Abstract—The aim of this work was to study the effects of thymosin-1 alpha (Tα1) on the anti-inflammatory response of RAW 264.7 macrophages cultured in the presence of lipopolysaccharide (LPS) from the walls of gram-negative bacteria. As well, we evaluated production of pro-inflammatory cytokines and the activity of the NF-κB and SAPK/JNK signaling pathways. In addition, the level of expression of a number of genes that regulate cell apoptosis, as well as the activity of receptors involved in the pro-inflammatory response, was determined. First, the addition of Tα1 normalized the level of cytokine production to varying degrees, with a particularly noticeable effect on IL-1β and IL-6. Second, the addition of Tα1 normalized the activity of the NF-κB and SAPK/JNK signaling cascades and the expression of the Tlr4 gene. Third, Tα1 significantly reduced p53 and the activity of the P53 gene, which is a marker of cell apoptosis. Fourth, it was shown that the increase in Ar-1 gene expression under the influence of LPS was significantly reduced using Tα1. Thus, it was found that the presence of Tα1 in the RAW 264.7 cell culture medium significantly reduced the level of the pro-inflammatory response of cells.
Similar content being viewed by others
INTRODUCTION
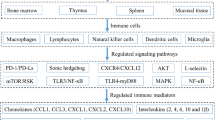
Inflammation is the response of the immune system to damaging factors, including pathogens, damaged cells, toxic compounds, or ionizing radiation [1]. In this case, the reaction of the body is aimed at removing damaging stimuli and initiating the healing process [2]. Thus, inflammation is a protective mechanism that is vital for mammals [3]. Over the past 15 years, we have studied the anti-inflammatory efficacy of thymus hormones (thymulin and thymopentine) under in vitro and in vivo conditions [4–15]. The choice of this line of research is due to the understanding of the special role of the thymus in the functioning of the immune system. It is known that the thymus undergoes age-related involution [16], which can be accelerated when exposed to damaging factors. At the same time, the accelerated involution of the thymus manifests itself as a side effect caused by the use of a number of drugs in such serious diseases as tuberculosis, and oncological diseases [17]. Thymus involution can reduce the body’s ability to rebuild the peripheral T cell repertoire and respond to new antigens. Currently, there are no available treatments for acute thymic atrophy, which leads to disruption of the immune system during acute stressful events [18]. It is known that many damaging factors, including infections, poisons, ionizing radiation, etc., lead to acute atrophy of the thymus tissue. It is important to note that according to existing concepts all physiological stress factors, including malnutrition, lead to acute thymus involution [19].
To prevent the transition of acute inflammation to chronic inflammation, inflammatory reactions must be suppressed to prevent additional tissue damage. The reduction in inflammation is a well-controlled process involving controlled production of mediators in space and time, in which chemokine gradients, cytokines, and reactive oxygen species (ROS) are “diluted” over time [20]. Circulating leukocytes gradually cease to feel these changes and are not recruited to the sites of injury. Dysregulation of this process can lead to uncontrolled chronic inflammation [21]. Inflammatory resolution processes that restore tissue homeostasis include reduction or cessation of tissue infiltration by neutrophils and apoptosis of waste neutrophils, counterregulation of chemokines and cytokines, transformation of macrophages from classical to alternatively activated, and initiation of healing [22, 23].
Previously, we proved the anti-inflammatory effect of the thymus hormones thymulin and thymopentine not only in the model of sepsis in mice [4–6], but also in a condition simulating multiple sclerosis [7, 8]. The published data point to the likely anti-inflammatory efficacy of another thymus hormone, Thymosin α-1 (Tα1) [26, 27] and determined that Tα1 is a potent modulator of immunity and inflammation. Taken together, the results of these studies confirm the intrathymic role of the hormone leptin in maintaining healthy thymic epithelium and stimulation of thymopoiesis, which manifests itself when endotoxemia disrupts thymic homeostasis [1]. In addition, a certain relationship has been established between the longevity of centenarians, the state of the immunosenescence system, and the level of Tα1 [19, 28, 29]. Tα1, a 28-amino acid protein with immunomodulatory functions, has a beneficial effect in infectious and oncological diseases, immunodeficiency states, and also has a neuroprotective effect [30].
Taking these data into account, the aim of this work was to study the effects of Tα1 on the pro-inflammatory activation of alveolar macrophages RAW264.7 cultivated in the presence of lipopolysaccharide (LPS) from the walls of gram-negative bacteria. The production of pro-inflammatory cytokines was evaluated, and the state of the NF-κB and SAPK/JNK signaling pathways was also studied. In addition, the level of expression of a number of genes that regulate the levels of cell apoptosis, as well as the activity of the TLR4 receptor, which is involved in the pro-inflammatory response, was determined.
EXPERIMENTAL
Cultivation of RAW 264.7 cells. Cultivation of cells of the RAW264.7 macrophage line was performed in the presence of an inducer of inflammation and Tα1. RAW 264.7 cells were grown in culture flasks in a medium consisting of a mixture of RPMI : DMEM (PanEco, Russia) in a 1 : 1 ratio supplemented with 10% fetal calf serum (FBS) and a mixture of antibiotics (penicillin 100 µg/mL, streptomycin 100 µg/mL, gentamicin 50 µg/mL), at 37°C and 5% CO2. Cell reseeding (passage) was performed after reaching a monolayer density of ~80%. Cells were used in the experiments after four to eight passages. After each passage, the viability of RAW 264.7 was assessed visually using an inverted LEICA DMIL HC microscope (Leica, Germany), as well as by counting living cells in a Goryaev chamber when the RAW 264.7 suspension was stained with a 0.01% trypan blue solution (AppliChem, Germany) in physiological saline (NaCl 0.9%). The number of surviving macrophage cells was 93–97%. Pro-inflammatory responses were induced by LPS isolated from the walls of the Escherichia coli strain 0128: B12 (Sigma, United States) at a concentration of 1 μg/mL. Exogenous Tα1 (Sigma) was added at a concentration of 10 ng/mL simultaneously with the induction of pro-inflammatory responses. To determine the production of cytokines, cells were removed from the surface of the culture flask using scrapers (Corning, United States), washed from the old medium, diluted in fresh medium, and seeded at a density of 106 cells in 1 mL in 24-well plates. After 24 h, the test substances were added to each well at a given concentration. At the end of the 72-h incubation, the cells were lysed three times by freeze-thaw, while the lysates were used immediately or stored at –20°C. To determine the production of signal and stress proteins, the cells were seeded into culture flasks with a density of 100 × 106 cells per vial. After cell attachment (24 h), test substances were added according to the above scheme and incubated for 6 h. Next, the cells were removed from the surface of the flask, washed from the old medium, and diluted in 1 mL of saline for further protein isolation. Within each independent experiment, the characteristics of the samples were measured in parallel in six to nine repetitions and the average value was determined. Values averaged over four experiments were used to determine the statistical significance of differences between groups (n = 4). Cells that had not been treated with LPS were used as controls.
Viability test. RAW 264.7 cells were cultured in 96‑well plates (TPP, Switzerland), 100 µL (2 × 104 cells) per well in RPMI 1640 medium (PanEco) containing 10% FTS, 2.04 mM L-glutamine (PanEco), 100 µg/mL streptomycin at 37°С in an atmosphere of 5% CO2. After culturing for 24 h, either LPS (1 µg/mL), or Tα1 (10 ng/mL), or LPS + Tα1 at the indicated concentrations was added to a monolayer of RAW 264.7 cells, cultured for another 24 h, washed three times with PBS, and stained for 10 min with a 0.05% violet crystal (Sigma). The wells were thoroughly washed with running distilled water, and 100 µl of 1% sodium dodecyl sulfate was added to each well. Ten minutes later, the optical density was measured at 546 nm on a Titertek Multiscan MCC/340 plate spectrophotometer (Flow Laboratories, Finland).
Determination of the level of oxidative stress in cells. The level of oxidative stress in cells was measured using the diacetyl derivative of 5,6-carboxy-2',7'-dichlorodihydrofluorescein (carboxy-H2DCFDA) (Invitrogen, United States). Carboxy-H2DCFDA is a chemically reduced analogue of fluorescein used as a general indicator of oxidative stress in cells. This nonfluorescent molecule is readily converted to the green fluorescent form (carboxy-DCF) as intracellular oxidation removes acetate groups by intracellular esterases. It should be noted that DCFH (and carboxy-H2DCFDA) do not react with superoxide, hydrogen peroxide, or nitric oxide. The DCFH/carboxy-H2DCFDA ratio largely reflects the peroxidase-catalyzed oxidation. RAW 264.7 cells were preliminarily cultured for 24 h in a 96-well plate (2.5 × 104 cells per well) in 100 µL of DMEM medium, washed with PBS, and treated with a freshly prepared solution of carboxy-H2DCFDA (Invitrogen) in sterile DMSO at a final concentration of 2.5 µM in a medium with 2% FTS. Cells were incubated with carboxy-H2DCFDA in the dark for 1 h. Simultaneously with the addition of carboxy-H2DCFDA, LPS (1 μg/mL), Tα1 (10 ng/mL) were added. The fluorescence signal from untreated RAW 264.7 cells was used as a control. The background signal of the culture medium DMEM was subtracted from the corresponding signals of the experimental samples. Fluorescence was measured using an Infinite 200 fluorescent plate reader (Tecan, Austria) at an excitation wavelength of 480 nm and an absorption wavelength of 530 nm (Ex/Em = 485/535 nm). Three independent experiments were performed (three repetitions for each experimental group (n = 9).
Determination of cytokine production. Mouse TNF, IL-10 IL-1β, and IL-6 were determined using an ELISA kit (PeproTech, United States). Binding was visualized using 100 µL of ABTS green dye (Sigma) dissolved in 0.05 M citrate buffer (pH 5.0) supplemented with 0.01% hydrogen peroxide, and the optical density was measured at 405 nm using a microplate spectrophotometer (Multiscan EX; Thermo Electron Corp., United States).
Denaturing gel electrophoresis and immunoblotting. To prepare protein samples, a suspension of RAW 264.7 cells, previously washed from the cultivation medium with 0.9% NaCl, was frozen–thawed three times. After this, protease and phosphatase inhibitors were added. (Protease and phosphatase inhibitor cocktail 100 xl; Thermo Scientific). Solubilizing buffer for electrophoresis, β-mercaptoethanol (2–5%) was added to the samples prepared in this way and boiled for 5 min. The protein concentration was measured using a NanoDrop2000c (NanoDrop, United States); 10 µL of the sample was added to each well of a 10% denaturing polyacrylamide gel (Ds-Na-PAGE). The presence of proteins in the samples was determined using Western blot analysis using sets of antibodies: rabbit antibodies to ph-NF-κB (Ser536), p53, ph-SAPK/JNK, NRF-2, TLR4, α-β-tubulin (Cell Signaling, United States). Proteins were detected using the ECL system (GE Healthcare, Sweden). The photographs of the bands were taken with a TFX 35 WL transilluminator (Vilber Lourmat, France). The quantitative content of proteins was determined after densitometry using the Qapa program (Ver. 3.7). Three independent experiments were carried out (cells from different passages were used) for each protein. The obtained digital data were normalized according to the values in the corresponding control (α-β-tubulin bands) and expressed in relative units.
Assessment of changes in gene expression. Gene expression was analyzed in RAW 264.7 cells by real-time PCR (RT-PCR). Tα1 (10 ng/mL) or LPS (1 μg/mL) were added separately or together to the cell culture medium, incubated for 6 h, and the expression of genes associated with apoptosis was determined (P53) encoding transcription factors (NF-κB, Ap-1, and NRF-2), TLR4 receptor, cytokines TNF, IL-6, and iNos.
The procedure for isolation of total RNA, cDNA synthesis, and real-time PCR we described in detail in [31]. RNA was isolated from RAW 264.7 cells using the RNA extract reagent according to the manufacturer’s instructions (Evrogen, Russia). Total RNA was treated with DNase I (New England Biolabs, United States) to remove possible genomic DNA impurities. The RNA concentration was determined spectrophotometrically (NanoDrop1000c, United States) by absorbance at 260 nm. RNA integrity was assessed by electrophoresis in 2% agarose gel in the presence of ethidium bromide (1 μg/mL) by the presence of rRNA bands (18S and 28S). The resulting RNA (2 µg per reaction) was used in the reverse transcription reaction using the MMLV RT kit (Evrogen). The synthesized cDNA was used in real-time PCR with gene-specific oligonucleotides (Table 1) and 5× qPCRmix-HS kit (Evrogen) in a DTprime amplifier (DNA-technology, Russia), real-time PCR mode: (1) hot start, 95°С, 3 min; (2) denaturation, 95°С, 15 s; and (3) primer annealing and chain synthesis, 60°С, 20 s + fluorescence registration. Steps 2 and 3 were repeated 40 times. Changes in gene expression levels are presented in relative units from the values in the control for intact cells [31].
The level of gene expression was normalized according to the level of the cytoskeletal β-actin gene (gene Actb household). The ΔCt value was calculated using the formula ΔCt = Ct(tested gene) – Ct (Actb); ΔΔCt was calculated using the formula ΔCt (control) × ΔCt (experiment). Differences in gene expression were calculated using the 2^–ΔΔCt method.
Statistical analysis was carried out using Statistica 6.0 software (StatSoft, United States). Statistical significance of differences was determined using one-way analysis of variance (ANOVA) with Tukey’s post hoc test. Differences were considered significant for p < 0.05.
RESULTS
The Effect of Thymosin-1α on the Expression of Genes Regulating the Response of RAW 264.7 Cells to Lipopolysaccharide
Real-time PCR was used to evaluate the expression of genes known as genes that regulate the response of cells to the damaging effects of endotoxin. These genes include, first of all, the genes of cytokines, the concentration of which (TNF and IL-6) usually sharply increases when exposed to endotoxin. As for the genes of these cytokines, we also noted a significant stimulation of expression, especially TNF (almost 5 times), and IL-6 by 2.5 times (Table 1). At the same time, the addition of Tα1 significantly reduced the expression TNF induced by LPS. It is important to note that the introduction of LPS into the RAW 264.7 cell culture medium caused a significant increase in the expression of all the studied genes, except for the Nrf-2 gene. No significant upregulation of gene expression was noted for Nrf-2 under the influence of LPS, although Tα1 against the background of LPS significantly stimulated the expression of this gene, which indicates an increase in the antioxidant protection of cells in the presence of thymus peptide.
It should be noted that the addition of Tα1 statistically significantly normalized the expression of all the studied genes. The only exception was inos gene expression, encoding inducible NO-synthase, the synthesis of which in the presence of LPS increased by 8 times, and with the addition of Tα1, by 13 times.
For the Tlr4 gene, in the presence of LPS, its expression increased by almost 2.5 times, while the addition of Tα1 led to a significant decrease in the expression of this gene, which indicates the normalization caused by the presence of Tα1 in the culture medium of RAW 264.7 cells. The same changes were found in the expression of the Nf-κb gene, which increased by almost 4 times in the presence of LPS, while the addition of Tα1 significantly reduced the expression of this gene (Table 2).
However, determining Ap-1 gene expression showed that the presence of LPS in the RAW 264.7 cell culture medium activated the expression of this gene by almost 6.5 times, while the addition of Tα1 significantly reduced its level. P53 gene expression, which regulates the level of cell apoptosis, sharply increased in the presence of LPS (8.5 times), while the addition of Tα1 reduces this effect (Table 2).
Production of Cytokines and Reactive Oxygen Species in RAW 264.7 Alveolar Macrophages Cultivated in the Presence of Lipopolysaccharide and Thymosin-1α
The production of several pro-inflammatory cytokines (TNF, IL-6, and IL-1β) and the anti-inflammatory cytokine IL-10 was measured by enzyme immunoassay (ELISA). It is important that the addition of LPS to the RAW 264.7 cell culture medium stimulated the production of all studied cytokines, while the addition of Tα1 normalized the production of cytokines to varying degrees. A particularly noticeable effect was observed in the case of IL-1β and IL-6 (Fig. 1a). However, the addition of Tα1 did not reduce TNF production in LPS-activated macrophages.
The effect of thymosin-1alpha on the production of cytokines (a), ROS production estimated by probe fluorescence (b), and the number of living cells RAW 264.7 (c). *Statistically significant differences from the LPS group, p < 0.05. **Statistically significant differences from the LPS group, p < 0.01. n = 3–4.
It is known that under the influence of LPS, ROS production can increase in the cell. In fact, using a fluorescent carboxy-H2DCFDA probe, we have shown that the addition of LPS leads to a several-fold increase in the amount of ROS produced in RAW 264.7 cells; the addition of Tα1 completely removes this effect (Fig. 1b). At the same time, the addition of only Tα1 to cells did not affect the level of ROS.
Interestingly, quantification of viable RAW 264.7 macrophages showed that both LPS and Tα1 stimulate cell viability and these effects were additive (Fig. 1c). This important observation indicates that the concentration of Tα1, equal to 10 ng/mL and significantly higher than the concentration in control cells, is not toxic.
Production of Proteins Regulating the Activity of Signaling Cascades and TLR4, Apoptosis of RAW 264.7 Cells
It is known that the NF-κB signaling cascade is the main regulator of cell activity in the presence of damaging agents. Determination of the level of the p65 NF-κB protein showed that the addition of LPS significantly increases the amount of this protein, while the addition of Tα1 cells to the culture medium completely removes the effect of LPS. Thus, we have proved that Tα1 protects cells from the action of endotoxin. Examination of the activity of another signal transduction cascade, SAPK/JNK, showed that under the influence of LPS, the accumulation of phosphorylated p46 and p54 forms in cells increases, and the addition of Tα1 eliminates the functional activation of these proteins in the cell induced by LPS (Fig. 2). This indicates the protective potential of Tα1, which removed the damaging effect of LPS; this causes the activation of the SAPK/JNK cascade.
Western blot analysis of proteins (TLR4, NF-κB and SAPK/JNK, NRF-2, and p53) in RAW 264.7 cells cultured under different conditions. The results of a typical experiment are presented. Under the immunoblots, the content of proteins (in relative units) is indicated, calculated from the averaged results of densitometric determination in three independent experiments, in % of the control. Statistically significant differences from values in cells incubated with the addition of LPS, **R < 0.01 *p < 0.05. The content of phNF-κB (Ser276) was determined using antibodies to the p65 subunit.
Toll-like receptors (TLRs) are involved in signaling that activates the NF-κB signal transduction cascade. The most studied receptor of this class is the TLR4transmembrane receptor. We have shown that the cultivation of RAW 264.7 cells in the presence of LPS leads to a statistically significant increase in the amount of TLR4, while the addition of Tα1 completely removes the effect of LPS (Fig. 2).
Figure 2 also shows the results of determination of the amount of the NRF-2 protein, which regulates the antioxidant response of cells. In the presence of LPS, a decrease in the level of NRF-2 protein was observed, while the addition of Tα1 to the RAW 264.7 cell culture medium increased the level of NRF-2 protein to values exceeding the control level.
Finally, changes in the content of the p53 protein, which is involved in the regulation of the level of apoptosis in cells, were analyzed by Western blotting. It was found that the addition of LPS leads to an increase in p53 content, which indicates the induction of apoptosis in RAW 264.7 cells in the presence of endotoxin. If Tα1 was added to the cells, a decrease in the level of the p53 protein was observed, which indicates the possibility of a change in the level of apoptosis (Fig. 2).
DISCUSSION
The effectiveness of Tα1 as an anti-inflammatory agent was studied on RAW 264.7 alveolar macrophages that were exposed to endotoxin (LPS), which is most often used to model inflammation. We analyzed such cell functions as production of pro- and anti-inflammatory cytokines (TNF-α, IL-6, IL-1β, and IL-10), ROS formation, activity of NF-κB and SAPK/JNK signaling cascades, production of NRF-2, TLR4, and p53, as well as the activity of a number of genes that regulate-synthesis of these key agents.
Previously, using RAW 264.7 macrophages, we showed that other thymus peptides (thymulin and thymopentin) also exhibit an anti-inflammatory effect in LPS-treated cells [6]. Both peptides reduced the secretion of pro-inflammatory cytokines in RAW 264.7 macrophages cultured with LPS, and these effects were blocked by inhibitors of the NF-κB cascades and SAPK/JNK stress-activated protein kinase, as well as, to a lesser extent, by an inhibitor of TLR4.
In RAW 264.7 macrophages stimulated with bacterial LPS, the peptides themselves did not affect the secretion of cytokines, but significantly enhanced the effects of each of the inhibitors. Thymopentin increased the activation of the NF-κB and SAPK/JNK cascades in unstimulated macrophages, while thymulin significantly reduced the activation of the SAPK/JNK cascade, but not NF-κB, in LPS-stimulated macrophages. Thymulin and thymopentin increased the production of the HSP72 heat shock protein in both stimulated and unstimulated LPS cells [6].
The possibility of using thymus hormones (thymulin and thymopentin) as anti-inflammatory agents was confirmed by us earlier [4–6]. In the present work, we analyzed the anti-inflammatory efficacy of Tα1. It could be assumed that Tα1 is able to compensate for the state of chronic inflammation caused by endotoxin. In reality, to understand the mechanism of action of thymus hormones, it is useful to take into account the role of age-related thymus involution and the lack of secretion of thymus hormones for aging processes and, especially, “inflammatory aging.”
Two centuries ago, the average life expectancy of a person, even in the most developed countries, did not exceed 40–45 years, although even then there were centenarians. However, the improvement of living conditions and advances in medicine have led to an increase in life expectancy, and, consequently, to the aging of a significant part of the population [32].
The human immune system is forced to cope with the evolutionarily unpredictable exposure to various antigens, which underlies the deep age-related changes referred to as immunosenescence, or immunoaging. The main changes that occur during immunoaging are due to the accumulation of cellular and molecular defects and involutional events (for example, thymus involution) that occur simultaneously with hyperstimulation of both innate and adaptive immunity (accumulation of proliferating clones of memory cells and effector T cells and reduction of the T-cell repertoire) receptors, and progressive activation of macrophages), which leads to indolent chronic inflammation [19].
Correlations between chronic inflammation and aging are explained within the “network theory of aging,” which considers a global decline in the ability to cope with various stressors and a concomitant progressive increase in pro-inflammatory status as the main characteristics of the aging process [3]. These characteristics, defined as “inflammatory aging,” result from antigenic load and stress, and according to evolutionary studies, the immune response and the stress response are equivalent. One can refer to the special role of macrophages as an active agent not only in the inflammatory response and immunity, but also in the response to stress [33]. At the same time, it is argued that the persistence of inflammatory stimuli over time can be considered as a biological background that favors susceptibility to age-related diseases [33]. Finally, the deficiency of resistant gene variants or the presence of weak gene variants is likely to be required for the development of overt organ-specific age-related diseases with inflammatory pathogenesis, such as atherosclerosis, Alzheimer’s disease, osteoporosis, and diabetes mellitus. Several paradoxes of healthy centenarians (increased plasma levels of inflammatory cytokines, acute phase proteins, and blood coagulation factors) have been explained in agreement with this phenomenon. However, according to the antagonistic pleiotropic theory of aging, the positive effects of inflammation, aimed at neutralizing harmful agents in early and adult life, become detrimental late in life, a period largely unforeseen by evolution [33].
Moreover, the study of the molecular mechanisms associated with thymus aging showed the need to take biological variables into account, such as gender and nutritional habits, when studying the role of genes involved in molecular processes responsible for thymus involution [34]. The use of model organisms makes it easier to test various hypotheses about the role of genetics in immune responses. Using several lines derived from the natural Drosophila melanogaster population with chromosome substitutions [35], found significant genetic variability in the immune response of flies of different strains to E. coli showing improvement, no change, or decrease with age. Overall, these data suggest that different loci contribute to variations in immune responses at each age, consistent with the aging accumulation model. Previously, it was found that in mature macrophages Tα1 internalizes and destroys pathogens by stimulating phagocytosis mediated by the complement receptor [36]. These observations support the idea that Tα1 is an early and potent activator of innate immunity and also support the concept of its pleiotropy.
An important role in aging belongs not only to cytokines, but also to oxidative stress, with the NRF-2 transcription factor being one of the main antioxidant systems [30, 37, 38]. In our work, it was shown that the addition of LPS to cells leads to a significant decrease in the content of the NRF-2 protein, while the addition of Tα1 to cultured macrophages completely removes this effect. Moreover, Tα1 stimulates Nrf-2 gene expression.
The AP-1 family of dimeric transcription complexes is involved in virtually all cellular and physiological functions. Until recently, it remained unclear how AP-1 controls gene transcription. However, the emergence of new technologies that allow the study of transcription factors on a genome-wide scale has changed the view on the mechanistic action of AP-1. There is reason to believe that AP-1 can act as a local transcription switch that operates near transcription start sites [39]. All indications are that AP-1 mainly acts as a remote command, determining the dynamics of chromatin architecture [40]. In our work, it was proved that an increase in Ar-1 gene expression under the influence of LPS was significantly reduced when using Tα1.
When selecting an appropriate dose of Tα1 to be added to cells, we relied on data according to which the concentration of Tα1 in human blood is 0.1–1 ng/mL [41]. We tried two therapeutic doses of Tα1 in situ: 10 and 50 ng/mL. Analysis of preliminary data showed that the effect of Tα1 is almost independent of the dose, so a dose of 10 ng/mL was chosen to exclude a possible toxic effect of Tα1.
It is known that stress agents increase the activity of NF-κB and SAPK/JNK signaling cascades. In fact, we have shown that the addition of LPS to RAW 264.7 cells leads to an increase in the amount of regulatory proteins; however, this activation was abolished in the presence of Tα1.
Thus, the study of the effects of Tα1 on stressed macrophages RAW 264.7 in the presence of LPS showed that Tα1 protects cells from the effects of endotoxin, in almost all cases normalizing the levels of the studied proteins and gene expression. This property of the Tα1 thymus peptide makes it a possible candidate for the role of an immunotherapeutic agent that can be used to reduce pathological signs associated not only with the development of viral and oncological diseases, but also with aging.
REFERENCES
Gruver A.G., Ventevogel M.S., Sempowski G.D. 2009. Leptin receptor is expressed in thymus medulla and leptin protects against thymic remodeling during endotoxemia induced thymus involution. J. Endocrinol. 203, 75–85.
Haynes B.F., Markert M.L., Sempowski G.D., Patel D.D., Hale L.P. 2000. The role of the thymus in immune reconstitution in aging, bone marrow transplantation, and HIV-1 infection. Annu. Rev. Immunol. 18, 529–560.
Franceschi C., Bonafè M., Valensin S., Olivieri F., De Luca M., Ottaviani E., De Benedictis G. 2000. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann. N.Y. Acad. Sci. 908, 44–54.
Lunin S.M., Khrenov M.O., Novoselova T.V., Parfenyuk S.B., Novoselova E.G. 2008. Thymulin, a thymic peptide, prevents the overproduction of pro-inflammatory cytokines and heat shock protein hsp70 in inflammation-bearing mice. Immunol. Invest. 37, 858–870.
Lunin S.M., Novoselova T.V., Khrenov M.O., Glushkova O.V., Parfenyuk S.B., Smolikhina T.I., Fesenko E.E., Novoselova E.G. 2009. Immunomodulatory effects of thymopentin under acute and chronic inflammations in mice. Biopysics (Moscow). 54. 179–181.
Lunin S.M., Glushkova O.V., Khrenov M.O., Parfenyuk S.B., Novoselova T.V., Fesenko E.E., Novoselova E.G. 2011. Thymus peptides regulate activity of RAW 264.7 macrophage cells: Inhibitory analysis and a role of signal cascades. Expert Opin. Ther. Targets. 15, 1337–1346.
Lunin S.M., Glushkova O.V., Khrenov M.O., Novoselova T.V., Parfenyuk S.B., Fesenko E.E., Novose-lova E.G. 2013. Thymic peptides restrain the inflammatory response in mice with experimental autoimmune encephalomyelitis. Immunobiology. 218, 402–407.
Lunin S.M., Khrenov M.O., Novoselova T.V., Parfenyuk S.B., Glushkova O.V., Fesenko E.E., Novoselova E.G. 2015. Modulation of inflammatory response in mice with severe autoimmune disease by thymic peptide thymulin and inhibitor of NF-kappaB signaling. Int. Immunopharmacol. 25, 260–266.
Lunin S.M., Khrenov M.O., Glushkova O.V., Vinogradova E.V., Yashin V.A., Fesenko E.E., Novoselova E.G. 2017. Extrathymic production of thymulin induced by oxidative stress, heat shock, apoptosis, or necrosis. Int. J. Immunopathol. Pharmacol. 30, 58–69.
Lunin S.M., Khrenov M.O., Glushkova O.V., Parfenyuk S.B., Novoselova T.V., Novoselova E.G. 2019. Immune response in the relapsing-remitting experimental autoimmune encephalomyelitis in mice: The role of the NF-κB signaling pathway. Cell. Immunol. 336, 20–27.
Lunin S.M., Novoselova E.G., Glushkova O.V., Parfenyuk S.B., Novoselova T.V., Khrenov M.O. 2022. Cell senescence and central regulators of immune response. Int. J. Mol. Sci. 23, 4109.
Lunin S.M., Novoselova E.G. 2010. Thymus hormones as prospective anti-inflammatory agents. Expert Opin. Ther. Targets. 14, 775–786.
Novoselova E.G., Khrenov M.O., Glushkova O.V., Lunin S.M., Parfenyuk S.B., Novoselova T.V., Fesenko E.E. 2014. Anti-inflammatory effects of IKK inhibitor XII, thymulin, and fat-soluble antioxidants in LPS-treated mice. Mediators Inflamm. 2014, 724838.
Novoselova E.G., Lunin S.M., Glushkova O.V., Khrenov M.O., Parfenyuk S.B., Zakharova N.M., Fesenko E.E. 2018. Thymulin, free or bound to PBCA nanoparticles, protects mice against chronic septic inflammation. PLoS One. 13, e0197601.
Lunin S.M., Khrenov M.O., Glushkova O.V., Parfenyuk S.B., Novoselova T.V., Novoselova E.G. 2020. Precursors of thymic peptides as stress sensors. Expert Opin. Biol. Ther. 20, 1461–1475.
Aspinall R., Andrew D. 2000. Thymic involution in aging. J. Clin. Immunol. 20, 250–256.
Gruver A.L., Sempowski G.D. 2008. Cytokines, leptin, and stress-induced thymic atrophy. J. Leukoc. Biol. 84, 915–923.
Medzhitov R. 2010. Inflammation 2010: New adventures of an old flame. Cell. 140, 771–776.
Ostan R., Bucci L., Capri M., Salvioli S., Scurti M., Pini E., Monti D., Franceschi C. 2008. Immunosenescence and immunogenetics of human longevity. Neuroimmunomodulation. 15, 224–240.
Chen L., Deng H., Cui H., Fang J., Zuo Z., Deng J., Li Y., Wang X., Zhao L. 2018. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 9, 7204–7218.
Reville K., Crean J.K., Vivers S., Dransfield I., Godson C. 2006. Lipoxin A4 redistributes myosin IIA, Cdc42 in macrophages: Implications for phagocytosis of apoptotic leukocytes. J. Immunol. 176, 1878–1888.
Headland S.E., Norling L.V. 2015. The resolution of inflammation: Principles and challenges. Semin. Immunol. 27, 149–160.
Serhan C.N., Savill J. 2005. Resolution of inflammation: The beginning programs the end. Nat. Immunol. 6, 1191–1197.
Novoselova E.G., Lunin S.M., Khrenov M.O., Novoselova T.V., Fesenko E.E. 2009. Involvement of NF-kappaB transcription factor in the antiinflammatory activity of thymic peptides. Dokl. Biol. Sci. 428. 484–486.
Lunin S.M., Khrenov M.O., Glushkova O.V., Parfenyuk S.B., Novoselova T.V., Novoselova E.G. 2019. Protective effect of PBCA nanoparticles loaded with thymulin against the relapsing-remitting form of experimental autoimmune encephalomyelitis in mice. Int. J. Mol. Sci. 20, E5374.
Romani L., Bistoni F., Montagnoli C., Gaziano R., Bozza S., Bonifazi P., Zelante T., Moretti S., Rasi G., Garaci E., Puccetti P. 2007. Thymosin alpha1: An endogenous regulator of inflammation, immunity, and tolerance. Ann. N.Y. Acad. Sci. 1112, 326–338.
Liu F., Wang H.-M., Wang T., Zhang Y.-M., Zhu X. 2016. The efficacy of thymosin α1 as immunomodulatory treatment for sepsis: A systematic review of randomized controlled trials. BMC Infect. Dis. 16, 488.
Pica F., Chimenti M.S., Gaziano R., Buè C., Casalinuovo I.A., Triggianese P., Conigliaro P., Di Carlo D., Cordero V., Adorno G., Volpi A., Perricone R., Garaci E. 2016. Serum thymosin α1 levels in patients with chronic inflammatory autoimmune diseases. Clin. Exp. Immunol. 186, 39–45.
Sansoni P., Vescovini R., Fagnoni F., Biasini C., Zanni F., Zanlari L., Telera A., Lucchini G., Passeri G., Monti D., Franceschi C., Passeri M. 2008. The immune system in extreme longevity. Exp. Gerontol. 43, 61–65.
Shi Q.-X., Chen B., Nie C., Zhao Z.-P., Zhang J.-H., Si S.-Y., Cui S.-J., Gu J.-W. 2020. Improvement in cognitive dysfunction following blast induced traumatic brain injury by thymosin α1 in rats: Involvement of inhibition of Tau phosphorylation at the Thr205 epitope. Brain Res. 1747, 147038.
Sharapov M.G., Novoselov V.I., Penkov N.V., Fesenko E.E., Vedunova M.V., Bruskov V.I., Gudkov S.V. 2018. Protective and adaptogenic role of peroxiredoxin 2 (Prx2) in neutralization of oxidative stress induced by ionizing radiation. Free Radical Biol. Med. 134, 76–86.
World Health Organization. 2002. The European Health Report 2002. European Ser. 97. Geneva, Switzerland.
Fujiwara N., Kobayashi K. 2005. Macrophages in inflammation. Curr. Drug Targets Inflam. Allergy. 4, 281–286.
Lustig A., Weeraratna A.T., Wood 3rd W.W., Teichberg D., Bertak D., Carter A., Poosala S., Firman J., Becker K.G., Zonderman A.B., Longo D.L., Taub D.D. 2007. Transcriptome analysis of age-, gender- and diet-associated changes in murine thymus. Cell Immunol. 245, 42–61.
Lesser K.J., Paiusi I.C., Leips J. 2006. Naturally occurring genetic variation in the age-specific immune response of Drosophila melanogaster. Aging Cell. 5, 293–295.
Serafino A., Pica F., Andreola F., Gaziano R., Moroni N., Moroni G., Zonfrillo M., Pierimarchi P., Sinibaldi-Vallebona P., Garaci E. 2014. Thymosin α1 activates complement receptor-mediated phagocytosis in human monocyte-derived macrophages. J. Innate Immun. 6, 72–88.
Cichon A.C., Brown D.R. 2014. Nrf-2 regulation of prion protein expression is independent of oxidative stress. Mol. Cell. Neurosci. 63, 31–37.
Yanaka A., Zhang S., Tauchi M., Suzuki H., Shibahara T., Matsui H., Nakahara A., Tanaka N., Yamamoto M. 2005. Role of the Nrf-2 gene in protection and repair of gastric mucosa against oxidative stress. Inflammopharmacology. 13, 83–90.
Seo J., Koçak D.D., Bartelt L.C., Williams C.A., Barrera A., Gersbach C.A., Reddy T.E. 2021. AP-1 subunits converge promiscuously at enhancers to potentiate transcription. Genome Res. 31, 538–550.
Manna P.R., Eubank D.W., Stocco D.M. 2019. The AP-1 transcriptional complex: Local switch or remote command. Biochim. Biophys. Acta, Rev. Cancer. 1872, 11–23.
Weller F.E., Shah U., Cummings G.D., Chretien P.B., Mutchnick M.G. 1992. Serum levels of immunoreactive thymosin alpha 1 and thymosin beta 4 in large cohorts of healthy adults. Thymus. 19, 45–52.
Funding
This work was supported by a grant from the Russian Science Foundation (project no. 23-24-00041).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
COMPLIANCE WITH ETHICAL STANDARDS
This work was carried out without involving human participants and animals as objects of study.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note.
Pleiades Publishing remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Novoselova, E.G., Glushkova, O.V., Khrenov, M.O. et al. The Thymic Hormone Thymosin-1α Reduces the Pro-Inflammatory Response of Raw 264.7 Cells Induced by Endotoxin. Mol Biol 57, 1004–1013 (2023). https://doi.org/10.1134/S0026893323060110
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0026893323060110