Abstract
Background
Insomnia disorder is associated with an impairment in cognitive performance. Doxepin and zolpidem have been found to be effective in improving sleep. In this study, we aimed to compare the effects of doxepin and zolpidem on sleep structure and executive function in patients with insomnia disorder.
Methods
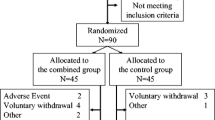
Patients with primary insomnia were randomly assigned to receive doxepin 6 mg/day orally or zolpidem 5–10 mg/day orally. Polysomnography (PSG) and the Pittsburgh Sleep Quality Index (PSQI) were used at baseline and after the 8-week treatment to compare clinical efficacy in the two groups. Safety was assessed using the Treatment Emergent Symptom Scale (TESS). Executive function was evaluated using the Wisconsin sorting card test (WSCT).
Results
Of 120 patients enrolled in the study, 60 participants were assigned to each group. A total of 109 participants (53 in the doxepin group and 56 in the zolpidem group) completed the study. After treatment, the wake after sleep onset (WASO) and total sleep time (TST) values in the doxepin group were 80.3 ± 21.4 min and 378.9 ± 21.9 min, respectively, which were significantly better than those in the zolpidem group (132.9 ± 26.5 min and 333.2 ± 24.2 min, respectively; (P < 0.05)). The sleep onset latency (SOL) value in the zolpidem group (20.3 ± 4.7 min) was significantly better than that in the doxepin group (28.2 ± 5.6 min; P < 0.05). The sleep efficiency (SE) in the doxepin group was 77.8 ± 4.2%, which was significantly better than that in the zolpidem group (68.6 ± 5.0%; P < 0.05). The PSQI score of the doxepin group was 6.1 ± 1.1, which was significantly lower than that in the zolpidem group (7.9 ± 1.9; P < 0.05). The treatment adverse events in the doxepin group was 23.3%, which was significantly higher than that in the zolpidem group (13.3%; P < 0.05). The WSCT showed a significant improvement in persistent errors (PE), random errors (RE), and categories in the two groups after 8-week treatment, and the improvement in RE and the categories was more obvious in the doxepin group (P < 0.05).
Conclusions
Both doxepin and zolpidem were found to be effective in improving sleep quality, but the effects exhibited different patterns. Doxepin improved executive function more effectively than zolpidem in patients with insomnia disorder.
Similar content being viewed by others
Data availability
The data that support our findings are available from the corresponding author upon reasonable request.
References
Bhaskar S, Hemavathy D, Prasad S (2016) Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J Family Med Prim Care 5(4):780–784
Feige B, Baglioni C, Spiegelhalder K, Hirscher V, Nissen C, Riemann D (2013) The microstructure of sleep in primary insomnia: an overview and extension. Int J Psychophysiol 89(2):171–180
Roane BM, Taylor DJ (2008) Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep 31(10):1351–1356
Ozminkowski RJ, Wang S, Walsh JK (2007) The direct and indirect costs of untreated insomnia in adults in the United States. Sleep 30(3):263–273
Krystal AD, Prather AA, Ashbrook LH (2019) The assessment and management of insomnia: an update. World Psychiatry 18(3):337–352
Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, Morin CM (2012) Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev 16(1):83–94
Liu H, Wang D, Li Y, Li Z, Zhang Y, Lei F, Du L, Tang X (2014) Examination of daytime sleepiness and cognitive performance testing in patients with primary insomnia. PLoS ONE 9(6):e100965
Kalmbach DA, Cheng P, Arnedt JT, Cuamatzi-Castelan A, Atkinson RL, Fellman-Couture C, Roehrs T, Drake CL (2019) Improving daytime functioning, work performance, and quality of life in postmenopausal women with insomnia: comparing cognitive behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. J Clin Sleep Med 15(7):999–1010
Yaffe K (2014) Cherie M Falvey, Tina Hoang: Connections between sleep and cognition in older adults. Lancet Neurol 13(10):1017–1028
Brownlow JA, Miller KE, Gehrman PR (2020) Insomnia and cognitive performance. Sleep Med Clin 15(1):71–76
Climent-Martinez G, Luna-Lario P, Bombin-Gonzalez I, Cifuentes-Rodriguez A, Tirapu-Ustarroz J, Diaz-Orueta U (2014) Neuropsychological evaluation of the executive functions by means of virtual reality. Rev Neurol 58(10):465–475
Zambrano-Sanchez E, Martinez-Cortes JA, Rio-Carlos YD, Martinez-Wbaldo Mdel C, Poblano A (2010) Executive dysfunction screening and intelectual coefficient measurement in children with attention deficit hyperactivity disorder. Arq Neuropsiquiatr 68(4):545–549
Muto V, Shaffii-le Bourdiec A, Matarazzo L, Foret A, Mascetti L, Jaspar M, Vandewalle G, Phillips C, Degueldre C, Balteau E et al (2012) Influence of acute sleep loss on the neural correlates of alerting, orientating and executive attention components. J Sleep Res 21(6):648–658
Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M (2008) Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med 4(5):487–504
Yeung WF, Chung KF, Yung KP, Ng TH (2015) Doxepin for insomnia: a systematic review of randomized placebo-controlled trials. Sleep Med Rev 19:75–83
Krystal AD, Lankford A, Durrence HH, Ludington E, Jochelson P, Rogowski R, Roth T (2011) Efficacy and safety of doxepin 3 and 6 mg in a 35-day sleep laboratory trial in adults with chronic primary insomnia. Sleep 34(10):1433–1442
Weber J, Siddiqui MA, Wagstaff AJ, McCormack PL (2010) Low-dose doxepin: in the treatment of insomnia. CNS Drugs 24(8):713–720
Food and Drug Administration (2013) FDA approved drug products. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm
Association AP (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Washington, DC, pp 361–365
Liu X, Tang M, Hu L, Wang A, Wu H, Zhao G, Gao C, Li W (1996) Reliability and vallidity of the Pittsburgh Sleep Quality Index. Chin J Psychiatry 29(2):103–107
Zhang M (2003) Handbook of psychiatric rating scale. Hunan Science and Technology Press, Changsha, pp 81–201
Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G (1993) Wisconsin card sorting test manual, revised and expanded. Odessa, Psychological Assessment Resources, Florida
Lezak MD (1995) Neuropsychological assessment, 3rd edn. Oxford University Press, New York
Paolo S, Pietro D, Andrea R, Alessandro R (2005) Executive function assessment of patients with schizophrenic disorder residual type in olanzapine treatment: an open study. Hum Psychopharmacol 20(6):401–408
Wu J, Chang F, Zu H (2015) Efficacy and safety evaluation of citalopram and doxepin on sleep quality in comorbid insomnia and anxiety disorders. Exp Ther Med 10(4):1303–1308
Bettica P, Squassante L, Groeger JA, Gennery B, Winsky-Sommerer R, Dijk DJ (2012) Differential effects of a dual orexin receptor antagonist (SB-649868) and zolpidem on sleep initiation and consolidation, SWS, REM sleep, and EEG power spectra in a model of situational insomnia. Neuropsychopharmacology 37(5):1224–1233
Bu J, Zu H (2017) Mechanism underlying the effects of doxepin on beta-amyloid -induced memory impairment in rats. Iran J Basic Med Sci 20(9):1044–1049
Covassin N, de Zambotti M, Sarlo M, De Min TG, Sarasso S, Stegagno L (2011) Cognitive performance and cardiovascular markers of hyperarousal in primary insomnia. Int J Psychophysiol 80(1):79–86
Joo EY, Kim H, Suh S, Hong SB (2014) Hippocampal substructural vulnerability to sleep disturbance and cognitive impairment in patients with chronic primary insomnia: magnetic resonance imaging morphometry. Sleep 37(7):1189–1198
Rongve A, Boeve BF, Aarsland D (2010) Frequency and correlates of caregiver-reported sleep disturbances in a sample of persons with early dementia. J Am Geriatr Soc 58(3):480–486
Zhao WR (2017) The impaired inhibitory control of insomnia disorder: evidence from stop signal task and resting-state EEG rhythms. Southwest University, Chongqing, China
Acknowledgements
We thank the patient who participates in our study. We are grateful to the funding of this study.
Funding
Funding for this study was provided by Hangzhou Science and technology development plan project (No. 20180533B81(Li HAN were responsible for collecting clinical data and performing the clinical rating), No. 20160533B30 (Zhenghe YU were responsible for study design and data analysis)), Project for Hangzhou Medical Disciplines of Excellence, Key Project for Hangzhou Medical Disciplines.
Author information
Authors and Affiliations
Contributions
SW and ZY were responsible for study design. LH, LR, YX, WL, LM, YW, LY, and YL were responsible for collecting clinical data and performing the clinical rating. SW and PY were responsible for analysis and manuscript. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Hangzhou Seventh People’s Hospital. The purpose and importance of the study were explained to the participant. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Written informed consent was obtained from the patient for publication of this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, Z., Han, L., Yan, P. et al. Doxepin is more effective than zolpidem in improving executive function in patients with insomnia disorder. Sleep Breath (2023). https://doi.org/10.1007/s11325-023-02972-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11325-023-02972-4