Abstract
Purpose of Review
To describe medical therapies and mechanical circulatory support devices used in the treatment of acute right ventricular failure.
Recent Findings
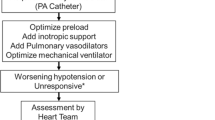
Experts have proposed several algorithms providing a stepwise approach to medical optimization of acute right ventricular failure including tailored volume administration, ideal vasopressor selection to support coronary perfusion, inotropes to restore contractility, and pulmonary vasodilators to improve afterload. Studies have investigated various percutaneous and surgically implanted right ventricular assist devices in several clinical settings.
Summary
The initial management of acute right ventricular failure is often guided by invasive hemodynamic data tracking parameters of circulatory function with the use of pharmacologic therapies. Percutaneous microaxial and centrifugal extracorporeal pumps bypass the failing RV and support circulatory function in severe cases of right ventricular failure.

Similar content being viewed by others
Abbreviations
- cGMP:
-
Cyclic guanosine monophosphate
- CO:
-
Cardiac output
- CVP:
-
Central venous pressure
- EF:
-
Ejection fraction
- ICU:
-
Intensive care unit
- iNO:
-
Inhaled nitric oxide
- LV:
-
Left ventricle
- LVAD:
-
Left ventricular assist device
- LVEDV:
-
Left ventricular end-diastolic volume
- MAP:
-
Mean arterial pressure
- MCS:
-
Mechanical circulatory support
- MI:
-
Myocardial infarction
- PA:
-
Pulmonary artery
- PADP:
-
Pulmonary artery diastolic pressure
- PAPi:
-
Pulmonary artery pulsatility index
- PASP:
-
Pulmonary artery systolic pressure
- PCWP:
-
Pulmonary capillary wedge pressure
- PE:
-
Pulmonary embolism
- PEEP:
-
Positive end-expiratory pressure
- PPV:
-
Positive pressure ventilation
- PVR:
-
Pulmonary vascular resistance
- RA:
-
Right atrium
- RAP:
-
Right atrial pressure
- RV:
-
Right ventricle
- RVAD:
-
Right ventricular assist device
- RVEDV:
-
Right ventricular end-diastolic volume
- RVSWI:
-
Right ventricular stroke work index
- SV:
-
Stroke volume
- VA ECMO:
-
Venoarterial extracorporeal membrane oxygenation
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Greyson CR. Pathophysiology of right ventricular failure. Crit Care Med. 2008;36(1 Suppl):S57-65. https://doi.org/10.1097/01.Ccm.0000296265.52518.70.
Konstam MA, Kiernan MS, Bernstein D, Bozkurt B, Jacob M, Kapur NK, et al. Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation. 2018;137(20):e578–622. https://doi.org/10.1161/cir.0000000000000560.
Dell’Italia LJ. Anatomy and physiology of the right ventricle. Cardiol Clin. 2012;30(2):167–87. https://doi.org/10.1016/j.ccl.2012.03.009.
Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117(13):1717–31. https://doi.org/10.1161/circulationaha.107.653584.
Friedberg MK, Redington AN. Right versus left ventricular failure: differences, similarities, and interactions. Circulation. 2014;129(9):1033–44. https://doi.org/10.1161/circulationaha.113.001375.
Mahmood SS, Pinsky MR. Heart-lung interactions during mechanical ventilation: the basics. Ann Transl Med. 2018;6(18):349. https://doi.org/10.21037/atm.2018.04.29.
Friedberg MK. Imaging right-left ventricular interactions. JACC Cardiovasc Imaging. 2018;11(5):755–71. https://doi.org/10.1016/j.jcmg.2018.01.028.
Cecconi M, Johnston E, Rhodes A. What role does the right side of the heart play in circulation? Crit Care. 2006;10(3):S5. https://doi.org/10.1186/cc4832.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing G-J, Harjola V-P, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543–603. https://doi.org/10.1093/eurheartj/ehz405.
Kapur NK, Esposito ML, Bader Y, Morine KJ, Kiernan MS, Pham DT, et al. Mechanical circulatory support devices for acute right ventricular failure. Circulation. 2017;136(3):314–26. https://doi.org/10.1161/circulationaha.116.025290.
Voelkel NF, Quaife RA, Leinwand LA, Barst RJ, McGoon MD, Meldrum DR, et al. Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation. 2006;114(17):1883–91. https://doi.org/10.1161/circulationaha.106.632208.
Saxena A, Garan AR, Kapur NK, O’Neill WW, Lindenfeld J, Pinney SP, et al. Value of hemodynamic monitoring in patients with cardiogenic shock undergoing mechanical circulatory support. Circulation. 2020;141(14):1184–97. https://doi.org/10.1161/circulationaha.119.043080.
Drazner MH, Velez-Martinez M, Ayers CR, Reimold SC, Thibodeau JT, Mishkin JD, et al. Relationship of right- to left-sided ventricular filling pressures in advanced heart failure: insights from the ESCAPE trial. Circ Heart Fail. 2013;6(2):264–70. https://doi.org/10.1161/circheartfailure.112.000204.
Tehrani BN, Truesdell AG, Psotka MA, Rosner C, Singh R, Sinha SS, et al. A standardized and comprehensive approach to the management of cardiogenic shock. JACC Heart Fail. 2020;8(11):879–91. https://doi.org/10.1016/j.jchf.2020.09.005.
Lim HS, Gustafsson F. Pulmonary artery pulsatility index: physiological basis and clinical application. Eur J Heart Fail. 2020;22(1):32–8. https://doi.org/10.1002/ejhf.1679.
Korabathina R, Heffernan KS, Paruchuri V, Patel AR, Mudd JO, Prutkin JM, et al. The pulmonary artery pulsatility index identifies severe right ventricular dysfunction in acute inferior myocardial infarction. Catheter Cardiovasc Interv. 2012;80(4):593–600. https://doi.org/10.1002/ccd.23309.
Mortensen CS, Kramer A, Schultz J, Lyhne MD, Nielsen-Kudsk JE, Andersen A. Impact of preload on right ventricular hemodynamics in acute pulmonary embolism. Crit Care Med. 2020;48(12):e1306–12. https://doi.org/10.1097/ccm.0000000000004643.
•• Ventetuolo CE, Klinger JR. Management of acute right ventricular failure in the intensive care unit. Ann Am Thorac Soc. 2014;11(5):811–22. https://doi.org/10.1513/AnnalsATS.201312-446FR. This review discusses right ventricular pathophysiology and offers guidance on medical therapies in the critically ill population.
Piazza G, Goldhaber SZ. The acutely decompensated right ventricle: pathways for diagnosis and management. Chest. 2005;128(3):1836–52. https://doi.org/10.1378/chest.128.3.1836.
Mercat A, Diehl JL, Meyer G, Teboul JL, Sors H. Hemodynamic effects of fluid loading in acute massive pulmonary embolism. Crit Care Med. 1999;27(3):540–4. https://doi.org/10.1097/00003246-199903000-00032.
Ternacle J, Gallet R, Mekontso-Dessap A, Meyer G, Maitre B, Bensaid A, et al. Diuretics in normotensive patients with acute pulmonary embolism and right ventricular dilatation. Circ J. 2013;77(10):2612–8. https://doi.org/10.1253/circj.cj-13-0404.
Labrada L, Romero C, Sadek A, Belardo D, Raza Y, Forfia P. Intravenous diuresis in severe precapillary pulmonary-hypertension-related right heart failure: effects on renal function and blood pressure. J Clin Med. 2023;12(22):7149.
Spotnitz HM, Berman MA, Epstein SE. Pathophysiology and experimental treatment of acute pulmonary embolism. Am Heart J. 1971;82(4):511–20. https://doi.org/10.1016/0002-8703(71)90236-5.
Kato R, Pinsky MR. Personalizing blood pressure management in septic shock. Ann Intensive Care. 2015;5(1):41. https://doi.org/10.1186/s13613-015-0085-5.
Ghignone M, Girling L, Prewitt RM. Volume expansion versus norepinephrine in treatment of a low cardiac output complicating an acute increase in right ventricular afterload in dogs. Anesthesiology. 1984;60(2):132–5. https://doi.org/10.1097/00000542-198402000-00009.
Kerbaul F, Rondelet B, Motte S, Fesler P, Hubloue I, Ewalenko P, et al. Effects of norepinephrine and dobutamine on pressure load-induced right ventricular failure. Crit Care Med. 2004;32(4):1035–40. https://doi.org/10.1097/01.ccm.0000120052.77953.07.
Pérez-Nieto OR, Gómez-Oropeza I, Quintero-Leyra A, Kammar-García A, Zamarrón-López ÉI, Soto-Estrada M, et al. Hemodynamic and respiratory support in pulmonary embolism: a narrative review. Front Med (Lausanne). 2023;10:1123793. https://doi.org/10.3389/fmed.2023.1123793.
•• Price LC, Wort SJ, Finney SJ, Marino PS, Brett SJ. Pulmonary vascular and right ventricular dysfunction in adult critical care: current and emerging options for management: a systematic literature review. Crit Care. 2010;14(5):R169. https://doi.org/10.1186/cc9264. This review is a comprehensive summary of the evidence and guidelines in the medical management of right ventricular failure.
Wang H, Gong M, Zhou B, Dai A. Comparison of inhaled and intravenous milrinone in patients with pulmonary hypertension undergoing mitral valve surgery. Adv Ther. 2009;26(4):462–8. https://doi.org/10.1007/s12325-009-0019-4.
Hansen MS, Andersen A, Nielsen-Kudsk JE. Levosimendan in pulmonary hypertension and right heart failure. Pulm Circ. 2018;8(3):2045894018790905. https://doi.org/10.1177/2045894018790905.
Ichinose F, Roberts JD Jr, Zapol WM. Inhaled nitric oxide: a selective pulmonary vasodilator: current uses and therapeutic potential. Circulation. 2004;109(25):3106–11. https://doi.org/10.1161/01.Cir.0000134595.80170.62.
Cheifetz IM. Cardiorespiratory interactions: the relationship between mechanical ventilation and hemodynamics. Respir Care. 2014;59(12):1937–45. https://doi.org/10.4187/respcare.03486.
Cortes-Puentes GA, Oeckler RA, Marini JJ. Physiology-guided management of hemodynamics in acute respiratory distress syndrome. Ann Transl Med. 2018;6(18):353. https://doi.org/10.21037/atm.2018.04.40.
Alkhunaizi FA, Burkhoff D, Brener MI. Right-sided mechanical circulatory support - a hemodynamic perspective. Curr Heart Fail Rep. 2022;19(5):334–45. https://doi.org/10.1007/s11897-022-00562-1.
DeFilippis EM, Topkara VK, Kirtane AJ, Takeda K, Naka Y, Garan AR. Mechanical circulatory support for right ventricular failure. Card Fail Rev. 2022;8: e14. https://doi.org/10.15420/cfr.2021.11.
Anderson MB, Goldstein J, Milano C, Morris LD, Kormos RL, Bhama J, et al. Benefits of a novel percutaneous ventricular assist device for right heart failure: the prospective RECOVER RIGHT study of the Impella RP device. J Heart Lung Transplant. 2015;34(12):1549–60. https://doi.org/10.1016/j.healun.2015.08.018.
Elder M, Blank N, Kaki A, Alraies MC, Grines CL, Kajy M, et al. Mechanical circulatory support for acute right ventricular failure in the setting of pulmonary embolism. J Interv Cardiol. 2018;31(4):518–24. https://doi.org/10.1111/joic.12503.
Cohen GI, Schreiber T, Singh H, Kaki A. Percutaneous thrombectomy and right ventricular mechanical circulatory support for pulmonary embolism in a coronavirus disease 2019 patient: case report, 1-year update, and echocardiographic findings. Eur Heart J Case Rep. 2022;6(1):ytac008. https://doi.org/10.1093/ehjcr/ytac008.
Anderson M, Morris DL, Tang D, Batsides G, Kirtane A, Hanson I, et al. Outcomes of patients with right ventricular failure requiring short-term hemodynamic support with the Impella RP device. J Heart Lung Transplant. 2018;37(12):1448–58. https://doi.org/10.1016/j.healun.2018.08.001.
Botti G, Gramegna M, Burzotta F, Masiero G, Briguori C, Trani C, et al. Impella RP for patients with acute right ventricular failure and cardiogenic shock: a subanalysis from the IMP-IT registry. J Pers Med. 2022;12(9). https://doi.org/10.3390/jpm12091481.
Elder M, Blank N, Shemesh A, Pahuja M, Kaki A, Mohamad T, et al. Mechanical circulatory support for high-risk pulmonary embolism. Interv Cardiol Clin. 2018;7(1):119–28. https://doi.org/10.1016/j.iccl.2017.09.002.
•• Akhmerov A, Ramzy D. Mechanical circulatory support in right ventricular failure. Interv Cardiol Clin. 2021;10(2):185–94. https://doi.org/10.1016/j.iccl.2020.12.010. This review provides a comprehensive overview over mechanical circulatory support options in right ventricular failure.
• Kuroda T, Miyagi C, Fukamachi K, Karimov JH. Mechanical circulatory support devices and treatment strategies for right heart failure. Front Cardiovasc Med. 2022;9: 951234. https://doi.org/10.3389/fcvm.2022.951234. This review discusses temporary and durable mechanical circulatory support options in right ventricular failure.
Alam A, Baran DA, Doshi H, Van Zyl J, Patlolla S, Salem M, et al. Safety and efficacy of ProtekDuo right ventricular assist device: a systemic review. Artif Organs. 2023;47(7):1094–103. https://doi.org/10.1111/aor.14525.
Leidenfrost J, Prasad S, Itoh A, Lawrance CP, Bell JM, Silvestry SC. Right ventricular assist device with membrane oxygenator support for right ventricular failure following implantable left ventricular assist device placement. Eur J Cardiothorac Surg. 2016;49(1):73–7. https://doi.org/10.1093/ejcts/ezv116.
Lee TML, Bianchi P, Kourliouros A, Price LC, Ledot S. Percutaneous oxygenated right ventricular assist device for pulmonary embolism: a case series. Artif Organs. 2023;47(3):595–603. https://doi.org/10.1111/aor.14420.
Kapur NK, Paruchuri V, Jagannathan A, Steinberg D, Chakrabarti AK, Pinto D, et al. Mechanical circulatory support for right ventricular failure. JACC Heart Fail. 2013;1(2):127–34. https://doi.org/10.1016/j.jchf.2013.01.007.
Ravichandran AK, Baran DA, Stelling K, Cowger JA, Salerno CT. Outcomes with the tandem Protek Duo dual-lumen percutaneous right ventricular assist device. ASAIO J. 2018;64(4):570–2. https://doi.org/10.1097/MAT.0000000000000709.
Salna M, Garan AR, Kirtane AJ, Karmpaliotis D, Green P, Takayama H, et al. Novel percutaneous dual-lumen cannula-based right ventricular assist device provides effective support for refractory right ventricular failure after left ventricular assist device implantation. Interact Cardiovasc Thorac Surg. 2020;30(4):499–506. https://doi.org/10.1093/icvts/ivz322.
Chopski SG, Murad NM, Fox CS, Stevens RM, Throckmorton AL. Mechanical circulatory support of the right ventricle for adult and pediatric patients with heart failure. ASAIO J. 2019;65(2):106–16. https://doi.org/10.1097/MAT.0000000000000815.
Takayama H, Naka Y, Kodali SK, Vincent JA, Addonizio LJ, Jorde UP, et al. A novel approach to percutaneous right-ventricular mechanical support. Eur J Cardiothorac Surg. 2012;41(2):423–6. https://doi.org/10.1016/j.ejcts.2011.05.041.
John R, Long JW, Massey HT, Griffith BP, Sun BC, Tector AJ, et al. Outcomes of a multicenter trial of the Levitronix CentriMag ventricular assist system for short-term circulatory support. J Thorac Cardiovasc Surg. 2011;141(4):932–9. https://doi.org/10.1016/j.jtcvs.2010.03.046.
Bhama JK, Bansal U, Winger DG, Teuteberg JJ, Bermudez C, Kormos RL, et al. Clinical experience with temporary right ventricular mechanical circulatory support. J Thorac Cardiovasc Surg. 2018;156(5):1885–91. https://doi.org/10.1016/j.jtcvs.2018.04.094.
Friedman O, Horowitz JM, Ramzy D. Advanced cardiopulmonary support for pulmonary embolism. Tech Vasc Interv Radiol. 2017;20(3):179–84. https://doi.org/10.1053/j.tvir.2017.07.007.
Pavlushkov E, Berman M, Valchanov K. Cannulation techniques for extracorporeal life support. Ann Transl Med. 2017;5(4):70. https://doi.org/10.21037/atm.2016.11.47.
Boulate D, Luyt CE, Pozzi M, Niculescu M, Combes A, Leprince P, et al. Acute lung injury after mechanical circulatory support implantation in patients on extracorporeal life support: an unrecognized problem. Eur J Cardiothorac Surg. 2013;44(3):544–9; discussion 9–50. https://doi.org/10.1093/ejcts/ezt125.
Pan P, Yan P, Liu D, Wang X, Zhou X, Long Y, et al. Outcomes of VA-ECMO with and without left centricular (LV) decompression using intra-aortic balloon pumping (IABP) versus other LV decompression techniques: a systematic review and meta-analysis. Med Sci Monit. 2020;26: e924009. https://doi.org/10.12659/MSM.924009.
Koeckert MS, Jorde UP, Naka Y, Moses JW, Takayama H. Impella LP 2.5 for left ventricular unloading during venoarterial extracorporeal membrane oxygenation support. J Card Surg. 2011;26(6):666–8. https://doi.org/10.1111/j.1540-8191.2011.01338.x.
Kopanczyk R, Al-Qudsi OH, Uribe A, Periel L, Fiorda-Diaz J, Abdel-Rasoul M, et al. Right ventricular dysfunction in patients with coronavirus disease 2019 supported with extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2022;36(2):629–31. https://doi.org/10.1053/j.jvca.2021.05.019.
Zochios V, Parhar K, Tunnicliffe W, Roscoe A, Gao F. The right ventricle in ARDS. Chest. 2017;152(1):181–93. https://doi.org/10.1016/j.chest.2017.02.019.
George B, Parazino M, Omar HR, Davis G, Guglin M, Gurley J, et al. A retrospective comparison of survivors and non-survivors of massive pulmonary embolism receiving veno-arterial extracorporeal membrane oxygenation support. Resuscitation. 2018;122:1–5. https://doi.org/10.1016/j.resuscitation.2017.11.034.
Guliani S, Das Gupta J, Osofsky R, Kraai EP, Mitchell JA, Dettmer TS, et al. Venoarterial extracorporeal membrane oxygenation is an effective management strategy for massive pulmonary embolism patients. J Vasc Surg Venous Lymphat Disord. 2021;9(2):307–14. https://doi.org/10.1016/j.jvsv.2020.04.033.
Ius F, Hoeper MM, Fegbeutel C, Kuhn C, Olsson K, Koigeldiyev N, et al. Extracorporeal membrane oxygenation and surgical embolectomy for high-risk pulmonary embolism. Eur Respir J. 2019;53(4). https://doi.org/10.1183/13993003.01773-2018.
Yusuff HO, Zochios V, Vuylsteke A. Extracorporeal membrane oxygenation in acute massive pulmonary embolism: a systematic review. Perfusion. 2015;30(8):611–6. https://doi.org/10.1177/0267659115583377.
Hoeper MM, Benza RL, Corris P, de Perrot M, Fadel E, Keogh AM, et al. Intensive care, right ventricular support and lung transplantation in patients with pulmonary hypertension. Eur Respir J. 2019;53(1). https://doi.org/10.1183/13993003.01906-2018 .
Joshi Y, Bories MC, Aissaoui N, Grinda JM, Bel A, Latremouille C, et al. Percutaneous venopulmonary artery extracorporeal membrane oxygenation for right heart failure after left ventricular assist device insertion. Interact Cardiovasc Thorac Surg. 2021;33(6):978–85. https://doi.org/10.1093/icvts/ivab197.
Riebandt J, Haberl T, Wiedemann D, Moayedifar R, Schloeglhofer T, Mahr S, et al. Extracorporeal membrane oxygenation support for right ventricular failure after left ventricular assist device implantation. Eur J Cardiothorac Surg. 2018;53(3):590–5. https://doi.org/10.1093/ejcts/ezx349.
Author information
Authors and Affiliations
Contributions
EY wrote the main manuscript text, created Table 1. MC wrote the main manuscript text, created Table 2. OF wrote the main manuscript text. JH wrote the main manuscript text.
Corresponding author
Ethics declarations
Conflict of Interest
James M. Horowitz reports consulting fees from Inari Medical and Penumbra for clinical trial design. The other authors report no conflict of interest pertinent to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuriditsky, E., Chonde, M., Friedman, O. et al. Medical and Mechanical Circulatory Support of the Failing Right Ventricle. Curr Cardiol Rep 26, 23–34 (2024). https://doi.org/10.1007/s11886-023-02012-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-02012-3