Abstract
Purpose
Photoplethysmography measurement of heart rate with wrist-worn trackers has been introduced in healthy individuals. However, additional consideration is necessary for patients with ischemic heart disease, and the available evidence is limited. The study aims to evaluate the validity and reliability of heart rate measures by a wrist-worn photoplethysmography (PPG) tracker compared to an electrocardiogram (ECG) during incremental treadmill exercise among patients with ischemic heart disease.
Methods
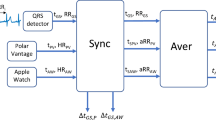
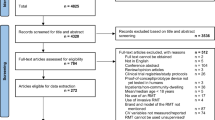
Fifty-one participants performed the standard incremental treadmill exercise in a controlled laboratory setting with 12-lead ECG attached to the patient's body and wearing wrist-worn PPG trackers.
Results
At each stage, the absolute percentage error of the PPG was within 10% of the standard acceptable range. Further analysis using a linear mixed model, which accounts for individual variations, revealed that PPG yielded the best performance at the baseline low-intensity exercise. As the stages progressed, heart rate validity decreased but was regained during recovery. The reliability was moderate to excellent.
Conclusions
Low-cost trackers AMAZFIT Cor and Bip validity and reliability were within acceptable ranges, especially during low-intensity exercise among patients with ischemic heart disease recovering from cardiac procedures. Though using the tracker as part of the diagnosis tool still requires more supporting studies, it can potentially be used as a self-monitoring tool with precautions.



Similar content being viewed by others
References
Paxton, M. Wearable Tech Fitness trackers on the rebound. 2020.
International Data Corporation. Shipments of Wearable Devices Reach 118.9 Million Units in the Fourth Quarter and 336.5 Million for 2019. Retrieved from https://www.idc.com/getdoc.jsp?containerId=prUS46122120
Research, G.V. Wearable Technology Market Size, Share & Trends Analysis Report By Product (Head & Eyewear, Wristwear), By Application (Consumer Electronics, Healthcare), By Region (Asia Pacific, Europe), And Segment Forecasts, 2023-2030. 2023.
Thompson, W. R. Worldwide survey of fitness trends for 2020. ACSM’s Health Fitness J. 23(6):45, 2019.
Allen, J. Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 28(3):R1-39, 2007.
Plews, D. J., et al. Comparison of heart-rate-variability recording with smartphone photoplethysmography, polar H7 chest strap, and electrocardiography. Int. J. Sports Physiol. Perform. 12(10):1324–1328, 2017.
Jachymek, M., et al. Wristbands in home-based rehabilitation: validation of heart rate measurement. Sensors. 2022. https://doi.org/10.3390/s22010060.
Winzer Ephraim, B., F. Woitek, and A. Linke. Physical activity in the prevention and treatment of coronary artery disease. J. Am. Heart Assoc. 7(4):007725, 2018.
McMahon, S. R., P. A. Ades, and P. D. Thompson. The role of cardiac rehabilitation in patients with heart disease. Trends Cardiovasc. Med. 27(6):420–425, 2017.
Van Iterson, E. H., et al. Cardiac rehabilitation is essential in the COVID-19 era: delivering uninterrupted heart care based on the cleveland clinic experience. J. Cardiopulm. Rehabil. Prev. 41(2):88–92, 2021.
Wongvibulsin, S., et al. Digital health interventions for cardiac rehabilitation: systematic literature review. J. Med. Internet Res. 23(2):e18773, 2021.
Batalik, L., et al. Benefits and effectiveness of using a wrist heart rate monitor as a telerehabilitation device in cardiac patients: A randomized controlled trial. Medicine (Baltimore). 99(11):e19556, 2020.
Sapra, A., A. Malik, and P. Bhandari. Vital Sign Assessment, in StatPearls. 2022, StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.: Treasure Island (FL).
Munos, B., et al. Mobile health: the power of wearables, sensors, and apps to transform clinical trials. Ann. N. Y. Acad. Sci. 1375(1):3–18, 2016.
Germini, F., et al. Accuracy and acceptability of wrist-wearable activity-tracking devices: systematic review of the literature. J. Med. Internet Res. 24(1):e30791, 2022.
Fuller, D., et al. Reliability and validity of commercially available wearable devices for measuring steps, energy expenditure, and heart rate: systematic review. JMIR Mhealth Uhealth. 8(9):e18694, 2020.
Force, U. P. S. T. Screening for cardiovascular disease risk with electrocardiography: US preventive services task force recommendation statement. JAMA. 319(22):2308–2314, 2018.
Jeet. Amazfit beats Huawei to become the third-largest smartwatch brand globally. 2021; Available from: https://www.gizmochina.com/2021/11/30/amazfit-becomes-third-largest-smartwatch-brand/.
Cupertino, Amazfit Ranked Third in Global Smartwatch Shipments in Q3 2021. 2021.
Zhang, S., et al. The auxiliary diagnostic value of a novel wearable electrocardiogram-recording system for arrhythmia detection: diagnostic trial. Front Med (Lausanne). 8:685999, 2021.
Düking, P., et al. Behavior change techniques in wrist-worn wearables to promote physical activity: content analysis. JMIR Mhealth Uhealth. 8(11):e20820, 2020.
Chen, E., et al. A new smart wristband equipped with an artificial intelligence algorithm to detect atrial fibrillation. Heart Rhythm. 17(5):847–853, 2020.
Rozanski, G. M., et al. Consumer wearable devices for activity monitoring among individuals after a stroke: a prospective comparison. JMIR Cardio. 2(1):e1, 2018.
Sprint, G., et al. Analyzing sensor-based time series data to track changes in physical activity during inpatient rehabilitation. Sensors (Basel). 17(10):48, 2017.
Falter, M., et al. Accuracy of apple watch measurements for heart rate and energy expenditure in patients with cardiovascular disease: cross-sectional study. JMIR mHealth uHealth. 7(3):e11889–e11889, 2019.
Etiwy, M., et al. Accuracy of wearable heart rate monitors in cardiac rehabilitation. Cardiovasc Diagn Ther. 9(3):262–271, 2019.
Mühlen, J. M., et al. Recommendations for determining the validity of consumer wearable heart rate devices: expert statement and checklist of the INTERLIVE Network. Br. J. Sports Med. 55(14):767, 2021.
O’Driscoll, R., et al. The validity of two widely used commercial and research-grade activity monitors, during resting, household and activity behaviours. Health Technol. 10(3):637–648, 2020.
Shumate, T., et al. Validity of the Polar Vantage M watch when measuring heart rate at different exercise intensities. PeerJ. 9:e10893, 2021.
Fan, Y. Y., et al. Diagnostic performance of a smart device with photoplethysmography technology for atrial fibrillation detection: pilot study (Pre-mAFA II registry). JMIR Mhealth Uhealth. 7(3):e11437, 2019.
Inui, T., et al. Use of a smart watch for early detection of paroxysmal atrial fibrillation: validation study. JMIR Cardio. 4(1):e14857, 2020.
Kooiman, T. J. M., et al. Reliability and validity of ten consumer activity trackers. BMC Sports Sci. Med. Rehabil. 7:24, 2015. https://doi.org/10.1186/s13102-015-0018-5.
Shcherbina, A., et al. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J. Person. Med. 7(2):48, 2017.
Gordon, W. J., and R. S. Rudin. Why APIs? Anticipated value, barriers, and opportunities for standards-based application programming interfaces in healthcare: perspectives of US thought leaders. JAMIA Open. 5(2):023, 2022.
Dullabh, P., et al. Application programming interfaces in health care: findings from a current-state sociotechnical assessment. Appl. Clin. Inform. 11(1):59–69, 2020.
Thiebaud, R. S., et al. Validity of wrist-worn consumer products to measure heart rate and energy expenditure. Digital Health. 4:2055207618770322, 2018.
Harb, S. C., et al. Prognostic value of functional capacity in different exercise protocols. J. Am. Heart Assoc. 9(13):e015986, 2020.
Fitzpatrick, T. B. The validity and practicality of sun-reactive skin types I through VI. Arch. Dermatol. 124(6):869–871, 1988.
MD-Isa, Z., et al. The reliability of Fitzpatrick Skin Type Chart Comparing to Mexameter (Mx 18) in measuring skin color among first trimester pregnant mothers in Petaling District Malaysia. . Malays. J. Public Health Med. 16:59–65, 2016.
Meteyard, L., and R. A. I. Davies. Best practice guidance for linear mixed-effects models in psychological science. J. Mem. Language. 112:104092, 2020.
Liljequist, D., B. Elfving, and K. S. Roaldsen. Intraclass correlation: a discussion and demonstration of basic features. PLoS ONE. 14(7):0219854, 2019.
Portney, L.G. and M.P. Watkins. Foundations of clinical research: applications to practice. Vol. 892. 2009: Pearson/Prentice Hall Upper Saddle River, NJ.
Chen, G., et al. Intraclass correlation: Improved modeling approaches and applications for neuroimaging. Hum. Brain Map. 39(3):1187–1206, 2018.
Taylor, J. L., A. R. Bonikowske, and T. P. Olson. Optimizing outcomes in cardiac rehabilitation: the importance of exercise intensity. Front. Cardiovasc. Med. 8:734278, 2021.
Dooley, E. E., N. M. Golaszewski, and J. B. Bartholomew. Estimating accuracy at exercise intensities: a comparative study of self-monitoring heart rate and physical activity wearable devices. JMIR Mhealth Uhealth. 5(3):e34, 2017.
Gillinov, A. M., et al. Variable accuracy of commercially available wearable heart rate monitors. J. Am. Coll. Cardiol. 69(11):336, 2017.
Kobayashi, M., T. Shinohara, and S. Usuda. Accuracy of wrist-worn heart rate monitors during physical therapy sessions among hemiparetic inpatients with stroke. J. Phys. Therapy Sci. 33(1):45–51, 2021.
Jachymek, M., et al. Wristbands in home-based rehabilitation-validation of heart rate measurement. Sensors (Basel). 22(1):7, 2021.
Chow, H. W., and C. C. Yang. Accuracy of optical heart rate sensing technology in wearable fitness trackers for young and older adults: validation and comparison study. JMIR Mhealth Uhealth. 8(4):e14707, 2020.
Fokkema, T., et al. Reliability and validity of ten consumer activity trackers depend on walking speed. Med Sci Sports Exerc. 49(4):793–800, 2017.
Nelson, M. B., et al. Validity of consumer-based physical activity monitors for specific activity types. Med. Sci. Sports Exerc. 48(8):1619–1628, 2016.
Chowdhury, E. A., et al. Assessment of laboratory and daily energy expenditure estimates from consumer multi-sensor physical activity monitors. PLoS ONE. 12(2):e0171720, 2017.
Hoevenaars, D., et al. Accuracy of heart rate measurement by the fitbit charge 2 during wheelchair activities in people with spinal cord injury: instrument validation study. JMIR Rehabil. Assist. Technol. 9(1):e27637, 2022.
Nelson, B. W., and N. B. Allen. Accuracy of consumer wearable heart rate measurement during an ecologically valid 24-hour period: intraindividual validation study. JMIR Mhealth Uhealth. 7(3):e10828, 2019.
Sjöberg, V., et al. Wrist-worn activity trackers in laboratory and free-living settings for patients with chronic pain: criterion validity study. JMIR Mhealth Uhealth. 9(1):e24806, 2021.
Bent, B., et al. Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ. Digital Med. 3(1):18, 2020.
Alzahrani, A., et al. A multi-channel opto-electronic sensor to accurately monitor heart rate against motion artefact during exercise. Sensors (Basel, Switzerland). 15(10):25681–25702, 2015.
Sartor, F., et al. Wrist-worn optical and chest strap heart rate comparison in a heterogeneous sample of healthy individuals and in coronary artery disease patients. BMC Sports Sci. Med. Rehabil. 10(1):10, 2018.
Gillinov, S., et al. Variable accuracy of wearable heart rate monitors during aerobic exercise. Med. Sci. Sports Exerc. 49(8):1697–1703, 2017.
Wang, R., et al. Accuracy of wrist-worn heart rate monitors. JAMA Cardiol. 2(1):104–106, 2017.
Bunn, J. A., et al. Current state of commercial wearable technology in physical activity monitoring 2015–2017. Int. J. Exercise Sci. 11(7):503–515, 2018.
Stone, J. D., et al. Assessing the accuracy of popular commercial technologies that measure resting heart rate and heart rate variability. Front. Sports Act. Living. 3:585870, 2021.
Nelson, B. W., et al. Guidelines for wrist-worn consumer wearable assessment of heart rate in biobehavioral research. NPJ Digital Med. 3(1):90, 2020.
Spadaccio, C., and U. Benedetto. Coronary artery bypass grafting (CABG) vs percutaneous coronary intervention (PCI) in the treatment of multivessel coronary disease: quo vadis? -a review of the evidences on coronary artery disease. Ann. Cardiothorac. Surg. 7(4):506–515, 2018.
Stahl, S. E., et al. How accurate are the wrist-based heart rate monitors during walking and running activities? Are they accurate enough? BMJ Open Sport Exercise Med. 2(1):e000106, 2016.
Boudreaux, B. D., et al. Validity of wearable activity monitors during cycling and resistance exercise. Med. Sci. Sports Exercise. 50(3):8, 2018.
Jo, E., et al. Validation of biofeedback wearables for photoplethysmographic heart rate tracking. J. Sports Sci. Med. 15(3):540–547, 2016.
Dondzila, C. J., et al. Congruent accuracy of wrist-worn activity trackers during controlled and free-living conditions. Int. J. Exercise Sci. 11:575–584, 2018.
Hannan, M., et al. Behavioral medicine for sedentary behavior, daily physical activity, and exercise to prevent cardiovascular disease: a review. Curr. Atheroscler. Rep. 23(9):48, 2021.
Wallen, M. P., et al. Accuracy of heart rate watches: implications for weight management. PLoS ONE. 11(5):e0154420, 2016.
Degroote, L., et al. Low-cost consumer-based trackers to measure physical activity and sleep duration among adults in free-living conditions: validation study. JMIR Mhealth Uhealth, 8(5):e16674, 2020.
Delgado-Gonzalo, R., et al. Evaluation of accuracy and reliability of PulseOn optical heart rate monitoring device. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2015:430–433, 2015.
Tang, M. S. S., et al. Effectiveness of Wearable trackers on physical activity in healthy adults: systematic review and meta-analysis of randomized controlled trials. JMIR mHealth and uHealth. 8(7):e15576–e15576, 2020.
Dagan, A., and O. J. Mechanic. Use of ultra-low cost fitness trackers as clinical monitors in low resource emergency departments. Clin. Exp. Emergency Med. 7(3):144–149, 2020.
Bai, Y., et al. Comparative evaluation of heart rate-based monitors: apple watch vs fitbit charge HR. J. Sports Sci. 36(15):1734–1741, 2018.
Acknowledgements
The study was partially funded by a Research Grant from the Universiti Malaya (RF009C-2018). Any other parties provided no other grants or funds. Special thanks to all the participants from the Universiti Malaya Medical Centre (UMMC) Rehabilitation Medicine Clinic and the UMMC Stress Test Lab physicians and technicians for their assistance in data collection.
Author information
Authors and Affiliations
Contributions
AS, RS, WLL, and NSI have contributed substantially to the research design, NSI collecting of the data, NSI and RS analyzing and interpreting the data. NSI and EWP have participated in drafting the manuscript. All authors have read and approved the final version.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Additional information
Associate Editor Christian Zemlin oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ibrahim, N.S., Rampal, S., Lee, W.L. et al. Evaluation of Wrist-Worn Photoplethysmography Trackers with an Electrocardiogram in Patients with Ischemic Heart Disease: A Validation Study. Cardiovasc Eng Tech 15, 12–21 (2024). https://doi.org/10.1007/s13239-023-00693-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-023-00693-z