Abstract
Background
Observational studies have shown a causal association between dyslipidemia and osteoporosis, but the genetic causation and complete mechanism of which are uncertain. The disadvantage of previous observational studies is that they are susceptible to confounding factors and bias, that makes it difficult to infer a causal link between those two diseases. Abnormal epigenetic modifications, represented by DNA methylation, are important causes of many diseases. However, there are no studies showing a bridging role for methylation modifications in blood lipid metabolism and osteoporosis.
Methods
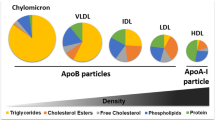
SNPs for lipid profile (Blood VLDL cholesterol (VLDL-C), blood LDL cholesterol (LDL-C), blood HDL cholesterol (HDL-C), blood triglycerides (TG), diagnosed pure hypercholesterolaemia, blood apolipoprotein B (Apo B), blood apolipoprotein A1(Apo A1)), and bone mineral density (BMD) in different body parts (Heel BMD, lumbar BMD, whole-body BMD, femoral neck BMD) were obtained from large meta-analyses of genome-wide association studies as instrumental variables for two-sample Mendelian randomization. Assessment of the genetic effects of lipid profile-associated methylation sites and bone mineral density was carried out using the summary-data-based Mendelian randomization (SMR) method.
Results
Two-sample Mendelian randomization showed that there was a negative causal association between hypercholesterolaemia and heel BMD (p = 0.0103, OR = 0.4590), and total body BMD (p = 0.0002, OR = 0.2826). LDL-C had a negative causal association with heel BMD (p = 8.68E-05, OR = 0.9586). VLDL-C had a negative causal association with heel BMD (p = 0.035, OR = 0.9484), lumbar BMD (p = 0.0316, OR = 0.9356), and total body BMD (p = 0.0035, OR = 0.9484). HDL-C had a negative causal association with heel BMD (p = 1.25E-05, OR = 0.9548), lumbar BMD (p = 0.0129, OR = 0.9358), and total body BMD (p = 0.0399, OR = 0.9644). Apo B had a negative causal association with heel BMD (p = 0.0001, OR = 0.9647). Apo A1 had a negative causal association with heel BMD (p = 0.0132, OR = 0.9746) and lumbar BMD (p = 0.0058, OR = 0.9261). The p-values of all positive results corrected by the FDR method remained significant and sensitivity analysis showed that there was no horizontal pleiotropy in the results despite the heterogeneity in some results. SMR identified 3 methylation sites associated with lipid profiles in the presence of genetic effects on BMD: cg15707428(GREB1), cg16000331(SREBF2), cg14364472(NOTCH1).
Conclusion
Our study provides insights into the potential causal links and co-pathogenesis between dyslipidemia and osteoporosis. The genetic effects of dyslipidaemia on osteoporosis may be related to certain aberrant methylation genetic modifications.



Similar content being viewed by others
Data Availability
GWAS summary data are from IEU OpenGWAS project (mrcieu.ac.uk). Data for all individuals have been uploaded to Tables 1–10 of Supplementary material.
Abbreviations
- GWAS:
-
Genome-wide association study
- BMD:
-
Bone mineral density
- MR:
-
Mendelian randomization
- Total.Body.BMD:
-
Whole-body bone mineral density
- Heel.BMD:
-
Heel bone mineral density
- Lumbar.BMD:
-
Lumbar bone mineral density
- SMR:
-
Summary-data-based mendelian randomization
- LDL-C:
-
Blood low-density lipoprotein cholesterol
- VLDL-C:
-
Blood very low-density lipoprotein cholesterol
- HDL-C:
-
Blood high-density lipoprotein cholesterol
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- SNPs:
-
Single nucleotide polymorphism
- IVW:
-
Inverse-variance weighted
- GLGC:
-
Global Lipids Genetics Consortium
- GEFOs:
-
GEnetic Factors for OSteoporosis Consortium
- IV:
-
Instrumental variable
- Apo B:
-
Apolipoprotein B
- Apo A1:
-
Apolipoprotein A1
- meQTL:
-
Methylation quantitative trait loci
- MAF:
-
Minor allele frequency
References
Srivastava M, Deal C (2002) Osteoporosis in elderly: prevention and treatment. Clin Geriatr Med 18(3):529–555. https://doi.org/10.1016/s0749-0690(02)00022-8
Zhang Q, Zhou J, Wang Q, Lu C, Xu Y, Cao H, Xie X, Wu X, Li J, Chen D (2020) Association between bone mineral density and lipid profile in Chinese women. Clin Interv Aging 15(15):1649–1664. https://doi.org/10.2147/CIA.S266722
Tan A, Shu J, Huang H, Shao H, Yang J (2023) The correlation between the serum LDL-C/Apo B ratio and lumbar bone mineral density in young adults. BMC Musculoskelet Disord 24(1):213. https://doi.org/10.1186/s12891-023-06325-w
Ambrogini E, Que X, Wang S, Yamaguchi F, Weinstein RS, Tsimikas S, Manolagas SC, Witztum JL, Jilka RL (2018) Oxidation-specific epitopes restrain bone formation. Nat Commun 9(1):2193. https://doi.org/10.1038/s41467-018-04047-5
Zhao H, Li Y, Zhang M, Qi L, Tang Y (2021) Blood lipid levels in patients with osteopenia and osteoporosis:a systematic review and meta-analysis. J Bone Miner Metab 39(3):510–520. https://doi.org/10.1007/s00774-020-01189-9
Chen YY, Wang WW, Yang L, Chen WW, Zhang HX (2018) Association between lipid profiles and osteoporosis in postmenopausal women: a meta-analysis. Eur Rev Med Pharmacol Sci 22(1):1–9. https://doi.org/10.26355/eurrev_201801_14093
Sekula P, Del Greco MF, Pattaro C, Köttgen A (2016) Mendelian Randomization as an approach to assess causality using observational data. J Am Soc Nephrol 27(11):3253–3265. https://doi.org/10.1681/ASN.2016010098
Zheng HTOF, Forgetta V, Hsu YH, et.al. Whole-genome sequencing identifies EN1 as a determinant of bone density and fracture. Nature. 2015 526(7571):112–7. doi: https://doi.org/10.1038/nature14878. Epub 2015 Sep 14. PMID: 26367794; PMCID: PMC4755714.) and a meta-analysis (Medina-Gomez C, Kemp JP, Trajanoska K, et.al. Life-Course Genome-wide Association Study Meta-analysis of Total Body BMD and Assessment of Age-Specific Effects. Am J Hum Genet. 2018 Jan 4;102(1):88–102. doi:https://doi.org/10.1016/j.ajhg.2017.12.005. PMID: 29304378; PMCID: PMC5777980
Richardson TG, Sanderson E, Palmer TM, Ala-Korpela M, Ference BA, Davey Smith G, Holmes MV (2020) Evaluating the relationship between circulating lipoprotein lipids and apolipoproteins with risk of coronary heart disease: a multivariable Mendelian randomisation analysis. PloS Med 17(3):e1003062. https://doi.org/10.1371/journal.pmed.1003062
Bjornsson HT, Fallin MD, Feinberg AP (2004) An integrated epigenetic and genetic approach to common human disease. Trends Genet 20(8):350–358. https://doi.org/10.1016/j.tig.2004.06.009
Jones AC, Irvin MR, Claas SA, Arnett DK (2021) Lipid phenotypes and DNA methylation: a review of the literature. Curr Atheroscler Rep 23(11):71. https://doi.org/10.1007/s11883-021-00965-w
Dekkers KF, van Iterson M, Slieker RC et al (2016) Blood lipids influence DNA methylation in circulating cells. Genome Biol 17(1):138. https://doi.org/10.1186/s13059-016-1000-6
Zheng HF, Forgetta V, Hsu YH et al (2015) Whole-genome sequencing identifies EN1 as a determinant of bone density and fracture. Nature 526(7571):112–7. https://doi.org/10.1038/nature14878
Medina-Gomez C, Kemp JP, Trajanoska K et al (2018) Life-course genome-wide association study meta-analysis of total body BMD and assessment of age-specific effects. Am J Hum Genet 102(1):88–102. https://doi.org/10.1016/j.ajhg.2017.12.005
Richardson TG, Sanderson E, Palmer TM et al (2020) Evaluating the relationship between circulating lipoprotein lipids and apolipoproteins with risk of coronary heart disease: a multivariable Mendelian randomisation analysis. PloS Med 17(3):e1003062. https://doi.org/10.1371/journal.pmed.1003062
Willer CJ, Schmidt EM, Sengupta S et al (2013) Global lipids genetics consortium. Discovery and refinement of loci associated with lipid levels. Nat Genet 45(11):1274–1283. https://doi.org/10.1038/ng.2797
Ong JS, MacGregor S (2019) Implementing MR-PRESSO and GCTA-GSMR for pleiotropy assessment in Mendelian randomization studies from a practitioner’s perspective. Genet Epidemiol 43(6):609–616. https://doi.org/10.1002/gepi.22207
Burgess S, Davies NM, Thompson SG (2016) Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol 40(7):597–608
McRae AF, Marioni RE, Shah S et al (2018) Identification of 55,000 Replicated DNA Methylation QTL. Sci Rep 8:17605. https://doi.org/10.1038/s41598-018-35871-w
Wu Y, Zeng J, Zhang F et al (2018) Integrative analysis of omics summary data reveals putative mechanisms underlying complex traits. Nat Commun 9:918. https://doi.org/10.1038/s41467-018-03371-0
Sayols-Baixeras S, Subirana I, Lluis-Ganella C et al (2016) Identification and validation of seven new loci showing differential DNA methylation related to serum lipid profile: an epigenome-wide approach the REGICOR study. Hum Mol Genet 25(20):4556–4565. https://doi.org/10.1093/hmg/ddw285.Erratum.In:HumMolGenet.2019Apr15;28(8):1402.PMID:28173150;PMCID:PMC6284258
Zhu Z, Zhang F, Hu H et al (2016) Integration of summary data from GWAS and eQTL studies predicts complex trait gene targets. Nat Genet 48:481–487. https://doi.org/10.1038/ng.3538
Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, Laurin C, Burgess S, Bowden J, Langdon R, Tan VY, Yarmolinsky J, Shihab HA, Timpson NJ, Evans DM, Relton C, Martin RM, Davey Smith G, Gaunt TR, Haycock PC (2018) The MR-Base platform supports systematic causal inference across the human phenome. Elife 30(7):e34408. https://doi.org/10.7554/eLife.34408
Yuan S, Larsson S (2020) Causal associations of iron status with gout and rheumatoid arthritis, but not with inflammatory bowel disease. Clin Nutr 39(10):3119–3124. https://doi.org/10.1016/j.clnu.2020.01.019
Hemani G, Zheng J, Be Elsworth et al (2018) The MR-Base platform supports systematic causal inference across the human phenome. Elife. 7:e34408. https://doi.org/10.7554/eLife.34408
Huang W, Xiao J, Ji J, Chen L (2021) Association of lipid-lowering drugs with COVID-19 outcomes from a Mendelian randomization study. Elife 6(10):e73873. https://doi.org/10.7554/eLife.73873
Ghorabi S, Shab-Bidar S, Sadeghi O, Nasiri M, Khatibi SR, Djafarian K (2019) Lipid profile and risk of bone fracture: a systematic review and meta-analysis of observational studies. Endocr Res 44(4):168–184. https://doi.org/10.1080/07435800.2019.1625057
Ghadiri-Anari A, Mortezaii-Shoroki Z, Modarresi M, Dehghan A (2016) Association of lipid profile with bone mineral density in postmenopausal women in Yazd province. Int J Reprod Biomed 14(9):597–602
Go JH, Song YM, Park JH, Park JY, Choi YH (2012) Association between serum cholesterol level and bone mineral density at lumbar spine and femur neck in postmenopausal korean women. Korean J Fam Med 33(3):166–73. https://doi.org/10.4082/kjfm.2012.33.3.166
Qi T, Wu Y, Zeng J et al (2018) Identifying gene targets for brain-related traits using transcriptomic and methylomic data from blood. Nat Commun 9:2282. https://doi.org/10.1038/s41467-018-04558-1
Hemani G, Bowden J, Davey SG (2018) Evaluating the potential role of pleiotropy in Mendelian randomization studies. Hum Mol Genet 27(R2):R195–R208. https://doi.org/10.1093/hmg/ddy163
Zheng J, Baird D, Borges MC, Bowden J, Hemani G, Haycock P, Evans DM, Smith GD (2017) Recent developments in mendelian randomization studies. Curr Epidemiol Rep 4(4):330–345. https://doi.org/10.1007/s40471-017-0128-6
Miserez AR, Cao G, Probst LC, Hobbs HH (1997) Structure of the human gene encoding sterol regulatory element binding protein 2 (SREBF2). Genomics 40(1):31–40. https://doi.org/10.1006/geno.1996.4525
García-García AB, Martínez-Hervás S, Vernia S, Ivorra C, Pulido I, Martín-Escudero JC, Casado M, Carretero J, Real JT, Chaves FJ (2022) A very rare variant in SREBF2, a possible cause of hypercholesterolemia and increased glycemic levels. Biomedicines 10(5):1178. https://doi.org/10.3390/biomedicines10051178
Golic M, Stojanovska V, Bendix I, Wehner A, Herse F, Haase N, Kräker K, Fischer C, Alenina N, Bader M, Schütte T, Schuchardt M, van der Giet M, Henrich W, Muller DN, Felderhoff-Müser U, Scherjon S, Plösch T, Dechend R (2018) Diabetes mellitus in pregnancy leads to growth restriction and epigenetic modification of the Srebf2 gene in rat fetuses. Hypertension 71(5):911–920. https://doi.org/10.1161/HYPERTENSIONAHA.117.10782
Madduma Hewage S, Au-Yeung KKW, Prashar S, Wijerathne CUB, Karmin O, Siow YL (2022) Lingonberry improves hepatic lipid metabolism by targeting notch1 signaling. Antioxidants (Basel) 11(3):472. https://doi.org/10.3390/antiox11030472
Ibrahim DA, Elsebai EA, Fayed A, Abdelrahman AE (2022) Prognostic value of NOTCH1 and OCT4 in gastric carcinoma. Indian J Pathol Microbiol 65(2):328–335. https://doi.org/10.4103/IJPM.IJPM_871_20
Lu L, Wang Z, Zhang H, Liu T, Fang H (2022) Drynaria fortunei improves lipid profiles of elderly patients with postmenopausal osteoporosis via regulation of Notch1-NLRP3 inflammasome-mediated inflammation. Gynecol Endocrinol 38(2):176–180. https://doi.org/10.1080/09513590.2021.2015760
Hegarty KG, Drummond FJ, Daly M, Shanahan F, Molloy MG (2018) GREB1 genetic variants are associated with bone mineral density in Caucasians. J Bone Miner Metab 36(2):189–199. https://doi.org/10.1007/s00774-017-0823-x
Cheng M, Michalski S, Kommagani R (2018) Role for growth regulation by estrogen in breast cancer 1 (GREB1) in hormone-dependent cancers. Int J Mol Sci 19(9):2543. https://doi.org/10.3390/ijms19092543
He P, Meng XH, Zhang X, Lin X, Zhang Q, Jiang RL, Schiller MR, Deng FY, Deng HW (2020) Identifying pleiotropic SNPs associated with femoral neck and heel bone mineral density. Front Genet 22(11):772. https://doi.org/10.3389/fgene.2020.00772
Qin C, Diaz-Gallo LM, Tang B, Wang Y, Nguyen TD, Harder A, Lu Y, Padyukov L, Askling J, Hägg S (2023) Repurposing antidiabetic drugs for rheumatoid arthritis: results from a two-sample Mendelian randomization study. Eur J Epidemiol 38(7):809–819. https://doi.org/10.1007/s10654-023-01000-9
Acknowledgements
We thank all the researchers who provided publicly open GWAS summary data.
Funding
This work was supported by ShanXi Applied Basic Research Programme (Nos.201901D111409), Key Research and Development (R&D) Projects of Shanxi Province (No.201803D31134) and Taiyuan Science and Technology Programme (No.202201). All of the funding were gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
ZZ was responsible for the methodological design and data collation and visualisation of the figures. YD was responsible for the writing of the draft and grammatical touch-ups. JH provided the conceptualisation, revision and review of the draft and the financial support for the study. ZZ and YD contributed equally to the article.
Corresponding author
Ethics declarations
Conflict of interest
Zhaoliang Zhang, Yuchen Duan and Jianzhong Huo declare that they have no conflict of interest.
Ethical Approval
This study was conducted in accordance with the Declaration of Helsinki. All cited GWAS and other data have been approved by the relevant review boards.
Human and Animal Rights and Informed Consent
All Human and Animal Rights and Informed Consent statements can be found from the original GWAS.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Z., Duan, Y. & Huo, J. Lipid Metabolism, Methylation Aberrant, and Osteoporosis: A Multi-omics Study Based on Mendelian Randomization. Calcif Tissue Int 114, 147–156 (2024). https://doi.org/10.1007/s00223-023-01160-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-023-01160-6