Abstract
Background
Tubular dysfunction can cause electrolyte disturbances with potentially serious consequences. We studied the epidemiology and outcomes of electrolyte disturbances and tubular dysfunction among critically ill children and evaluated their relationships with acute kidney injury (AKI).
Methods
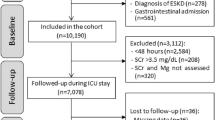
We conducted a prospective cohort study recruiting children aged 1 month to ≤ 18 years old admitted to the pediatric intensive care unit (PICU) from 6/2020 to 6/2021. The serum levels of sodium, potassium, calcium, phosphate, and magnesium were reviewed and simultaneous urinary investigations for tubular function were performed among children with electrolyte disturbances.
Results
Altogether there were 253 episodes of admission. The median (interquartile) age was 4.9 (1.3–11.0) years and 58.1% were male. The median number of electrolyte disorders was 3 (2–4) types. Hypophosphatemia (74.2%), hypocalcemia (70.3%) and hypermagnesemia (52.9%) were the three commonest types of disturbances. Urinary electrolyte wasting was commonly observed among children with hypomagnesemia (70.6%), hypophosphatemia (67.4%) and hypokalemia (28.6%). Tubular dysfunction was detected in 82.6% of patients and urinary β2-microglobulin level significantly correlated with the severity of tubular dysfunction (p < 0.001). The development of tubular dysfunction was independent of AKI status. Tubular dysfunction was associated with mortality (p < 0.001) and was an independent predictor of PICU length of stay (LOS) (p < 0.001). The incorporation of the tubular dysfunction severity into the AKI staging system improved the prediction of PICU LOS.
Conclusions
Tubular dysfunction was associated with both morbidity and mortality in critically ill children and its assessment may help to capture a more comprehensive picture of acute kidney insult.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information


Similar content being viewed by others
Data availability
The dataset generated for this publication is available from the corresponding author on reasonable request.
The authors declared that the submitted work was original. The study was presented in part at the 19th IPNA Congress 2022 but otherwise it has not been published elsewhere.
References
Buckley MS, Leblanc JM, Cawley MJ (2010) Electrolyte disturbances associated with commonly prescribed medications in the intensive care unit. Crit Care Med 38(6 Suppl):S253-264. https://doi.org/10.1097/CCM.0b013e3181dda0be
Elala G, Shimels D (2018) Patterns of electrolyte abnormalities in children 0–15 years of age admitted to pediatric emergency and intensive care units of a tertiary hospital. IOSR J Dental Med Sci 17:12–16
Naseem F, Saleem A, Mahar IA, Arif F (2019) Electrolyte imbalance in critically ill paediatric patients. Pak J Med Sci 35:1093–1098. https://doi.org/10.12669/pjms.35.4.286
Agarwal N, Saxena R, Acharya R (2018) Profile of serum electrolytes in critically Ill children: A prospective study. Indian J Child Health 5:128–132
Chary CR, Shalini B (2017) Correlation between serum electrolyte and clinical outcome in children admitted to PICU. IOSR J Dental Med Sci 16:24–27
Waite MD, Fuhrman SA, Badawi O, Zuckerman IH, Franey CS (2013) Intensive care unit-acquired hypernatremia is an independent predictor of increased mortality and length of stay. J Crit Care 28:405–412. https://doi.org/10.1016/j.jcrc.2012.11.013
McMahon GM, Mendu ML, Gibbons FK, Christopher KB (2012) Association between hyperkalemia at critical care initiation and mortality. Intensive Care Med 38:1834–1842. https://doi.org/10.1007/s00134-012-2636-7
Singhi SC, Singh J, Prasad R (2003) Hypocalcaemia in a paediatric intensive care unit. J Trop Pediatr 49:298–302. https://doi.org/10.1093/tropej/49.5.298
Şan ES, Erdoğan S, Boşnak M, Şan M (2017) Hypophosphatemia associated risk factors in pediatric intensive care patients. Turk J Pediatr 59:35–41. https://doi.org/10.24953/turkjped.2017.01.006
Shah SK, Irshad M, Gupta N, Kabra SK, Lodha R (2016) Hypophosphatemia in critically ill children: Risk factors, outcome and mechanism. Indian J Pediatr 83:1379–1385. https://doi.org/10.1007/s12098-016-2188-x
Upala S, Jaruvongvanich V, Wijarnpreecha K, Sanguankeo A (2016) Hypomagnesemia and mortality in patients admitted to intensive care unit: a systematic review and meta-analysis. QJM 109:453–459. https://doi.org/10.1093/qjmed/hcw048
Perazella MA (2019) Drug-induced acute kidney injury: diverse mechanisms of tubular injury. Curr Opin Crit Care 25:550–557. https://doi.org/10.1097/MCC.0000000000000653
Palmer BF (2015) Regulation of potassium homeostasis. Clin J Am Soc Nephrol 10:1050–1060. https://doi.org/10.2215/CJN.08580813
Jeon US (2008) Kidney and calcium homeostasis. Electrolyte Blood Press 6:68–76. https://doi.org/10.5049/EBP.2008.6.2.68
Prasad N, Bhadauria D (2013) Renal phosphate handling: Physiology. Indian J Endocrinol Metab 17:620–627. https://doi.org/10.4103/2230-8210.113752
Curry JN, Yu ASL (2018) Magnesium handling in the kidney. Adv Chronic Kidney Dis 25:236–243. https://doi.org/10.1053/j.ackd.2018.01.003
Bech A, Blans M, Telting D, de Boer H (2013) Incidence and aetiology of renal phosphate loss in patients with hypophosphatemia in the intensive care unit. Intensive Care Med 39:1785–1791. https://doi.org/10.1007/s00134-013-2970-4
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO Clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Argyropoulos CP, Chen SS, Ng YH, Roumelioti ME, Shaffi K, Singh PP, Tzamaloukas AH (2017) Rediscovering beta-2 microglobulin as a biomarker across the spectrum of kidney diseases. Front Med (Lausanne) 15:73. https://doi.org/10.3389/fmed.2017.00073
Ruggiero A, Ferrara P, Attinà G, Rizzo D, Riccardi R (2017) Renal toxicity and chemotherapy in children with cancer. Br J Clin Pharmacol 83:2605–2614. https://doi.org/10.1111/bcp.13388
Satirapoj B, Kongthaworn S, Choovichian P, Supasyndh O (2016) Electrolyte disturbances and risk factors of acute kidney injury patients receiving dialysis in exertional heat stroke. BMC Nephrol 17:55. https://doi.org/10.1186/s12882-016-0268-9
McMahon KR, Rassekh SR, Schultz KR, Blydt-Hansen T, Cuvelier GDE, Mammen C, Pinsk M, Carleton BC, Tsuyuki RT, Ross CJD, Palijan A, Huynh L, Yordanova M, Crépeau-Hubert F, Wang S, Boyko D, Zappitelli M; Applying Biomarkers to Minimize Long-term Effects of Childhood/Adolescent Cancer Treatment (ABLE) Research Study Group (2020) Epidemiologic Characteristics of Acute Kidney Injury During Cisplatin Infusions in Children Treated for Cancer. JAMA Netw Open 3:e203639. https://doi.org/10.1001/jamanetworkopen.2020.3639
Burns AR, Ho KM (2018) Urinary potassium excretion and its association with acute kidney injury in the intensive care unit. J Crit Care 46:58–62. https://doi.org/10.1016/j.jcrc.2018.04.009
Hall AM, de Seigneux S (2022) Metabolic mechanisms of acute proximal tubular injury. Pflugers Arch 474:813–827. https://doi.org/10.1007/s00424-022-02701-y
Daha MR, van Kooten C (2000) Is the proximal tubular cell a proinflammatory cell? Nephrol Dial Transplant 15(Suppl 6):41–43. https://doi.org/10.1093/ndt/15.suppl_6.41
Barak V, Schwartz A, Kalickman I, Nisman B, Gurman G, Shoenfeld Y (1998) Prevalence of hypophosphatemia in sepsis and infection: the role of cytokines. Am J Med 104:40–47. https://doi.org/10.1016/s0002-9343(97)00275-1
Nakamura K, Hayashi H, Kubokawa M (2015) Proinflammatory Cytokines and Potassium Channels in the Kidney. Mediators Inflamm 2015:362768. https://doi.org/10.1155/2015/362768
Zeng S, Hossain D, Bostwick DG, Herrera GA, Zhang PL (2014) Urinary β2-microglobulin is a good indicator of proximal tubule injury: a correlative study with renal biopsies. J Biomark 2014:492838. https://doi.org/10.1155/2014/492838
Portman RJ, Kissane JM, Robson AM (1986) Use of beta 2 microglobulin to diagnose tubulo-interstitial renal lesions in children. Kidney Int 30:91–98. https://doi.org/10.1038/ki.1986.156
Barton KT, Kakajiwala A, Dietzen DJ, Goss CW, Gu H, Dharnidharka VR (2018) Using the newer Kidney Disease: Improving Global Outcomes criteria, beta-2-microglobulin levels associate with severity of acute kidney injury. Clin Kidney J 11:797–802. https://doi.org/10.1093/ckj/sfy056
Du Y, Zappitelli M, Mian A, Bennett M, Ma Q, Devarajan P, Mehta R, Goldstein SL (2011) Urinary biomarkers to detect acute kidney injury in the pediatric emergency center. Pediatr Nephrol 26:267–274. https://doi.org/10.1007/s00467-010-1673-0
Roth KS, Foreman JW, Segal S (1981) The Fanconi syndrome and mechanisms of tubular transport dysfunction. Kidney Int 20:705–716. https://doi.org/10.1038/ki.1981.200
Morgan JE, McKeever K, Tyerman KS, Henderson M, Picton S, Phillips RS (2016) Aminoaciduria in the prediction of ifosfamide-induced tubulopathy after childhood cancer: a feasibility study. Pilot Feasibility Stud 2:4. https://doi.org/10.1186/s40814-015-0040-0
Kwiatkowski DM, Menon S, Krawczeski CD, Goldstein SL, Morales DL, Phillips A, Manning PB, Eghtesady P, Wang Y, Nelson DP, Cooper DS (2015) Improved outcomes with peritoneal dialysis catheter placement after cardiopulmonary bypass in infants. J Thorac Cardiovasc Surg 149:230–236. https://doi.org/10.1016/j.jtcvs.2013.11.040
Ostermann M, Zarbock A, Goldstein S, Kashani K, Macedo E, Murugan R, Bell M, Forni L, Guzzi L, Joannidis M, Kane-Gill SL, Legrand M, Mehta R, Murray PT, Pickkers P, Plebani M, Prowle J, Ricci Z, Rimmelé T, Rosner M, Shaw AD, Kellum JA, Ronco C (2020) Recommendations on acute kidney injury biomarkers from the acute disease quality initiative consensus conference: A consensus statement. JAMA Netw Open 3:e2019209. https://doi.org/10.1001/jamanetworkopen.2020.19209
Author information
Authors and Affiliations
Contributions
Research idea and study design: WF Hui; Data acquisition: WF Hui, VPY Chan; Data analysis and manuscript drafting: WF Hui; Clinical management: WF Hui, WL Cheung, VPY Chan; KL Hon; SW Ku; Supervision: SW Ku, KL Hon; Manuscript review and approval: WL Cheung, VPY Chan; SW Ku, KL Hon.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest and did not receive any financial support from any organization for the submitted work.
Ethics approval and informed consent
The study complied with Declaration of Helsinki and was conducted in accordance with the approved protocol of the research ethics committee of the Hong Kong Children’s Hospital (HKCH-REC-2020–007). Informed consent has been obtained from the parents of the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hui, W.F., Chan, V.P.Y., Cheung, W.L. et al. The impact of tubular dysfunction and its relationship with acute kidney injury in children. Pediatr Nephrol 39, 1617–1626 (2024). https://doi.org/10.1007/s00467-023-06220-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06220-5