Abstract
Background
Cocrystallization by solvent evaporation was used to enhance the dissolution, physicochemical properties, and bioavailability of nimodipine (NMD). Here, we aimed to develop NMD cocrystals with improved solubility and dissolution. Thereafter, our objective was to check the changes in brain tissue concentrations before and after the cocrystal formation of NMD.
Methods
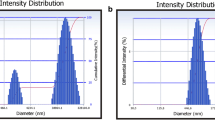
A 32-factor design was used for product optimization by determining the desirability function. Differential scanning calorimetry, powder X-ray diffraction, and scanning electron microscopy were used to confirm the formation of cocrystals.
Results
The saturation solubility study of NMD:SA cocrystals resulted in 9.52 mg/ml, which is 128-fold higher than that of pure NMD (0.074 mg/ml). In vitro dissolution and permeability studies showed an improvement in the percentage of drug release and permeability of NMD from cocrystals as compared to pristine NMD. An in vivo study of oral bioavailability in Wistar rats demonstrated higher plasma and brain tissue concentrations of NMD in the cocrystal form than in the conventional oral suspension.
Discussions
The findings of this study showed a positive correlation between nimodipine solubility, improvement in dissolution, and its effect on brain tissue concentration in Wistar rats. The improved solubility of nimodipine may lead to increased dissolution rates, which can enhance its bioavailability and therapeutic efficacy in the treatment of cerebral vasospasms.








Similar content being viewed by others
Data Availability
Data will be made available on request to authors.
References
Blagden N, de Matas M, Gavan PT, York P. Crystal engineering of active pharmaceutical ingredients to improve solubility and dissolution rates. Adv Drug Deliv Rev. 2007;59(7):617–30. Available from: https://www.sciencedirect.com/science/article/pii/S0169409X07000828.
Savjani KT, Gajjar AK, Savjani JK. Drug solubility: importance and enhancement techniques. ISRN Pharm. 2012;2012(100 mL):1–10.
Bavishi DD, Borkhataria CH. Spring and parachute: how cocrystals enhance solubility. Prog Cryst Growth Charact Mater. 2016;62(3):1–8.
Urso R, Blardi P, Giorgi G. A short introduction to pharmacokinetics. Eur Rev Med Pharmacol Sci. 2002;6(2):33–44.
Kotak U, Prajapati V, Solanki H, Jani G, Jha P. Co-crystallization technique - its rationale and recent progress. World J Pharm Pharm Sci. 2015;4(04):1484–508.
Vaghela P, Tank HM, Jalpa P. Cocrystals : a novel approach to improve the physicochemical and mechanical properties. Indo Am J Pharm Res. 2014;4(10).
Desiraju G. Crystal engineering: a brief overview. J Chem Sci. 2010;122:667–75.
Elliott WJ, Ram CVS. Calcium channel blockers. J Clin Hypertens (Greenwich). 2011;13(9):687–9.
Mahmoud SH, Ji X, Isse FA. Nimodipine pharmacokinetic variability in various patient populations. Drugs R D. 2020;20(4):307–18.
Riekes MK, Caon T, da Silva J, Sordi R, Kuminek G, Bernardi LS, et al. Enhanced hypotensive effect of NMD solid dispersions produced by supercritical CO2 drying. Powder Technol. 2015;278:204–10.
Zhao Y, Xin T, Ye T, Yang X, Pan W. Solid dispersion in the development of a NMD delayed-release tablet formulation. Asian J Pharm Sci. 2014;9(1):35–41.
Sun Y, Rui Y, Wenliang Z, Tang X. NMD semi-solid capsules containing solid dispersion for improving dissolution. Int J Pharm. 2008;359(1):144–9.
Zu Y, Li N, Zhao X, Li Y, Ge Y, Wang W, et al. In vitro dissolution enhancement of micronized l-NMD by antisolvent re-crystallization from its crystal form H. Int J Pharm. 2014;464(1):1–9.
Hänggi D, Etminan N, Macdonald RL, Steiger HJ, Mayer SA, Aldrich F, et al. NEWTON: NMD microparticles to enhance recovery while reducing toxicity after subarachnoid hemorrhage. Neurocrit Care. 2015;23(2):274–84.
Fu Q, Sun J, Zhang D, Li M, Wang Y, Ling G, et al. NMD nanocrystals for oral bioavailability improvement: preparation, characterization and pharmacokinetic studies. Colloids Surf B Biointerfaces. 2013;109:161–6.
Yu J, He HB, Tang X. Formulation and evaluation of NMD-loaded lipid microspheres. J Pharm Pharmacol. 2006;58(11):1429–35.
Xiong R, Lu W, Li J, Wang P, Xu R, Chen T. Preparation and characterization of intravenously injectable NMD nanosuspension. Int J Pharm. 2008;350(1):338–43.
Fu Q, Kou L, Gong C, Li M, Sun J, Zhang D, et al. Relationship between dissolution and bioavailability for NMD colloidal dispersions: the critical size in improving bioavailability. Int J Pharm. 2012;427(2):358–64.
Liu M, Hong C, Yao Y, Shen H, Ji G, Li G, et al. Development of a pharmaceutical cocrystal with solution crystallization technology: preparation, characterization, and evaluation of myricetin-proline cocrystals. Eur J Pharm Biopharm. 2016;107:151–9.
Alatas F, Ratih H, Soewandhi SN. Enhancement of solubility and dissolution rate of telmisartan by telmisartan-oxalic acid co-crystal formation. Int J Pharm Pharm Sci. 2015;7(3):423–6.
Hiendrawan S, Hartanti AW, Veriansyah B, Widjojokusumo E, Tjandrawinata RR. Solubility enhancement of ketoconazole via salt and cocrystal formation. Int J Pharm Pharm Sci. 2015;7(7):160–4.
Shewale S, Shete AS, Doijad RC, Kadam SS, Patil VA, Yadav AV. Formulation and solid state characterization of nicotinamide-based co-crystals of fenofibrate. Indian J Pharm Sci. 2015;77(3):328–34.
Sarkar A, Rohani S. Cocrystals of acyclovir with promising physicochemical properties. J Pharm Sci. 2015;104(1):98–105.
Shah K, Borhade SD, Londhe V. Utilization of co-crystallization for solubility enhancement of a poorly soluble antiretroviral drug - RITONAVIR. Int j Pharm Pharm Sci. 2014;(2):556–8.
Sanphui P, Devi VK, Clara D, Malviya N, Ganguly S, Desiraju GR. Cocrystals of hydrochlorothiazide: solubility and diffusion/permeability enhancements through drug–coformer interactions. Mol Pharm. 2015;12(5):1615–22.
Lee G, Goosens KA. Sampling blood from the lateral tail vein of the rat. J Vis Exp. 2015;99: e52766.
Brahmankar DM, Jaiswal SB. Biopharmaceutics and pharmacokinetics: a treatise. Vallabh Prakashan. 2005. Available from: https://books.google.co.in/books?id=PVCEMwEACAAJ.
Zhang Q, Jiang X, Wu C. Distribution of NMD in brain following intranasal administration in rats. Acta Pharmacol Sin. 2004;25(4):522–7.
Paduszyński K. Extensive evaluation of the conductor-like screening model for real solvents method in predicting liquid-liquid equilibria in ternary systems of ionic liquids with molecular compounds. J Phys Chem B. 2018;122(14):4016–28.
Sathisaran I, Dalvi SV. Crystal engineering of curcumin with salicylic acid and hydroxyquinol as coformers. Cryst Growth Des. 2017;17(7):3974–88.
Panzade P, Shendarkar G, Shaikh S, Rathi PB. Pharmaceutical cocrystal of piroxicam: design, formulation and evaluation. Adv Pharm Bull. 2017;7(3):399–408.
Lu E, Rodríguez-Hornedo N, Suryanarayanan R. A rapid thermal method for cocrystal screening. CrystEngComm. 2008;10(6):665–8.
Beck R, Nyster TO, Enstad GG, Malthe-Sørenssen D, Andreassen JP. Influence of crystal properties on powder flow behavior of an aromatic amine and l-glutamic acid. Part Sci Technol. 2010;28(2):146–60.
Rahman Z, Agarabi C, Zidan AS, Khan SR, Khan MA. Physico-mechanical and stability evaluation of carbamazepine cocrystal with nicotinamide. AAPS PharmSciTech. 2011;12(2):693–704.
Emami S, Siahi-Shadbad M, Adibkia K, Barzegar-Jalali M. Recent advances in improving oral drug bioavailability by cocrystals. BioImpacts. 2018;8(4):305–20.
Towart R, Wehinger E, Meyer H, Kazda S. The effects of NMD, its optical isomers and metabolites on isolated vascular smooth muscle. Arzneimittelforschung. 1982;32(4):338–46.
Wessell A, Kole MJ, Badjatia N, Parikh G, Albrecht JS, Schreibman DL, et al. High compliance with scheduled NMD is associated with better outcome in aneurysmal subarachnoid hemorrhage patients cotreated with heparin infusion. Front Neurol. 2017;8:268.
Herbette LG, Mason PE, Sweeney KR, Trumbore MW, Mason RP. Favorable amphiphilicity of NMD facilitates its interactions with brain membranes. Neuropharmacology. 1994;33(2):241–9.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Nilam Rathod and Vidhi Patel—research; Ravi Manek and Chetan Borkhataria—guidance and article draft. Nilesh Patel, Kalpesh Patel, and Jalpa Paun—calculations and factorial design. Dhruv Sakhiya—inferences and discussion of the results.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rathod, N., Borkhataria, C., Manek, R. et al. Study on the Correlation Between Nimodipine (BCS Class II) Solubility, Dissolution Improvement, and Brain Tissue Concentration Through Cocrystallization. J Pharm Innov 18, 2235–2248 (2023). https://doi.org/10.1007/s12247-023-09786-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12247-023-09786-7