, the diagnostic thresholds of BNP and NT-proBNP for AF complicated by HFpEF should be increased to 240 pg/mL and 660 pg/mL, respectively [3]. In addition to traditional diagnostic methods, the H2FPEF score and HFA-PEFF score can be used to diagnose HFpEF (Fig. 1). The study by Sepehrvand et al. [34] found that an H2FPEF score of > 2 had a sensitivity of 89–90% to detect HFpEF and that an H2FPEF score < 6 had a specificity of 82% to rule out HFpEF in the Alberta HEART population. However, it should be noted that the population recruited into Alberta HEART is nonrandom, and differences in HFpEF prevalence will influence positive and negative predictive values. Additionally, patients with higher H2FPEF scores are at a higher risk of adverse events [34]. The HFA-PEFF score is the other new diagnostic algorithm that accounts for various factors, and higher scores are associated with an increased risk of rehospitalization and all-cause mortality in patients with HF [35]. Although specificity was robust for both scores, sensitivity was poorer for HFA-PEFF, with a false-negative rate of 55% for low-probability scores compared with 25% using the H2FPEF score [36]. These scores offer new methods for diagnosing AF and HFpEF, but they are not without limitations. For instance, the H2FPEF score overlooks BNP levels, and its accuracy and utility require thorough evaluation. Furthermore, the HFA-PEFF score is overly lengthy and complicated, challenging its widespread implementation.
H2FPEF score and HFA-PEFF score. BMI, body mass index; RVSP, right ventricular systolic pressure; e’, septal mitral annulus tissue relaxation velocity in early diastole; E/e’, the ratio of early diastolic mitral inflow velocity to septal mitral annulus tissue relaxation velocity; TR, tricuspid regurgitation; LAVI, left atrial volume index; RWT, relative wall thickness; LVMI, left ventricular mass index; BNP, B-type natriuretic peptide; NT-proBNP, N-terminal pro-B-type natriuretic peptide; AF, atrial fibrillation; LV, left ventricle; HFpEF, heart failure with preserved ejection fraction
In the era of big data, artificial intelligence technology has become increasingly sophisticated, and intelligent algorithms based on machine learning have resulted in breakthroughs in the medical field [37]. These breakthroughs may be used to develop important methods of auxiliary diagnosis and treatment in the future. Currently, deep learning models based on echocardiography have been used to classify the degree of diastolic dysfunction and aid in the diagnosis of HFpEF [38]. These models can identify HFpEF phenotypes with different clinical features and long-term prognoses [39], providing effective evidence for the stratified diagnosis and treatment of HFpEF. Additionally, machine learning based on different biomarkers can identify HFpEF subgroups with different biomarker spectra [40], which may reveal different underlying pathological and physiological pathways of HFpEF.
Challenges in pharmacological and interventional treatments
The efficacy of current medications for managing AF and HFpEF often falls short, leading to recurring symptoms or disease progression. Adverse effects from these medications, ranging from dizziness to increased bleeding risk, can affect patient adherence and overall well-being [41]. With AF and HFpEF patients frequently having multiple comorbidities, polypharmacy becomes a concern, introducing potential drug interactions and complicating treatment [42,43,44].
Despite the declining mortality rate in HFrEF patients due to new anti-HF drugs, the mortality rate in HFpEF patients remains concerning [45, 46]. This underscores the need for alternative treatments for AF and HFpEF [47, 48]. Ablation therapy, especially pulmonary vein isolation (PVI), has emerged as a significant treatment for AF [49]. Radiofrequency ablation (RFA) is more effective than drug therapy for maintaining sinus rhythm, reducing readmission, and improving diastolic function [50, 51]. In a detailed analysis of the CABANA trial data (trial code NCT00911508), Packer et al. [52] ascertained that catheter ablation outperformed antiarrhythmic drugs in enhancing the quality of life and curtailing AF recurrence specifically among patients with coexisting AF and HFpEF.
While RFA has proven effective, newer ablation technologies such as cryoballoon ablation and pulsed field ablation (PFA) offer potential advantages (Fig. 2). These methods promise safety and efficiency, with PFA notably preserving surrounding cardiac structures [53]. However, comprehensive research on these techniques is still in its infancy, warranting further exploration for their efficacy and safety in AF and HFpEF patients.
Diagrams of radiofrequency catheter ablation, cryoballoon ablation, and pulsed-field ablation. The image displays three distinct techniques for ablation. A Radiofrequency catheter ablation, which effectively achieves PVI through thermal ablation. B Balloon ablation in which cryogenic balloons are used to isolate the pulmonary vein. C Pulsed-field ablation in which irreversible micropores are formed in the myocardial membrane by administering pulsed electric fields. These micropores enable various ions to penetrate the membrane, ultimately disrupting the vital internal environment of cardiomyocytes and leading to their death. This process eventually results in the successful isolation of the pulmonary vein. The inset image in (C) provides a visual representation of how pulsed-field ablation functions
Instrumental therapy and management
In the evolving landscape of cardiovascular care, the management of patients presenting with both AF and HFpEF has emerged as a multifaceted challenge. In this context, instrument-based interventions have garnered significant attention and promise. This comprehensive exploration delves into the realm of device therapies. By examining these interventions, we aim to shed light on their potential roles in improving the clinical outcomes and quality of life of patients with AF and HFpEF.
Cardiac resynchronization therapy
Cardiac resynchronization therapy (CRT) achieves biventricular pacing (BVP) by increasing left ventricular pacing, which significantly improves heart function and increases long-term patient survival rates [54, 55]. There is currently limited evidence supporting the significant improvement of HFpEF prognosis after CRT; however, its potential lies in its ability to improve systolic and diastolic dyssynchrony and provide chronotropic support, which may increase the diastolic filling time of the heart [55,56,57]. A case report in 2010 showed that a woman with HFpEF and left bundle-branch block (LBBB) experienced improved clinical symptoms after receiving CRT [58], suggesting that CRT may benefit specific populations with HFpEF.
BVP-mode CRT significantly improves the prognosis of patients with HF; however, one-third of patients do not respond to CRT [59, 60]. BVP is not equivalent to physiological pacing but rather to fusion pacing formed by two ectopic pacing points. The risk of HF hospitalization and AF incidence significantly increases when the cumulative percentage ventricular pacing burden is above a threshold of 40% [61, 62]. Therefore, achieving greater ventricular resynchronization in the form of physiological pacing can significantly improve heart function and avoid pacemaker-induced cardiomyopathy [62, 63].
The His bundle is an extension of the physiological structure of the atrioventricular node that is connected to the left and right bundle branches and participates in the formation of the ventricular conduction system. Therefore, HBP is a new pacing mode that can replace BVP. Studies have shown that HBP-mode CRT can improve cardiac function in patients with AF and HFpEF after atrioventricular node ablation and is beneficial for antiventricular remodeling [64]. However, HBP has several limitations in clinical practice, including high thresholds and low sensing, owing to blocking characteristics similar to that of the atrioventricular node. Additionally, implantation difficulty and low surgical success rates are common challenges for HBP [65]. Almost half of the patients with HF combined with LBBB cannot normalize their QRS waves after HBP, and the benefits of HBP are limited for patients with intraventricular conduction block [66]. The concept of LBBP has been developed to address these issues [67]. LBBP avoids the area of the conduction block and captures the main trunk and proximal branches of the left bundle branch at their more distal end. Moreover, LBBP has lower operation difficulty and requires lower precision in lead placement, allowing it to be the optimal pacing mode for patients with LBBB [68, 69]. LBBP combined with atrioventricular node ablation can achieve clinical benefits similar to those obtained with HBP in patients with AF, with lower sensing thresholds and higher success rates. This has been recognized as a safe and effective treatment option. [70]
Currently, there is a lack of high-level clinical evidence directly demonstrating the significant benefits of CRT in patients with AF and HFpEF. Furthermore, current guidelines do not recommend CRT for patients with HFpEF [54]. However, CRT with HBP or LBBP in combination with atrioventricular node ablation may be a feasible alternative option for patients with coexisting LBBB or significant ventricular dyssynchrony with limited response to conventional treatments.
Cardiac contractility modulation
Cardiac contractility modulation (CCM) is an innovative implantable electronic device used to treat chronic HF. The device features a pulse generator, which functions similar to a pacemaker, and two active fixation leads that are typically placed in the right ventricular septum with an interelectrode spacing of at least 2 cm. The device delivers a nonexcitatory biphasic signal of 7.5 V and 20 ms to the right ventricular septum during the absolute refractory period, promoting phosphorylation of phospholamban in the patient’s sarcoplasmic reticulum. Phosphorylated phospholamban dissociates from Ca2+-ATPase 2a on the sarcoplasmic reticulum, leading to increased intracellular Ca2+ concentration and a positive inotropic effect without increasing myocardial oxygen consumption, which improves cardiac function [71, 72].
Long-term CCM use can significantly enhance exercise tolerance and patient quality of life. According to the FIX-HF study (NCT01381172), CCM implantation dramatically increased LVEF, 6-min walking distance, and peak oxygen consumption and markedly reduced the risks of cardiovascular death and hospitalization for HF. The overall treatment effectiveness of CCM was found to be over 90% [73].
CCM has been approved for patients with symptomatic HFrEF with normal or slightly prolonged QRS duration in the European Union, China, India, Brazil, and other countries [74]. CCM has demonstrated significant benefits, particularly in patients with a baseline LVEF between 35 and 45%. At the molecular level, CCM improves calcium regulation in patients with HFrEF, reverses the fetal gene program associated with HF, and improves cardiac remodeling [74]. However, there is limited clinical evidence for the use of CCM in patients with HFpEF. In 2016, a case report described the implantation of CCM in two 59-year-old women with HFpEF. The patients showed improvements in cardiac function, 6-min walk test results, quality of life scores, and exercise tolerance after one year of follow-up [75]. However, their LVEF values of 50% and 47% were not typical for HFpEF, casting doubt on the effectiveness of the trial. In 2022, the CCM-HFpEF pilot study explored the use of CCM for the treatment of HFpEF [76]. The patients’ Kansas City Cardiomyopathy Questionnaire (KCCQ) composite score improved by 18.0 ± 16.6 points (p < 0.001) after 24 weeks of follow-up, and 93.6% of the patients did not experience any device- or procedure-related complications [76]. This trial provided a new strategy for the treatment of HFpEF, suggesting that CCM can significantly improve the health status of patients with HFpEF while ensuring their safety. Therefore, CCM may become another important nonpharmacological treatment for HFpEF.
Sinus rhythm is deemed necessary for effective treatment of CCM because the current CCM signal delivery algorithm requires sequential sensing of a p wave, followed by depolarizations at each ventricular lead [77]. It is noteworthy that most countries still consider AF a contraindication for CCM treatment. However, Röger et al. [78] found that CCM signal delivery is feasible in HF patients with permanent AF by sequential atrial-ventricular pacing, possibly due to the interpretation of the atrial pacing spike as a p wave by the CCM signal delivery algorithm. Additionally, the CCM-HFpEF pilot study [76] included almost half of the AF patients with HFpEF, revealing improvements in the KCCQ quality of life assessment. This suggests that CCM may offer encouraging potential benefits in improving the quality of life for HFpEF patients even when AF is present.
CCM treatment for patients with AF and HFpEF is still in the exploratory phase, and its actual clinical benefits are not yet clear. Some case reports and small sample studies have suggested that CCM may benefit patients with HFpEF; however, more robust evidence is necessary to support this claim. Therefore, routine CCM treatment for patients with AF and HFpEF is not currently recommended.
Autonomic neuromodulation therapies (ANMTs)
The autonomic nervous system (ANS) includes the sympathetic and parasympathetic nervous systems. The sympathetic nervous system increases the heart rate, enhances myocardial contractility, and promotes cardiac conduction. The parasympathetic nervous system innervates the sinoatrial node and atrioventricular bundle and branches and produces effects opposite to those of the sympathetic nervous system [79]. Overactivation of the sympathetic nervous system causes the opening of L-type calcium channels, which leads to an increase in intracellular calcium ions. This enhances Na+-Ca2+ exchange and automaticity in myocardial cells and results in early depolarization, which can induce AF. Overstimulation of the parasympathetic nervous system causes acetylcholine to bind to muscarinic potassium channels and produce a hyperpolarization current, which markedly shortens the atrial effective refractory period, leading to the occurrence of AF [80]. The physiological effects of the sympathetic and parasympathetic nervous systems are mutually exclusive; however, the two systems can function synergistically to promote AF when both are overactivated.
ANMTs are emerging treatment options that can regulate the ANS through surgical intervention or device-based therapy to suppress the occurrence of AF [81]. ANMTs typically include ganglion plexus ablation, epicardial injection of botulinum toxin, VNS, stellate ganglion block, baroreceptor activation therapy, earlobe VNS, spinal cord stimulation, and renal denervation; among those, VNS has been clinically implemented (Fig. 3) [79, 82,83,84].
VNS is a closed-loop, self-powered system that typically includes a stimulator and an implanted electrode. The stimulator was placed in the left subclavian area, and the electrode end with three helical coils was wrapped around the vagus nerve in the left carotid sheath. The external programmable controller allows adjustment of the VNS by regulating the stimulation mode and parameters [85]. Continuous low-frequency stimulation of the vagus nerve through VNS releases acetylcholine, which binds to nicotinic acetylcholine receptors on tissue macrophages, inhibiting the release of inflammatory factors and reducing myocardial damage [86,87,88]. Furthermore, VNS promotes cardiac electrical stability by reducing the loss of connexin 43 and has a certain reversal effect on electrical remodeling [82]. VNS was initially developed to treat refractory epilepsy; however, it has proven to be effective in significantly shortening the duration of paroxysmal AF and improving myocardial fibrosis [89]. It is also a safe and feasible option for patients with postoperative AF [88]. VNS can reduce cardiac inflammation and fibrosis and improve cardiac diastolic function in patients with HFpEF and has been validated in Dahl salt-sensitive rat models [90]. Recent studies have shown that continuous VNS for more than 3 months may significantly improve the quality of life and reduce the level of tumor necrosis factor-α in patients with HFpEF [91].
ANMTs are novel technologies that remain in the early stages of exploration. Despite extensive research on VNS, there is still a paucity of reliable evidence regarding its safety and effectiveness in patients with AF and HFpEF. Considering its significant benefits for patients with AF and HFpEF, VNS may emerge as a new alternative device therapy for these patients in the future.
Left ventricular expanders
Left ventricular expanders (LVEs) are spring-like devices implanted in the left ventricle to store elastic energy during cardiac contraction, releasing it during diastole. This process enhances left ventricular filling capacity, which is typically diminished in HFpEF [92].
The ImCardia and the CORolla transapical approach (CORolla TAA) devices are currently under development as two types of LVEs intended for implantation in the pericardium and endomyocardium, respectively. [92] ImCardia is an elastic, self-expanding device composed of a series of springs, with free lengths ranging from 35 to 46 mm, which are connected to attachment elements and screwed into the epimyocardium of the LV free wall 17 to 28 mm apart [93]. In animal models of diastolic dysfunction, ImCardia has been shown to be safe and effective in improving filling dynamics and enhancing cardiac contractility [94]. Furthermore, a prospective non-randomized study (NCT01347125) enrolled 19 HFpEF patients who underwent aortic valve replacement and were followed for 36 months. Although the intervention group exhibited no change in LVEF, reductions in left ventricular myocardial mass and left atrial area were observed. However, due to the complexities associated with implanting invasive devices, the trial had to be prematurely terminated.
CORolla TAA is a conical LVE composed of three elastic arms that can be implanted into the left ventricle through a transapical approach. Animal experiments have indicated a low incidence of adverse events associated with CORolla TAA implantation. Among 76 sheep models, one sheep experienced a significant decrease in LVEF, and two sheep developed mitral valve regurgitation. Active thrombi were detected in seven sheep, but all of them remained free of thrombosis after receiving antiplatelet therapy [95]. In an ongoing first-in-human clinical trial (NCT02499601), a 24-month follow-up is being conducted to assess the effectiveness and safety of CORolla TAA in 10 patients with HFpEF. One patient exhibited improvements in New York Heart Association (NYHA) functional class, KCCQ score, and a 6-min walk test at 6 months post-procedure. Additionally, at 12 months post-procedure, cardiac ultrasound indicated a reduction in left ventricular mass index (from 122 to 142 g/m2), left ventricular volume index (from 43 to 58 mL/m2), and left ventricular end-diastolic volume index (from 49 to 84 mL/m2). However, at 24 months post-procedure, the left ventricular mass index and left ventricular volume index increased to 130 g/m2 and 55 mL/m2, respectively, and the KCCQ score worsened to 44 points. Concerns about long-term cardiac function deterioration associated with CORolla TAA have been raised. This may be related to factors such as material fatigue, crack propagation, or stress corrosion cracking, necessitating further clinical trials to confirm the effectiveness and safety of CORolla TAA in HFpEF.
In short-term follow-up, LVEs have shown benefits for HFpEF patients, but their long-term effectiveness and safety remain uncertain. Currently, there is a lack of research evidence regarding LVEs in patients with AF and HFpEF. Furthermore, issues related to complications arising from LVE implantation, such as endomyocardial adhesions, valve damage, electrical conduction abnormalities, and potential impacts on pacemaker function, all require further investigation.
Others
In addition to conventional medical treatments, device-based therapies for heart valve diseases appear to offer potential benefits to patients with AF and HFpEF. Transcatheter aortic valve replacement (TAVR) and transcatheter edge-to-edge repair (TEER) are two eagerly anticipated minimally invasive procedures for the treatment of heart valve diseases. Both TAVR and TEER have demonstrated their effectiveness and safety in managing heart valve diseases, especially in elderly individuals at high risk who may not be suitable candidates for traditional surgical procedures [96, 97].
In patients with severe aortic stenosis (AS) and HF, TAVR has demonstrated a lower in-hospital mortality rate than surgical aortic valve replacement [98]. A retrospective cohort study involving 66 patients with severe AS and HFpEF revealed that TAVR significantly reduced pulmonary artery systolic pressure and the peak aortic valve gradient and led to an improved NYHA functional class at 1 month post-procedure [99]. For individuals with both AS and HFpEF, TAVR emerges as a promising therapeutic option. Nevertheless, new-onset AF is among the postoperative complications associated with TAVR. According to findings from the SOURCE XT study, preexisting AF was prevalent in 35.6% of TAVR patients, with a 7.2% incidence of new-onset AF. AF is linked to higher rates of all-cause mortality, cardiac mortality, and bleeding events in TAVR patients [100]. Consequently, the addition of AF ablation surgery to TAVR may provide supplementary clinical benefits.
TEER has demonstrated promising prognostic improvements in patients with AF and HFpEF, particularly in cases of moderate to severe mitral regurgitation (MR). Several observational trials have reported significant efficacy of TEER in ameliorating symptoms and enhancing the quality of life among HFpEF patients, a substantial portion of whom also present with AF [101, 102]. Moreover, findings from substantial randomized controlled trials (RCTs), such as the COAPT study, suggest a notable trend toward reduced hospitalization due to HF and decreased all-cause mortality among HF patients with moderate to severe secondary MR who undergo mitral valve clip therapy [103]. Notably, although COAPT’s primary focus was on patients with HFrEF, it is worth highlighting that nearly one-sixth of the participants had an ejection fraction exceeding 40%, underscoring TEER’s potential in addressing HFpEF.
The tricuspid valve, while often overshadowed in clinical discussions, plays a crucial role in the context of HFpEF, as indicated by recent research [104, 105]. Secondary TR, stemming from left HF, arises due to elevated left ventricular filling pressures. This pressure increase triggers right ventricular overload, leading to dilation of both the right heart and the tricuspid annulus, culminating in TR [106, 107]. The presence of AF can exacerbate this by causing further dilation of the tricuspid annulus [108]. This creates a detrimental feedback loop in patients with concurrent AF and TR. Recent retrospective studies have underscored the potential of tricuspid TEER in ameliorating cardiac function and possibly reducing mortality rates in patients grappling with severe TR and HFpEF [109]. This emphasizes the pivotal role of the tricuspid valve in managing HFpEF patients. However, a gap exists in the form of large-scale RCTs assessing TEER’s utility in AF and HFpEF patients, especially those with varying TR severities. This underscores the pressing need for more research to formulate holistic guidelines for tricuspid valve interventions in this demographic.
TAVR, as a minimally invasive surgical approach, holds promise for patients with heart valve diseases and HFpEF. When coupled with AF, adjunctive ablation procedures may provide additional benefits. Furthermore, TEER, recognized as an efficient interventional therapy, may hold potential benefits for patients with both AF and HFpEF who experience MR or TR. Although large-scale RCTs targeting specific patient populations are currently lacking, further clinical trials will contribute to validating the effectiveness and safety of both approaches.
Future directions and research
The need for RCTs
Instrument-based therapies have resulted in significant benefits to patients; however, the issue of surgical complications cannot be ignored, and different devices have their own limitations [54, 110]. Currently, there is limited trial evidence for the majority of instrument-based therapies in patients with AF combined with HFpEF. Furthermore, the efficacy of these therapies remains uncertain, which questions their ability to improve long-term patient outcomes. Therefore, it is necessary to strictly understand and follow the indications and contraindications of instrument-based therapies and use constantly updated new therapeutic equipment to enable maximum therapeutic and diagnostic benefit to patients.
A rigorous evaluation of alternative treatments for AF and HFpEF is required to establish their safety, efficacy, and potential clinical benefits. Currently, there is a need for large-scale RCTs that investigate non-pharmacological treatment options, such as ablation therapy, CRT, CCM, VNS, LVEs, and others, in patients with AF and HFpEF. These trials should be designed to compare novel treatment modalities against standard pharmacological therapies or in combination with them to determine optimal therapeutic strategies for managing these conditions. Additionally, RCTs should evaluate the long-term safety and efficacy of these alternative treatments and assess their impact on patient-reported outcomes, such as symptom burden, functional capacity, and quality of life.
Challenges in implementing new treatment modalities
The implementation of novel treatment modalities for AF and HFpEF introduces some challenges. Many new treatment options, particularly those involving advanced technologies or devices, may be associated with higher costs, limiting their accessibility for patients and healthcare systems [111]. Strategies to reduce costs and improve access to these treatments must be explored. Furthermore, the successful implementation of new treatment modalities requires adequate training and expertise among healthcare providers. This may involve the development of training programs, guidelines, and best practices to ensure proper execution and patient safety.
Identifying the most appropriate patient population for specific alternative treatments is crucial to optimize outcomes [112]. Researchers and clinicians must develop robust criteria for patient selection and account for factors such as disease severity, comorbidities, and patient preferences. The integration of new treatment options into clinical practice may face resistance from the medical community because of factors such as unfamiliarity, perceived risks, or concerns about the level of evidence supporting the new treatments. Continuous education, communication, and collaboration among healthcare professionals are essential for overcoming these barriers. The potential benefits of novel treatment approaches for AF and HFpEF can be more effectively realized after addressing these challenges, ultimately leading to improved patient care and outcomes.
Conclusions
AF and HFpEF are two interrelated conditions that have garnered increasing attention owing to their rising prevalence and significant impact on healthcare systems worldwide. The complex pathophysiology of these twin diseases is not completely understood, and the limitations of current pharmacological treatments lead to the inadequate management of many patients. In recent years, alternative treatment modalities, such as ablation therapy, CRT, CCM, VNS, LVEs, and others, have emerged as promising approaches to address the unmet clinical needs of patients with AF and HFpEF. These novel interventions have the potential to revolutionize patient care and outcomes by providing more effective and targeted therapies.
However, several challenges must be addressed to fully realize the benefits of these innovative treatment options, including cost and accessibility, training and expertise, patient selection, and resistance from the medical community. Furthermore, rigorous evaluation using RCTs is essential to establish the safety, efficacy, and clinical utility of these alternative treatments for the management of AF and HFpEF. Overcoming these challenges and pursuing further research into novel therapeutic approaches can improve the care of patients with AF and HFpEF, ultimately enhancing their quality of life and reducing the burden on healthcare systems worldwide.
Availability of data and material
No new data were generated or analyzed in support of this research.
Code availability
Figures 2 and 3 were created using the image bank of Servier Medical Art (http://smart.servier.com/), licensed under a Creative Commons Attribution 3.0 Unported License (https://creativecommons.org/licenses/by/3.0/).
Abbreviations
- AF:
-
Atrial fibrillation
- ANMTs:
-
Autonomic neuromodulation therapies
- ANS:
-
Autonomic nervous system
- AS:
-
Aortic stenosis
- BNP:
-
B-type natriuretic peptide
- BVP:
-
Biventricular pacing
- CCM:
-
Cardiac contractility modulation
- CRT:
-
Cardiac resynchronization therapy
- GDMT :
-
Guideline-directed medical therapy
- HBP:
-
His bundle pacing
- HF:
-
Heart failure
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- KCCQ:
-
Kansas City cardiomyopathy questionnaire
- LBBB:
-
Left bundle-branch block
- LBBP:
-
Left bundle-branch pacing
- LVEF:
-
Left ventricular ejection fraction
- LVEs:
-
Left ventricular expanders
- MR:
-
Mitral regurgitation
- NYHA:
-
New York Heart Association
- PFA:
-
Pulsed field ablation
- PVI:
-
Pulmonary vein isolation
- RCTs:
-
Randomized controlled trials
- RFA:
-
Radiofrequency ablation
- TAA:
-
Transapical approach
- TAVR:
-
Transcatheter aortic valve replacement
- TEER:
-
Transcatheter edge-to-edge repair
- TR:
-
Tricuspid regurgitation
- VNS:
-
Vagus nerve stimulation
References
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan G-A, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau J-P, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL (2021) 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 42(5):373–498
Reddy YNV, Borlaug BA, Gersh BJ (2022) Management of atrial fibrillation across the spectrum of heart failure with preserved and reduced ejection fraction. Circulation 146(4):339–357
Farmakis D, Chrysohoou C, Giamouzis G, Giannakoulas G, Hamilos M, Naka K, Tzeis S, Xydonas S, Karavidas A, Parissis J (2021) The management of atrial fibrillation in heart failure: an expert panel consensus. Heart Fail Rev 26(6):1345–1358
Temporelli PL, Arbelo E, Laroche C, Blomström-Lundqvist C, Kirchhof P, Lip GYH, Boriani G, Nakou E, Maggioni AP, Tavazzi L (2022) Atrial fibrillation ablation in heart failure: findings from the ESC-EHRA EORP Atrial Fibrillation Ablation long-term (AFA LT) registry. Int J Cardiol 346:19–26
Redfield MM, Borlaug BA (2023) Heart failure with preserved ejection fraction: a review. JAMA 329(10):827–838
Santhanakrishnan R, Wang N, Larson MG, Magnani JW, McManus DD, Lubitz SA, Ellinor PT, Cheng S, Vasan RS, Lee DS, Wang TJ, Levy D, Benjamin EJ, Ho JE (2016) Atrial fibrillation begets heart failure and vice versa: temporal associations and differences in preserved versus reduced ejection fraction. Circulation 133(5):484–492
Vermond RA, Geelhoed B, Verweij N, Tieleman RG, Van der Harst P, Hillege HL, Van Gilst WH, Van Gelder IC, Rienstra M (2015) Incidence of atrial fibrillation and relationship with cardiovascular events, heart failure, and mortality: a community-based study from the Netherlands. J Am Coll Cardiol 66(9):1000–1007
Campbell RT, McMurray JJV (2014) Comorbidities and differential diagnosis in heart failure with preserved ejection fraction. Heart Fail Clin 10(3):481–501
Bishu K, Deswal A, Chen HH, LeWinter MM, Lewis GD, Semigran MJ, Borlaug BA, McNulty S, Hernandez AF, Braunwald E, Redfield MM (2012) Biomarkers in acutely decompensated heart failure with preserved or reduced ejection fraction. Am Heart J 164(5)
Ariyaratnam JP, Lau DH, Sanders P, Kalman JM (2021) Atrial fibrillation and heart failure: epidemiology, pathophysiology, prognosis, and management. Card Electrophysiol Clin 13(1):47–62
Mentz RJ, Kelly JP, von Lueder TG, Voors AA, Lam CSP, Cowie MR, Kjeldsen K, Jankowska EA, Atar D, Butler J, Fiuzat M, Zannad F, Pitt B, O’Connor CM (2014) Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol 64(21):2281–2293
Hanna A, Frangogiannis NG (2020) Inflammatory cytokines and chemokines as therapeutic targets in heart failure. Cardiovasc Drugs Ther 34(6):849–863
Paulus WJ, Tschöpe C (2013) A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol 62(4):263–271
Knackstedt C, Gramley F, Schimpf T, Mischke K, Zarse M, Plisiene J, Schmid M, Lorenzen J, Frechen D, Neef P, Hanrath P, Kelm M, Schauerte P (2008) Association of echocardiographic atrial size and atrial fibrosis in a sequential model of congestive heart failure and atrial fibrillation. Cardiovasc Pathol 17(5):318–324
Sanders P, Morton JB, Davidson NC, Spence SJ, Vohra JK, Sparks PB, Kalman JM (2003) Electrical remodeling of the atria in congestive heart failure: electrophysiological and electroanatomic mapping in humans. Circulation 108(12):1461–1468
Kitzman DW, Little WC, Brubaker PH, Anderson RT, Hundley WG, Marburger CT, Brosnihan B, Morgan TM, Stewart KP (2002) Pathophysiological characterization of isolated diastolic heart failure in comparison to systolic heart failure. JAMA 288(17):2144–2150
Harada D, Asanoi H, Noto T, Takagawa J (2020) Different pathophysiology and outcomes of heart failure with preserved ejection fraction stratified by k-means clustering. Front Cardiovasc Med 7:607760
Vaduganathan M, Piccini JP, Camm AJ, Crijns HJGM, Anker SD, Butler J, Stewart J, Braceras R, Albuquerque APA, Wieloch M, Hohnloser SH (2022) Dronedarone for the treatment of atrial fibrillation with concomitant heart failure with preserved and mildly reduced ejection fraction: a post-hoc analysis of the ATHENA trial. Eur J Heart Fail 24(6):1094–1101
Rahbar Kouibaran F, Sabatino M, Barozzi C, Diemberger I (2023) Atrial natriuretic peptides as a bridge between atrial fibrillation, heart failure, and amyloidosis of the atria. Int J Mol Sci 24(7)
Shantsila E, Shantsila A, Blann AD, Lip GYH (2013) Left ventricular fibrosis in atrial fibrillation. Am J Cardiol 111(7)
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A (2021) 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42(36):3599–3726
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM, Evers LR, Fang JC, Fedson SE, Fonarow GC, Hayek SS, Hernandez AF, Khazanie P, Kittleson MM, Lee CS, Link MS, Milano CA, Nnacheta LC, Sandhu AT, Stevenson LW, Vardeny O, Vest AR, Yancy CW (2022) 2022 AHA/ACC/HFSA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 145(18):e876–e894
Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L, Merkely B, Pokushalov E, Sanders P, Proff J, Schunkert H, Christ H, Vogt J, Bänsch D (2018) Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 378(5):417–427
Packer DL, Mark DB, Robb RA, Monahan KH, Bahnson TD, Poole JE, Noseworthy PA, Rosenberg YD, Jeffries N, Mitchell LB, Flaker GC, Pokushalov E, Romanov A, Bunch TJ, Noelker G, Ardashev A, Revishvili A, Wilber DJ, Cappato R, Kuck K-H, Hindricks G, Davies DW, Kowey PR, Naccarelli GV, Reiffel JA, Piccini JP, Silverstein AP, Al-Khalidi HR, Lee KL (2019) Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 321(13):1261–1274
Di Biase L, Mohanty P, Mohanty S, Santangeli P, Trivedi C, Lakkireddy D, Reddy M, Jais P, Themistoclakis S, Dello Russo A, Casella M, Pelargonio G, Narducci ML, Schweikert R, Neuzil P, Sanchez J, Horton R, Beheiry S, Hongo R, Hao S, Rossillo A, Forleo G, Tondo C, Burkhardt JD, Haissaguerre M, Natale A (2016) Ablation versus amiodarone for treatment of persistent atrial fibrillation in patients with congestive heart failure and an implanted device: results from the AATAC multicenter randomized trial. Circulation 133(17):1637–1644
Nassif ME, Windsor SL, Borlaug BA, Kitzman DW, Shah SJ, Tang F, Khariton Y, Malik AO, Khumri T, Umpierrez G, Lamba S, Sharma K, Khan SS, Chandra L, Gordon RA, Ryan JJ, Chaudhry S-P, Joseph SM, Chow CH, Kanwar MK, Pursley M, Siraj ES, Lewis GD, Clemson BS, Fong M, Kosiborod MN (2021) The SGLT2 inhibitor dapagliflozin in heart failure with preserved ejection fraction: a multicenter randomized trial. Nat Med 27(11):1954–1960
Butler J, Filippatos G, Jamal Siddiqi T, Brueckmann M, Böhm M, Chopra VK, Pedro Ferreira J, Januzzi JL, Kaul S, Piña IL, Ponikowski P, Shah SJ, Senni M, Vedin O, Verma S, Peil B, Pocock SJ, Zannad F, Packer M, Anker SD (2022) Empagliflozin, Health status, and quality of life in patients with heart failure and preserved ejection fraction: the EMPEROR-preserved trial. Circulation 145(3):184–193
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, Martinez F, Packer M, Pfeffer MA, Pieske B, Redfield MM, Rouleau JL, van Veldhuisen DJ, Zannad F, Zile MR, Desai AS, Claggett B, Jhund PS, Boytsov SA, Comin-Colet J, Cleland J, Düngen HD, Goncalvesova E, Katova T, Kerr Saraiva JF, Lelonek M, Merkely B, Senni M, Shah SJ, Zhou J, Rizkala AR, Gong J, Shi VP, Lefkowitz MP (2019) Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med 381(17):1609–1620
Jia R, Zhang X, Xu Y, Zheng Z, Jiang L, Zhang X, Sun C, Wu X, Li S, Raj A, Sun D (2022) Effect of Sacubitril/Valsartan on renal function in patients with chronic kidney disease and heart failure with preserved ejection fraction: a real-world 12-week study. Eur J Pharmacol 928:175053
Silverman DN, Plante TB, Infeld M, Callas PW, Juraschek SP, Dougherty GB, Meyer M (2019) Association of β-blocker use with heart failure hospitalizations and cardiovascular disease mortality among patients with heart failure with a preserved ejection fraction: a secondary analysis of the TOPCAT trial. JAMA Netw Open 2(12):e1916598
Pfeffer MA, Claggett B, Assmann SF, Boineau R, Anand IS, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Heitner JF, Lewis EF, O’Meara E, Rouleau J-L, Probstfield JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, McKinlay SM, Pitt B (2015) Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial. Circulation 131(1):34–42
Kosiborod MN, Abildstrøm SZ, Borlaug BA, Butler J, Rasmussen S, Davies M, Hovingh GK, Kitzman DW, Lindegaard ML, Møller DV, Shah SJ, Treppendahl MB, Verma S, Abhayaratna W, Ahmed FZ, Chopra V, Ezekowitz J, Fu M, Ito H, Lelonek M, Melenovsky V, Merkely B, Núñez J, Perna E, Schou M, Senni M, Sharma K, Van der Meer P, von Lewinski D, Wolf D, Petrie MC (2023) Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N Engl J Med 389(12):1069–1084
Oikonomou E, Zografos T, Papamikroulis G-A, Siasos G, Vogiatzi G, Theofilis P, Briasoulis A, Papaioannou S, Vavuranakis M, Gennimata V, Tousoulis D (2019) Biomarkers in atrial fibrillation and heart failure. Curr Med Chem 26(5):873–887
Sepehrvand N, Alemayehu W, Dyck GJB, Dyck JRB, Anderson T, Howlett J, Paterson I, McAlister FA, Ezekowitz JA (2019) External validation of the H2F-PEF model in diagnosing patients with heart failure and preserved ejection fraction. Circulation 139(20):2377–2379
Sun Y, Si J, Li J, Dai M, King E, Zhang X, Zhang Y, Xia Y, Tse G, Liu Y (2021) Predictive value of HFA-PEFF score in patients with heart failure with preserved ejection fraction. Front Cardiovasc Med 8:656536
Reddy YNV, Kaye DM, Handoko ML, van de Bovenkamp AA, Tedford RJ, Keck C, Andersen MJ, Sharma K, Trivedi RK, Carter RE, Obokata M, Verbrugge FH, Redfield MM, Borlaug BA (2022) Diagnosis of heart failure with preserved ejection fraction among patients with unexplained dyspnea. JAMA Cardiol 7(9):891–899
Rajpurkar P, Lungren MP (2023) The current and future state of AI interpretation of medical images. N Engl J Med 388(21):1981–1990
Pandey A, Kagiyama N, Yanamala N, Segar MW, Cho JS, Tokodi M, Sengupta PP (2021) Deep-learning models for the echocardiographic assessment of diastolic dysfunction. JACC Cardiovasc Imaging 14(10):1887–1900
Segar MW, Patel KV, Ayers C, Basit M, Tang WHW, Willett D, Berry J, Grodin JL, Pandey A (2020) Phenomapping of patients with heart failure with preserved ejection fraction using machine learning-based unsupervised cluster analysis. Eur J Heart Fail 22(1):148–158
Woolley RJ, Ceelen D, Ouwerkerk W, Tromp J, Figarska SM, Anker SD, Dickstein K, Filippatos G, Zannad F, Metra M, Ng L, Samani N, van Veldhuisen DJ, Lang C, Lam CS, Voors AA (2021) Machine learning based on biomarker profiles identifies distinct subgroups of heart failure with preserved ejection fraction. Eur J Heart Fail 23(6):983–991
Liamis G, Megapanou E, Elisaf M, Milionis H (2019) Hyponatremia-inducing drugs. Front Horm Res 52:167–177
Verhaert DVM, Brunner-La Rocca HP, van Veldhuisen DJ, Vernooy K (2021) The bidirectional interaction between atrial fibrillation and heart failure: consequences for the management of both diseases. Europace 23(23 Suppl 2):ii40-ii45
Kao DP, Lewsey JD, Anand IS, Massie BM, Zile MR, Carson PE, McKelvie RS, Komajda M, McMurray JJV, Lindenfeld J (2015) Characterization of subgroups of heart failure patients with preserved ejection fraction with possible implications for prognosis and treatment response. Eur J Heart Fail 17(9):925–935
Law SWY, Lau WCY, Wong ICK, Lip GYH, Mok MT, Siu C-W, Chan EW (2018) Sex-based differences in outcomes of oral anticoagulation in patients with atrial fibrillation. J Am Coll Cardiol 72(3):271–282
Ilieșiu AM, Hodorogea AS (2018) Treatment of heart failure with preserved ejection fraction. Adv Exp Med Biol 1067:67–87
Omote K, Verbrugge FH, Borlaug BA (2022) Heart failure with preserved ejection fraction: mechanisms and treatment strategies. Annu Rev Med 73:321–337
Fukuta H, Goto T, Wakami K, Kamiya T, Ohte N (2021) Effect of beta-blockers on heart failure severity in patients with heart failure with preserved ejection fraction: a meta-analysis of randomized controlled trials. Heart Fail Rev 26(1):165–171
Neefs J, van den Berg NWE, Krul SPJ, Boekholdt SM, de Groot JR (2020) Effect of spironolactone on atrial fibrillation in patients with heart failure with preserved ejection fraction: post-hoc analysis of the randomized, placebo-controlled TOPCAT trial. Am J Cardiovasc Drugs 20(1):73–80
Parameswaran R, Al-Kaisey AM, Kalman JM (2021) Catheter ablation for atrial fibrillation: current indications and evolving technologies. Nat Rev Cardiol 18(3):210–225
Rattka M, Kühberger A, Pott A, Stephan T, Weinmann K, Baumhardt M, Aktolga D, Teumer Y, Bothner C, Scharnbeck D, Rottbauer W, Dahme T (2021) Catheter ablation for atrial fibrillation in HFpEF patients-a propensity-score-matched analysis. J Cardiovasc Electrophysiol 32(9):2357–2367
Gu G, Wu J, Gao X, Liu M, Jin C, Xu Y (2022) Catheter ablation of atrial fibrillation in patients with heart failure and preserved ejection fraction: a meta-analysis. Clin Cardiol 45(7):786–793
Packer DL, Piccini JP, Monahan KH, Al-Khalidi HR, Silverstein AP, Noseworthy PA, Poole JE, Bahnson TD, Lee KL, Mark DB (2021) Ablation Versus drug therapy for atrial fibrillation in heart failure: results from the CABANA trial. Circulation 143(14):1377–1390
Di Monaco A, Vitulano N, Troisi F, Quadrini F, Romanazzi I, Calvi V, Grimaldi M (2022) Pulsed field ablation to treat atrial fibrillation: a review of the literature. J Cardiovasc Dev Dis 9(4)
Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM, Barrabés JA, Boriani G, Braunschweig F, Brignole M, Burri H, Coats AJS, Deharo JC, Delgado V, Diller G-P, Israel CW, Keren A, Knops RE, Kotecha D, Leclercq C, Merkely B, Starck C, Thylén I, Tolosana JM, Leyva F, Linde C, Abdelhamid M, Aboyans V, Arbelo E, Asteggiano R, Barón-Esquivias G, Bauersachs J, Biffi M, Birgersdotter-Green U, Bongiorni MG, Borger MA, Čelutkienė J, Cikes M, Daubert JC, Drossart I, Ellenbogen K, Elliott PM, Fabritz L, Falk V, Fauchier L, Fernández-Avilés F, Foldager D, Van Gadler F, De Vinuesa PGG, Gorenek B, Guerra JM, Hermann Haugaa K, Hendriks J, Kahan T, Katus HA, Konradi A, Koskinas KC, Law H, Lewis BS, Linker NJ, Løchen ML, Lumens J, Mascherbauer J, Mullens W, Nagy KV, Prescott E, Raatikainen P, Rakisheva A, Reichlin T, Ricci RP, Shlyakhto E, Sitges M, Sousa-Uva M, Sutton R, Suwalski P, Svendsen JH, Touyz RM, Gelder IC, Vernooy K, Waltenberger J, Whinnett Z, Witte KK (2022) 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Europace 24(1)
Ahmed T (2020) Heart failure with preserved ejection fraction: can device therapy be our option? Cureus 12(3):e7323
Verbrugge FH, Verhaert D, Grieten L, Dupont M, Rivero-Ayerza M, De Vusser P, Van Herendael H, Reyskens R, Vandervoort P, Tang WHW, Mullens W (2013) Revisiting diastolic filling time as mechanistic insight for response to cardiac resynchronization therapy. Europace 15(12):1747–1756
Steendijk P, Tulner SA, Bax JJ, Oemrawsingh PV, Bleeker GB, van Erven L, Putter H, Verwey HF, van der Wall EE, Schalij MJ (2006) Hemodynamic effects of long-term cardiac resynchronization therapy: analysis by pressure-volume loops. Circulation 113(10):1295–1304
Penicka M, Kocka V, Herman D, Trakalova H, Herold M (2010) Cardiac resynchronization therapy for the causal treatment of heart failure with preserved ejection fraction: insight from a pressure-volume loop analysis. Eur J Heart Fail 12(6):634–636
Daubert C, Behar N, Martins RP, Mabo P, Leclercq C (2017) Avoiding non-responders to cardiac resynchronization therapy: a practical guide. Eur Heart J 38(19):1463–1472
Bertini M, Mele D, Malagù M, Fiorencis A, Toselli T, Casadei F, Cannizzaro T, Fragale C, Fucili A, Campagnolo E, Benea G, Ferrari R (2016) Cardiac resynchronization therapy guided by multimodality cardiac imaging. Eur J Heart Fail 18(11):1375–1382
Sweeney MO, Hellkamp AS, Ellenbogen KA, Greenspon AJ, Freedman RA, Lee KL, Lamas GA (2003) Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation 107(23):2932–2937
Sharma PS, Vijayaraman P, Ellenbogen KA (2020) Permanent His bundle pacing: shaping the future of physiological ventricular pacing. Nat Rev Cardiol 17(1):22–36
Hua J, Wang C, Kong Q, Zhang Y, Wang Q, Xiong Z, Hu J, Li J, Chen Q, Hong K (2022) Comparative effects of left bundle branch area pacing, His bundle pacing, biventricular pacing in patients requiring cardiac resynchronization therapy: A network meta-analysis. Clin Cardiol 45(2):214–223
Huang W, Su L, Wu S, Xu L, Xiao F, Zhou X, Ellenbogen KA (2017) Benefits of permanent his bundle pacing combined with atrioventricular node ablation in atrial fibrillation patients with heart failure with both preserved and reduced left ventricular ejection fraction. J Am Heart Assoc 6(4)
Hua J, Kong Q, Chen Q (2022) Alternative pacing strategies for optimal cardiac resynchronization therapy. Front Cardiovasc Med 9:923394
Upadhyay GA, Vijayaraman P, Nayak HM, Verma N, Dandamudi G, Sharma PS, Saleem M, Mandrola J, Genovese D, Tung R (2019) His corrective pacing or biventricular pacing for cardiac resynchronization in heart failure. J Am Coll Cardiol 74(1):157–159
Zhang S, Zhou X, Gold MR (2019) Left bundle branch pacing: JACC review topic of the week. J Am Coll Cardiol 74(24):3039–3049
Wu S, Su L, Vijayaraman P, Zheng R, Cai M, Xu L, Shi R, Huang Z, Whinnett ZI, Huang W (2021) left bundle branch pacing for cardiac resynchronization therapy: nonrandomized on-treatment comparison With His bundle pacing and biventricular pacing. Can J Cardiol 37(2):319–328
Wang Y, Zhu H, Hou X, Wang Z, Zou F, Qian Z, Wei Y, Wang X, Zhang L, Li X, Liu Z, Xue S, Qin C, Zeng J, Li H, Wu H, Ma H, Ellenbogen KA, Gold MR, Fan X, Zou J (2022) Randomized trial of left bundle branch vs biventricular pacing for cardiac resynchronization therapy. J Am Coll Cardiol 80(13):1205–1216
Cai M, Wu S, Wang S, Zheng R, Jiang L, Lian L, He Y, Zhu L, Xu L, Ellenbogen KA, Whinnett ZI, Su L, Huang W (2022) Left bundle branch pacing postatrioventricular junction ablation for atrial fibrillation: propensity score matching with His bundle pacing. Circ Arrhythm Electrophysiol 15(10):e010926
Talha KM, Anker SD, Burkhoff D, Filippatos G, Lam CSP, Stone GW, Wazni O, Butler J (2022) Role of cardiac contractility modulation in heart failure with a higher ejection fraction. J Card Fail 28(12):1717–1726
Chinyere IR, Balakrishnan M, Hutchinson MD (2022) The emerging role of cardiac contractility modulation in heart failure treatment. Curr Opin Cardiol 37(1):30–35
Abraham WT, Kuck K-H, Goldsmith RL, Lindenfeld J, Reddy VY, Carson PE, Mann DL, Saville B, Parise H, Chan R, Wiegn P, Hastings JL, Kaplan AJ, Edelmann F, Luthje L, Kahwash R, Tomassoni GF, Gutterman DD, Stagg A, Burkhoff D, Hasenfuß G (2018) A randomized controlled trial to evaluate the safety and efficacy of cardiac contractility modulation. JACC Heart Fail 6(10):874–883
Tschöpe C, Kherad B, Klein O, Lipp A, Blaschke F, Gutterman D, Burkhoff D, Hamdani N, Spillmann F, Van Linthout S (2019) Cardiac contractility modulation: mechanisms of action in heart failure with reduced ejection fraction and beyond. Eur J Heart Fail 21(1):14–22
Tschöpe C, Van Linthout S, Spillmann F, Klein O, Biewener S, Remppis A, Gutterman D, Linke WA, Pieske B, Hamdani N, Roser M (2016) Cardiac contractility modulation signals improve exercise intolerance and maladaptive regulation of cardiac key proteins for systolic and diastolic function in HFpEF. Int J Cardiol 203:1061–1066
Linde C, Grabowski M, Ponikowski P, Rao I, Stagg A, Tschöpe C (2022) Cardiac contractility modulation therapy improves health status in patients with heart failure with preserved ejection fraction: a pilot study (CCM-HFpEF). Eur J Heart Fail 24(12):2275–2284
Röger S, Borggrefe M, Kuschyk J (2015) Heart failure with reduced ejection fraction and a narrow QRS complex: combination of a subcutaneous defibrillator with cardiac contractility modulation. J Atr Fibrillation 8(3):1081
Röger S, Schneider R, Rudic B, Liebe V, Stach K, Schimpf R, Borggrefe M, Kuschyk J (2014) Cardiac contractility modulation: first experience in heart failure patients with reduced ejection fraction and permanent atrial fibrillation. Europace 16(8):1205–1209
Karatela MF, Fudim M, Mathew JP, Piccini JP (2023) Neuromodulation therapy for atrial fibrillation. Heart Rhythm 20(1):100–111
Manolis AA, Manolis TA, Apostolopoulos EJ, Apostolaki NE, Melita H, Manolis AS (2021) The role of the autonomic nervous system in cardiac arrhythmias: The neuro-cardiac axis, more foe than friend? Trends Cardiovasc Med 31(5):290–302
Chen P-S, Chen LS, Fishbein MC, Lin S-F, Nattel S (2014) Role of the autonomic nervous system in atrial fibrillation: pathophysiology and therapy. Circ Res 114(9):1500–1515
Hanna P, Buch E, Stavrakis S, Meyer C, Tompkins JD, Ardell JL, Shivkumar K (2021) Neuroscientific therapies for atrial fibrillation. Cardiovasc Res 117(7):1732–1745
Linz D, Ukena C, Mahfoud F, Neuberger H-R, Böhm M (2014) Atrial autonomic innervation: a target for interventional antiarrhythmic therapy? J Am Coll Cardiol 63(3):215–224
Capilupi MJ, Kerath SM, Becker LB (2020) Vagus nerve stimulation and the cardiovascular system. Cold Spring Harb Perspect Med 10(2)
Yuan H, Silberstein SD (2016) Vagus nerve and vagus nerve stimulation, a comprehensive review: Part II. Headache 56(2):259–266
Tracey KJ (2002) The inflammatory reflex. Nature 420(6917):853–859
Stavrakis S, Humphrey MB, Scherlag BJ, Hu Y, Jackman WM, Nakagawa H, Lockwood D, Lazzara R, Po SS (2015) Low-level transcutaneous electrical vagus nerve stimulation suppresses atrial fibrillation. J Am Coll Cardiol 65(9):867–875
Stavrakis S, Humphrey MB, Scherlag B, Iftikhar O, Parwani P, Abbas M, Filiberti A, Fleming C, Hu Y, Garabelli P, McUnu A, Peyton M, Po SS (2017) Low-level vagus nerve stimulation suppresses post-operative atrial fibrillation and inflammation: a randomized study. JACC Clin Electrophysiol 3(9):929–938
Sun Y, Chao S, Ouyang H, Zhang W, Luo W, Nie Q, Wang J, Luo C, Ni G, Zhang L, Yang J, Feng H, Mao G, Li Z (2022) Hybrid nanogenerator based closed-loop self-powered low-level vagus nerve stimulation system for atrial fibrillation treatment. Sci Bull (Beijing) 67(12):1284–1294
Elkholey K, Niewiadomska M, Morris L, Whyte S, Houser J, Humphrey MB, Stavrakis S (2022) Transcutaneous vagus nerve stimulation ameliorates the phenotype of heart failure with preserved ejection fraction through its anti-inflammatory effects. Circ Heart Fail 15(8):e009288
Stavrakis S, Elkholey K, Morris L, Niewiadomska M, Asad ZUA, Humphrey MB (2022) Neuromodulation of inflammation to treat heart failure with preserved ejection fraction: a pilot randomized clinical trial. J Am Heart Assoc 11(3):e023582
Parra-Lucares A, Romero-Hernández E, Villa E, Weitz-Muñoz S, Vizcarra G, Reyes M, Vergara D, Bustamante S, Llancaqueo M, Toro L (2022) New opportunities in heart failure with preserved ejection fraction: from bench to bedside… and back. Biomedicines 11(1)
Rosalia L, Ozturk C, Shoar S, Fan Y, Malone G, Cheema FH, Conway C, Byrne RA, Duffy GP, Malone A, Roche ET, Hameed A (2021) Device-based solutions to improve cardiac physiology and hemodynamics in heart failure with preserved ejection fraction. JACC Basic Transl Sci 6(9–10):772–795
Feld Y, Dubi S, Reisner Y, Schwammenthal E, Shofti R, Pinhasi A, Carasso S, Elami A (2011) Energy transfer from systole to diastole: a novel device-based approach for the treatment of diastolic heart failure. Acute Card Care 13(4):232–242
Feld Y, Reisner Y, Meyer-Brodnitz G, Hoefler R (2023) The CORolla device for energy transfer from systole to diastole: a novel treatment for heart failure with preserved ejection fraction. Heart Fail Rev 28(2):307–314
Mc Morrow R, Kriza C, Urbán P, Amenta V, Amaro JAB, Panidis D, Chassaigne H, Griesinger CB (2020) Assessing the safety and efficacy of TAVR compared to SAVR in low-to-intermediate surgical risk patients with aortic valve stenosis: an overview of reviews. Int J Cardiol 314:43–53
Sodhi N, Asch FM, Ruf T, Petrescu A, von Bardeleben S, Lim DS, Maisano F, Kar S, Price MJ (2022) Clinical outcomes with transcatheter edge-to-edge repair in atrial functional MR from the EXPAND study. JACC Cardiovasc Interv 15(17):1723–1730
Al-Khadra Y, Sattar Y, Ullah W, Moussa Pacha H, Baibars M, Darmoch F, Abu-Mahfouz M, Afonso L, Devireddy C, Anwaruddin S, Sorajja P, Ajmal R, Kwok CS, Asfour AI, Zehr K, Mamas MA, Alraies MC (2021) Temporal trends and outcomes in utilisation of transcatheter and surgical aortic valve therapies in aortic valve stenosis patients with heart failure. Int J Clin Pract 75(3):e13711
Dong M, Wang L, Tse G, Dai T, Wang L, Xiao Z, Liu T, Ren F (2023) Effectiveness and safety of transcatheter aortic valve replacement in elderly people with severe aortic stenosis with different types of heart failure. BMC Cardiovasc Disord 23(1):34
Tarantini G, Mojoli M, Windecker S, Wendler O, Lefèvre T, Saia F, Walther T, Rubino P, Bartorelli AL, Napodano M, D’Onofrio A, Gerosa G, Iliceto S, Vahanian A (2016) Prevalence and impact of atrial fibrillation in patients with severe aortic stenosis undergoing transcatheter aortic valve replacement: an analysis from the SOURCE XT prospective multicenter registry. JACC Cardiovasc Interv 9(9):937–946
Gröger M, Scheffler JK, Schösser F, Schneider LM, Rottbauer W, Markovic S, Keßler M (2021) Percutaneous edge-to-edge mitral valve repair for mitral regurgitation improves heart failure symptoms in heart failure with preserved ejection fraction patients. ESC Heart Fail 8(6):5010–5021
Popolo Rubbio A, Testa L, Grasso C, Sisinni A, Tusa M, Agricola E, De Marco F, Petronio AS, Montorfano M, Citro R, Adamo M, Mangieri A, Casenghi M, Milici AL, Stazzoni L, Colombo A, Tamburino C, Bedogni F (2022) Transcatheter edge-to-edge mitral valve repair in atrial functional mitral regurgitation: insights from the multi-center MITRA-TUNE registry. Int J Cardiol 349:39–45
Stone GW, Abraham WT, Lindenfeld J, Kar S, Grayburn PA, Lim DS, Mishell JM, Whisenant B, Rinaldi M, Kapadia SR, Rajagopal V, Sarembock IJ, Brieke A, Marx SO, Cohen DJ, Asch FM, Mack MJ (2023) Five-year follow-up after transcatheter repair of secondary mitral regurgitation. N Engl J Med 388(22):2037–2048
Mascherbauer J, Kammerlander AA, Zotter-Tufaro C, Aschauer S, Duca F, Dalos D, Winkler S, Schneider M, Bergler-Klein J, Bonderman D (2017) Presence of ´isolated´ tricuspid regurgitation should prompt the suspicion of heart failure with preserved ejection fraction. PLoS ONE 12(2):e0171542
Neuhold S, Huelsmann M, Pernicka E, Graf A, Bonderman D, Adlbrecht C, Binder T, Maurer G, Pacher R, Mascherbauer J (2013) Impact of tricuspid regurgitation on survival in patients with chronic heart failure: unexpected findings of a long-term observational study. Eur Heart J 34(11):844–852
Mutlak D, Lessick J, Reisner SA, Aronson D, Dabbah S, Agmon Y (2007) Echocardiography-based spectrum of severe tricuspid regurgitation: the frequency of apparently idiopathic tricuspid regurgitation. J Am Soc Echocardiogr 20(4):405–408
Topilsky Y, Inojosa JM, Benfari G, Vaturi O, Maltais S, Michelena H, Mankad S, Enriquez-Sarano M (2018) Clinical presentation and outcome of tricuspid regurgitation in patients with systolic dysfunction. Eur Heart J 39(39):3584–3592
Ton-Nu T-T, Levine RA, Handschumacher MD, Dorer DJ, Yosefy C, Fan D, Hua L, Jiang L, Hung J (2006) Geometric determinants of functional tricuspid regurgitation: insights from 3-dimensional echocardiography. Circulation 114(2):143–149
Kresoja K-P, Lauten A, Orban M, Rommel K-P, Alushi B, Besler C, Braun D, Unterhuber M, Stangl K, Landmesser U, Massberg S, Thiele H, Hausleiter J, Lurz P (2020) Transcatheter tricuspid valve repair in the setting of heart failure with preserved or reduced left ventricular ejection fraction. Eur J Heart Fail 22(10):1817–1825
Müller D, Remppis A, Schauerte P, Schmidt-Schweda S, Burkhoff D, Rousso B, Gutterman D, Senges J, Hindricks G, Kuck KH (2017) Clinical effects of long-term cardiac contractility modulation (CCM) in subjects with heart failure caused by left ventricular systolic dysfunction. Clin Res Cardiol 106(11):893–904
Witte K, Hasenfuss G, Kloppe A, Burkhoff D, Green M, Moss J, Peel A, Mealing S, Durand Zaleski I, Cowie MR (2019) Cost-effectiveness of a cardiac contractility modulation device in heart failure with normal QRS duration. ESC Heart Fail 6(6):1178–1187
Abdin A, Bauersachs J, Frey N, Kindermann I, Link A, Marx N, Lainscak M, Slawik J, Werner C, Wintrich J, Böhm M (2021) Timely and individualized heart failure management: need for implementation into the new guidelines. Clin Res Cardiol 110(8):1150–1158
Funding
This work was supported by the National Natural Science Foundation of China [no. 82070356, 81770337], the Key Project of Hunan Provincial Science and Technology Innovation [no. 2020SK1013], and the Hunan Provincial Natural Science Foundation of China [no. 2021JJ30033].
Author information
Authors and Affiliations
Contributions
Under the guidance of Professor Q. L., Y. X. collected relevant information, and Z. Z. wrote the manuscript, which was revised by Y. D. and Q. L. All authors contributed to the article and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
All authors participated in the study and made significant intellectual contributions to the manuscript.
Consent for publication
The manuscript is not currently under consideration elsewhere, and the work reported will not be submitted for publication elsewhere until a final decision has been made as to its acceptability by the Journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Z., Xiao, Y., Dai, Y. et al. Device therapy for patients with atrial fibrillation and heart failure with preserved ejection fraction. Heart Fail Rev 29, 417–430 (2024). https://doi.org/10.1007/s10741-023-10366-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-023-10366-7