Abstract
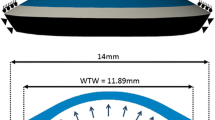
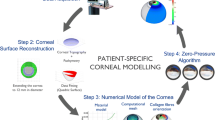
We present a patient-specific finite element model of the human cornea that accounts for the presence of the epithelium. The thin anterior layer that protects the cornea from the external actions has a scant relevance from the mechanical point of view, and it has been neglected in most numerical models of the cornea, which assign to the entire cornea the mechanical properties of the stroma. Yet, modern corneal topographers capture the geometry of the epithelium, which can be naturally included into a patient-specific solid model of the cornea, treated as a multi-layer solid. For numerical applications, the presence of a thin layer on the anterior cornea requires a finer discretization and the definition of two constitutive models (including the corresponding properties) for stroma and epithelium. In this study, we want to assess the relevance of the inclusion of the epithelium in the model of the cornea, by analyzing the effects in terms of uncertainties of the mechanical properties, stress distribution across the thickness, and numerical discretization. We conclude that if the epithelium is modeled as stroma, the material properties should be reduced by 10%. While this choice represents a sufficiently good approximation for the simulation of in vivo mechanical tests, it might result into an under-estimation of the postoperative stress in the simulation of refractive surgery.









Similar content being viewed by others
References
Agca A, Ozgurhan EB, Demirok A, Bozkurt E, Celik U, Ozkaya A, Cankaya I, Yilmaz OF (2014) Comparison of corneal hysteresis and corneal resistance factor after small incision lenticule extraction and femtosecond laser-assisted lasik: a prospective fellow eye study. Contact Lens Anterior Eye 37(2):77–80
Alastrué V, Calvo B, Peña E, Doblaré M (2006) Biomechanical modeling of refractive corneal surgery. J Biomech Eng 128(1):150–160
Ariza-Gracia MÁ, Ortillés Á, Cristóbal JÁ, Rodríguez Matas JF, Calvo B (2017) A numerical-experimental protocol to characterize corneal tissue with an application to predict astigmatic keratotomy surgery. J Mech Behav Biomed Mater 74:304–314
Bongiorno T, Chojnowski JL, Lauderdale JD, Sulchek T (2016) Cellular stiffness as a novel stemness marker in the corneal limbus. Biophys J 111(8):1761–1772
Bryant MR, Marchi V, Juhasz T (2000) Mathematical models of picosecond laser in situ keratomileusis for high myopia. J Refract Surg 16:155–162
Bryant MR, McDonnell PJ (1996) Constitutive laws for biomechanical modeling of refractive surgery. J Biomech Eng
Cabrera Fernandez D, Niazy AM, Kurtz RM, Djotyan GP, Juhasz T (2005) Finite element analysis applied to cornea reshaping. J Biomed Optics 10(6):064018
Deenadayalu C, Mobasher B, Rajan SD, Hall GW (2006) Refractive change induced by the LASIK flap in a biomechanical finite element model
Elsheikh A, McMonnies CW, Whitford C, Boneham GC (2015) In vivo study of corneal responses to increased intraocular pressure loading. Eye and Vision, 2(1), All Open Access. Gold Open Access, Green Open Access
Elsheikh A, Ross S, Alhasso D, Rama P (2009) Numerical study of the effect of corneal layered structure on ocular biomechanics. Curr Eye Res 34(1):26–35
Falgayrettes N, Patoor E, Cleymand F, Zevering Y, Perone JM (2023) Biomechanics of keratoconus: two numerical studies. PLoS ONE
Jayasuriya AC, Scheinbeim JI, Lubkin V, Bennett G, Kramer P (2003) Piezoelectric and mechanical properties in bovine cornea. J Biomed Mater Res A 66A:260–265
Last JA, Liliensiek SJ, Nealey PF, Murphy CJ (2009) Determining the mechanical properties of human corneal basement membranes with atomic force microscopy. J Struct Biol 167(1):19–24
Last JA, Thomasy SM, Croasdale CR, Russell P, Murphy CJ (2012) Compliance profile of the human cornea as measured by atomic force microscopy. Micron 43(12):1293–1298
Masterton S, Ahearne M (2018) Mechanobiology of the corneal epithelium. Exp Eye Res 177:122–129
Meek KM, Boote C (2009) The use of X-ray scattering techniques to quantify the orientation and distribution of collagen in the corneal stroma. Prog Retin Eye Res 28(5):369–392
Montanino A, Angelillo M, Pandolfi A (2019) A 3d fluid-solid interaction model of the air puff test in the human cornea. J Mech Behav Biomed Mater 94:22–31
Montanino A, Gizzi A, Vasta M, Angelillo M, Pandolfi A (2018) Modeling the biomechanics of the human cornea accounting for local variations of the collagen fibril architecture. ZAMM-J Appl Math Mech /Zeitschrift für Angewandte Mathematik und Mechanik 98(12):2122–2134
Montanino A, Pandolfi A (2020) On the recovery of the stress-free configuration of the human cornea. Modell Artif Intell Ophthalmol 4:11–33
Montanino A, van Overbeeke S, Pandolfi A (2023) Modelling the biomechanics of laser corneal refractive surgery. J Mech Behavior Biomed Mater, 105998
Pandolfi A, Boschetti F (2015) The influence of the geometry of the porcine cornea on the biomechanical response of inflation tests. Comput Methods Biomech Biomed Engin 18(1):64–77
Pandolfi A, Manganiello F (2006) A model for the human cornea: constitutive formulation and numerical analysis. Biomech Model Mechanobiol 5(4):237–246
Pandolfi A, Vasta M (2012) Fiber distributed hyperelastic modeling of biological tissues. Mech Mater 44:151–162
Petsche SJ, Pinsky PM (2013) The role of 3-d collagen organization in stromal elasticity: a model based on X-ray diffraction data and second harmonic-generated images. Biomech Model Mechanobiol 12:1101–1113
Sánchez P, Moutsouris K, Pandolfi A (2014) Biomechanical and optical behavior of human corneas before and after photorefractive keratectomy. J Cataract Refract Surg 40(6):905–917
Seven I, Vahdati A, Pedersen IB, Vestergaard A, Hjortdal J, Roberts CJ, Dupps WJ (2017) Contralateral eye comparison of smile and flap-based corneal refractive surgery: computational analysis of biomechanical impact. J Refract Surg 33(7):444–453
Simonini I, Pandolfi A (2015) Customized finite element modelling of the human cornea. PLoS ONE 10(6):e0130426
Sinha-Roy A, Dupps WJ (2009) Effects of altered corneal stiffness on native and postoperative LASIK corneal biomechanical behavior: a whole-eye finite element analysis. J Refract Surg 25(10):875–887
Sinha-Roy A, Dupps W. J (2011) Patient-specific modeling of corneal refractive surgery outcomes and inverse estimation of elastic property changes. J Biomech Eng, 133(1),
Sinha-Roy A, Dupps WJ, Roberts CJ (2014) Comparison of biomechanical effects of small-incision lenticule extraction and laser in situ keratomileusis: finite-element analysis. J Cataract Refract Surg 40(6):971–980
Straehla JP, Limpoco FT, Dolgova NV, Keselowsky BG, Sawyer WG, Perry SS (2010) Nanomechanical probes of single corneal epithelial cells: shear stress and elastic modulus. Tribol Lett 38:107–113
Studer HP, Riedwyl H, Amstutz CA, Hanson James VM, Büchler P (2013) Patient-specific finite-element simulation of the human cornea: a clinical validation study on cataract surgery. J Biomech 46(4):751–758
Thomasy SM, Raghunathan VK, Winkler M, Reilly CM, Sadeli AR, Russell P, Jester JV, Murphy CJ (2014) Elastic modulus and collagen organization of the rabbit cornea: epithelium to endothelium. Acta Biomater 10(2):785–791
Torres-Netto EA, Hafezi F, Spiru B, Gilardoni F, Hafezi NL, Gomes JAP, Randleman JB, Sekundo W, Kling S (2021) Contribution of bowman layer to corneal biomechanics. J Cataract Refract Surg 47(7):927–932
Whitford C, Studer H, Boote C, Meek KM, Elsheikh A (2015) Biomechanical model of the human cornea: considering shear stiffness and regional variation of collagen anisotropy and density. J Mech Behav Biomed Mater 42:76–87
Acknowledgements
The financial support of the iVis Technologies, Taranto, is gratefully acknowledged. A special thank goes to Giuseppe D’Ippolito and Giuseppe Criscenti. The research has been developed under the auspices of the Italian National Group of Physics–Mathematics (GNFM) of the Italian National Institution of High Mathematics “Francesco Severi” (INDAM).
Author information
Authors and Affiliations
Corresponding author
Appendix A: Constitutive model of the stroma
Appendix A: Constitutive model of the stroma
We model the stroma as a hyperelastic composite, made of an elastic matrix (made of proteoglycans) reinforced with two sets of dispersed collagen fibrils (Pandolfi and Vasta 2012). The uncertainty of the fibril orientation is described with a von Mises distribution (Pandolfi and Vasta 2012) about a main orientation \({\textbf{a}}_M\), with \(M=1,2\). The strain energy density is assumed to decompose additively into volumetric, isotropic–isochoric, and anisotropic–isochoric parts in the form
where \({\textbf{F}}= d{\textbf{x}}/d{\textbf{X}}\) is the deformation gradient, \({\textbf{x}}\) are the current coordinates and \({\textbf{X}}\) the reference coordinates, and \(J = \det {\textbf{F}}\) is the Jacobian determinant. \({\overline{\textbf{C}}}={\overline{\textbf{F}}}^T {\overline{\textbf{F}}}=J^{-2/3}{\textbf{F}}^T{\textbf{F}}\) is the isochoric Cauchy–Green deformation tensor, and \({\overline{I}_1}\) and \({\overline{I}_2}\) are the first and the second invariants of \({\overline{\textbf{C}}}\),
where \(\mathrm tr (.)\) denotes the trace operator. The average pseudo-invariant \({\overline{I}^*_{4\, M}}\) is defined as
where \(\kappa _M\) is a dispersion parameter, \(\otimes \) is the tensor product, and ( : ) is the double contraction product. The variance operator \({\sigma ^2_{I_4\, M}}\) is defined as
The mathematical form of the energies are
where K is the bulk modulus, \(\mu = \mu _1 + \mu _2\) is the shear modulus of the soft isotropic matrix, while \(k_{1\,M}\) (stiffness-like parameter) and \(k_{2\,M}\) (dimensionless rigidity parameters) control the mechanical response of the reinforcing fibers at low and high strains, respectively. The coefficient \(D^*({\overline{I}^*_{4\, M}})\) reads
and the coefficient \(K^*\)
The model parameters are seven: five with the dimension of a stiffness (shear elastic moduli), i.e., K, \(\mu _1\), \(\mu _2\), \(k_{1\,1}\), \(k_{1\,2}\) , and two dimensionless rigidity coefficients \(k_{2\,1}\), \(k_{2\, 2}\). The interested reader is referred to the original work (Pandolfi and Vasta 2012).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Montanino, A., Pandolfi, A. The inclusion of the epithelium in numerical models of the human cornea. Biomech Model Mechanobiol (2023). https://doi.org/10.1007/s10237-023-01801-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10237-023-01801-7