Abstract
Intracranial schwannomas are relatively uncommon, accounting for approximately 8% of all intracranial tumors, while intracerebral schwannomas represent an even rarer entity, responsible for roughly 1% of all intracranial schwannomas. After reviewing the relevant literature, we discussed the clinical journey of a 74-year-old woman who presented with a 3-week history of dizziness and nausea. Magnetic resonance imaging revealed a right temporal mass lesion with perifocal edema. The initial suspicion was the diagnosis of a glioblastoma or metastasis, prompting surgical intervention. During the surgery, a gross total resection of a noninvasive tumor was successfully performed. The patient’s postoperative recovery was uneventful. Histopathological examination and confirmatory immunohistochemistry played a crucial role in reaching the final diagnosis of an intracerebral temporal schwannoma, highlighting the diagnostic challenges posed by radiologically indistinguishable features from metastasis and gliomas. Despite these challenges, complete surgical removal remains the most preferred treatment option, resulting in a favorable long-term prognosis without the need for adjuvant or neoadjuvant chemotherapy. Intracerebral schwannomas are exceedingly rare brain tumors, often found on the brain’s surface or adjacent ventricles. Early and accurate diagnosis can be challenging due to radiological features overlapping with other intracranial pathologies. Nonetheless, histopathological examination and immunohistochemistry remain indispensable tools in establishing a definitive diagnosis and guiding effective treatment strategies. With complete surgical excision, patients with intracerebral schwannomas can expect a positive outcome and a promising long-term prognosis. Further research and case studies are warranted to enhance our understanding of these rare tumors and improve patient outcomes.
Similar content being viewed by others
Introduction
Schwannomas are a type of tumor that originates from Schwann cells, which form the myelin sheath of peripheral nerves. They account for approximately 8% of all primary brain tumors, with the majority (80–90%) being located in the cerebellopontine angle in association with the vestibular nerve [1]. However, when schwannomas occur without any relation to cranial nerves, they are considered intracerebral schwannomas (IS) [2]. These tumors are extremely rare and are often associated with neurofibromatosis type 2 (NF2). These intracerebral schwannomas account for less than 1% of all intracranial schwannomas. The first documented case of intracerebral schwannoma was reported by Gibson et al. in 1966 [2].
To the best of our knowledge and according to the latest literature review made in 2021, there were 150 reported cases in the literature with a majority occurring before the age of 30 and a slight male predominance. Only 7 cases of patients older than 70 years have been reported [3].
In our manuscript, we report a case of 74-year-old women with temporomesial schwannoma. This case report follows the CARE Guidelines [4].
Methods
In the present study, we report a new case of intracerebral schwannoma. In addition, we performed a literature research using the PubMed electronic database using the following medical subject heading (Mesh) terms: intracerebral schwannoma, schwannoma, brain tumor. The keywords were used separately and/or in different combinations. Only cases report of intracerebral schwannoma in old patients (> = 70 years old) were considered.
Case Description
History and Presentation
The patient is a 74-year-old female presented after a 3-week history of dizziness and nausea. The dizziness was described as a feeling of unsteadiness, exacerbated when lying down and turning to the side while lying down, leading to accompanying nausea and vomiting. Initial evaluation revealed a right temporal mass lesion with perifocal edema on a CT scan and MRI. For further investigation, the patient was transferred to our department (Fig. 1). It is also important to note that our patient suffered from arterial hypertension, hypercholesterolemia, glaucoma, and reflux esophagitis.
Imaging
An initial imaging (MRI cranial without contrast, MRI cranial with diffusion tensor imaging (DTI) and MRI cranial vascular angiography) confirmed the presence of a contrast-enhancing mass lesion in the right temporomesial region observed in conjunction with the pre-contrast MRI. It measured approximately 36 × 32 mm in the current T2 axial image. There were hypo-intensities (Fig. 2).
In the right frontal region, there were two small areas with increased signal intensity on diffusion-weighted imaging (DWI), corresponding to decreased apparent diffusion coefficient (ADC) values and increased signal on T2-weighted images.
Compared to the previous images (FIRST MRT), there were a slight increase in the size of the ventricles. Measurement of the lateral ventricle anterior horns on the axial image showed a current width of 41 mm, previously measuring 37 mm. There was no significant midline shift observed. The apical and basal cisterns were clearly delineated (Fig. 2).
The arterial time-of-flight (TOF) angiography showed no abnormalities in the anterior cerebral artery (ACA), middle cerebral artery (MCA), or internal carotid artery (ICA). The vertebral and basilar arteries appeared normal. A small outpouching was seen caudally at the transition from the right P1 to P2 segment of the posterior communicating artery (PCA), measuring approximately 2 × 2 mm in the TOF angiography (Fig. 2).
Surgical Procedure
The patient underwent a right temporal craniotomy. Guided by neuronavigation, a total microsurgical excision of the lesion was achieved. During the surgery, the tumor appeared well demarcated and firm, distinct from the brain tissue. Multiple samples were taken for histopathological examination. The tumor exhibited a high degree of vascularity and was partially firm-grayish-yellow in appearance.
Postoperative Course
After the surgery, the patient was transferred to the monitoring unit. On the following day, with stable neurological and cardiopulmonary condition, the patient was transferred to the general ward. The patient was mobilized at a rapid pace on the ward. The postoperative course was uneventful. No new neurological deficits were observed. The wound was dry and non-irritated. The postoperative cranial CT control showed a regular postoperative status without bleeding or obstruction.
Pathological Findings
The neuropathologist received 10.72 g of tissue, consisting of a large, gray, and firm tissue fragment measuring 3.9 × 2.4 × 0.7 cm.
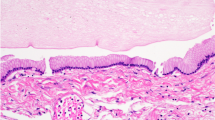
The histological sections demonstrate a densely cellular mesenchymal tumor. The tumor exhibited both, a compact and a loosely arranged, partially mucinous tissue matrix. Some areas showed a high cellularity. The tumor partly abutted vascular endothelium, while in other areas, tumor vessels demonstrated hyalinized walls and perivascular fibrous cuffs. The tumor cells showed a dense reticulin fiber network (Gomori’s silver impregnation). Pleomorphic elongated cell nuclei were observed in some areas. Individual mitotic figures were present. There was no evidence of tumor tissue necrosis (Fig. 3 A, B).
Histology of the intracerebral schwannoma. The tumor is mainly composed of mesenchymal cells with elongated nuclei (H&E-stain, A) that exhibited subtle basal membranes, as shown by the silver impregnation according to Gomori as fine lines around the cells (B). The immunohistochemical characterization is the nuclear and cytoplasmic S-100 antibodyreactivity, shown by the brown color reaction (C). The proliferative activity, demonstrates with the antibody Ki67 (=MIB1) as nuclear brown staining is moderate (D)
In some areas, the tumor was in direct contact with brain tissue. No leptomeningeal structures were visible between the brain and tumor tissue. A sharp demarcation of the tumor bulk was seen, and the brain tissue showed a reactive astrocytic gliosis with a gemistocytic reaction. Some remaining glia cells and some axons were visible in between the tumor bulk, arguing for an infiltrative growth of the tumor (Fig. 4).
Sharp border between brain tissue (left) and tumor bulk (right, H&E stain, A). Whereas the silver impregnation according to Gomori demonstrates the subtle basal membranes in the tumor tissue, the brain tissue is free of it (B). Densely arranged clumsy astrocytes, immunoreactive for the glial fibrillary acidic protein (GFAP, brown color), are seen in the brain tissue (left) adjacent to the tumor (right) and as single cells in the tumor (C). Whereas a dense axon staining is seen in the brain tissue using an antibody against neurofilament, only some axons are visible in the tumor tissue (D)
By immunohistiochemical antibody staining, it could be demonstrated that the tumor cells showed a nuclear and cytoplastic expression of S-100 (Fig. 3C), but no expression of the glial fibrillary acidic protein (GFAP) (Fig. 4C), no expression of the epithelial membrane antigene (EMA; data not shown), and no nuclear redistribution of the signal transducer and activator of transcription 6 (STAT6; data not shown). Together with the histological appearance, this identifies the tumor as a schwannoma WHO grade 1 and excludes a glioma, a meningioma, and a solitary fibrous tumor (SFT).
Genetic Findings
For further characterization of the schwannoma, an analysis of allelic losses from tumor cells on the long arm of chromosome 22 was conducted using microsatellite analysis. Four different microsatellites were analyzed for the characterization of a regional loss of chromosome 22, located between 22q11.23 and 22q13.1. The analysis was performed on a high-resolution Spreadex EL 800 gel in the Origins electrophoresis system by Elchrom Systems. The DNA extracted from the schwannoma tissue shows an allelic loss on the long arm of chromosome 22 in comparison to DNA extraction from patients’ blood (Fig. 5).
PCR-based microsatellite analysis reveals heterozygous allelic losses in the tumor tissue in for at least 3 (D22S445, D22S684, D22S268) out of 4 microsatellite markers (A). The location of the microsatellites is indicated by black lines on chromosome 22 (B). Legend: B, blood DNA; T, tumor DNA, M, marker of size
To confirm these findings, fluorescence in situ hybridization (FISH) was performed in native tumor tissue. Two-color hybridization DNA probes were used to detect the chromosomal regions 22q11.2 and 1p36.3 (MetaSystems GmbH). The procedure has been performed in previous studies in our neurosurgery research laboratory [5, 6]. Signals were analyzed with an Olympus BX43 fluorescence microscope based on the criteria of Hopman et al. [7].
The outcome of the FISH, as shown in Fig. 6, indicated the deletion of the chromosomal region 22q11.2. We could also observe an internal heterogeneity showing cells with a deletion on chromosome 22q.11.2, while others showed an intact 22q11.2. Furthermore, we could demonstrate no deletions of the chromosomal region 1p36.3 in the investigated cells (Fig. 6). Taken together, this suggests that some tumor cells are affected by extensive loss of chromosome 22q, ranging, at least, from 22q11.2 to 22q12.3.
Literature Review
A total of 6 articles describing 7 patients were included in our study (Table 1) [3, 8,9,10,11,12]. Among these seven patients (male = 2, female = 5), three underwent a subtotal resection of the tumor, and the rest underwent complete resection or gross total resection of the tumor. One of the patients was treated, after the gross tumor resection, by intensity-modulated radiation therapy (IMRT) with 37.5 Gy, delivered to the resection cavity in 15 fractions because a malignant intracerebral nerve sheath tumor was diagnosed. This entity is extremely rare compared to benign intracerebral schwannoma [12]. The vast majority of tumor cells show a lack of differentiation by S-100 negativity.
The reason for a subtotal resection was the tumor location. Weiner et al. reported a tumor intimately adjoining the brainstem [10], and Casedei et al. reported tumors extending to the medulla and into basal ganglia [8].
Discussion
Schwannomas originating from Schwann cells, which typically form the myelin sheath of peripheral nerves, are commonly found in cranial and peripheral nerves. However, intracerebral schwannomas are rare and have attracted speculation regarding their origin [8]. Various theories have been proposed to explain the development of this tumor, categorized as developmental and non-developmental theories. The developmental theory suggests distorted embryogenesis as the source of aberrant foci of Schwann cells in the brain parenchyma. This may involve the transformation of developed mesenchymal pial cells into Schwann cells, differentiation of multi potential mesenchymal elements, ectopic migration of neural crest cells, or misplaced myelinated nerve fibers [13, 14]. Conversely, the non-developmental theory proposes that intracerebral Schwann cells arise from the perivascular nerve plexus of parenchymal arterioles [15]. Schwannomas are frequent in patients carrying an autosomal dominant mutation in the gene NF2, which codes for the tumor-suppressor protein merlin (Moesin-Ezrin-Radixin-like protein). The gene of this protein is located on chromosome 22q.12.2 in proximity to the microsatellite marker D22S268. With two independent methods, we can demonstrate a somatic heterozygote loss of chromosome 22q in the tumor of the present patient, which may contribute to the tumor development. In the case of intracerebral schwannoma, which comprises less than 1% of surgically treated central and peripheral nervous system schwannomas, the lesions are predominantly supratentorial, either superficial or periventricular [3]. Most cases in the last literature review have been reported in younger individuals, with the majority presenting below the age of 30 [3]. Uncommon locations of ectopic schwannomas have also been described, such as the third and fourth ventricles, intrasellar region, and pontomedulary cistern with extension into the dorsal spinal cord. Radiological features of intracerebral schwannoma on CT and MRI include cystic formations, calcifications, and peritumoral edema. However, these imaging findings are not pathognomonic, leading to occasional misdiagnoses, such as mistaking schwannoma for meningiomas based on tentorial involvement and the presence of a dural tail sign [16, 17]. Actually, the diagnosis of this intracerebral schwannoma is almost never made preoperatively.
Histopathological analysis is crucial for distinguishing IS from other tumors, such as pilocytic astrocytoma, pleomorphic xanthoastrocytoma, ganglioglioma, solitary fibrous tumors, and meningioma. Differential diagnosis can be challenging, particularly between fibroblastic meningioma, the solitary fibrous tumor and an Antoni A cell-predominant schwannoma, or pilomyxoid/pilocytic astrocytoma and Antoni B cell-predominant schwannoma. Additional diagnostic tools, i.e., immunohistochemical analyses, are necessary to differentiate these entities. Intracerebral schwannoma typically exhibits positive staining for S-100, SOX10, and calretinine, while staining negative for EMA, GFAP, and STAT6 [18,19,20]. In addition, in the current epigenetic Heidelberg Brain Tumor Classifier v12.8, “MC CNS Schwannoma, VGLL-fused” is introduced as a provisional new class. The editors of this brain tumor classifier explained that this kind of tumor represents a very rare group of intracranial tumors with morphological and immunohistochemically features of schwannoma. These tumors often display fusions of the VGLL gene family (VGLL2 or VGLL3), which have also been reported for a subset of peripheral schwannoma. This type of schwannoma is a provisional class, which is still being further characterized [21].
For intracerebral schwannoma, surgery is the primary treatment, with complete resection often resulting in a favorable long-term outcome. Total removal of the tumor is typically curative, as evidenced in cases where long-term follow-up demonstrated no recurrence. A recurrence rate of 5.3% has been documented after GTR primarily attributed to the presence of malignant histopathology within the tumor [3]. In cases that underwent subtotal resection, 20% of the tumors with no malignant pathology needed a second surgery, proposing that recurrence is due to incomplete tumor removal [3]. In the presented case, total tumor removal was achieved, as confirmed by postoperative CT scan.
Conclusion
In conclusion, intracerebral schwannoma represents a rare variant of schwannoma, characterized by its intracerebral location and atypical features. The origin of these tumors remains an area of ongoing research, with both developmental and non-developmental theories proposed. Accurate diagnosis requires careful evaluation of histopathological features and the use of ancillary diagnostic techniques. Surgical resection is the preferred treatment approach, aiming for complete removal whenever possible, which often leads to favorable long-term outcomes. Further studies are warranted to elucidate the underlying mechanisms and optimal management strategies for this rare entity.
Data Availability
All data underlying the results are available as part of the article and no additional source data are required.
Abbreviations
- EMA:
-
Epithelial membrane antigen
- GFAP:
-
Glial fibrillary acidic protein
- GTR:
-
Gross total resection
- N.A:
-
Not applicable
- NF2:
-
Neurofibromatosis type 2
- STAT6:
-
Signal transducer and activator of transcription 6
- STR:
-
Subtotal resection
- TOF:
-
Time of flight
- VGLL:
-
Vestigial-like family
References
McLendon R, Rosenblum M, Bigner D. Russell & Rubinstein’s Pathology of Tumors of the Nervous System 7 Ed. 7th ed. Aufl. London: CRC Press; 2012. https://doi.org/10.1201/b13439.
Deora H, Srinivas D, Beniwal M, Vikas V, Rao KVLN, Somanna S. Rare cranial nerve schwannomas: a retrospective review of nontrigeminal, nonvestibular cranial nerve schwannomas. J Neurosci Rural Pract. 2018;9(2):258–63. https://doi.org/10.4103/jnrp.jnrp_469_17.
Kovalainen A, Haeren R, Paetau A, Lehecka M. Brainstem intraparenchymal schwannoma: a case report and literature review. Surg Neurol Int. 2021;12:508. https://doi.org/10.25259/SNI_621_2021.
Riley DS. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218–35. https://doi.org/10.1016/j.jclinepi.2017.04.026.
Hemmer S, Urbschat S, Oertel J, Ketter R. Deletions in the 17q chromosomal region and their influence on the clonal cytogenetic evolution of recurrent meningiomas. Mol Cytogenet. 2019;12:22. https://doi.org/10.1186/s13039-019-0434-4.
Lerner C, Ketter R, Linsler S, Henn W, Oertel J, Urbschat S. Establishment of a molecular cytogenetic analysis for native tumor tissue of meningiomas-suitable for clinical application. Mol Cytogenet. 2014;7:12. https://doi.org/10.1186/1755-8166-7-12.
Hopman AH. In situ hybridization as a tool to study numerical chromosome aberrations in solid bladder tumors. Histochemistry. 1988;89(4):307–16. https://doi.org/10.1007/BF00500631.
Casadei GP, Komori T, Scheithauer BW, Miller GM, Parisi JE, Kelly PJ. Intracranial parenchymal schwannoma: a clinicopathological and neuroimaging study of nine cases. J Neurosurg. 1993;79(2):217–22. https://doi.org/10.3171/jns.1993.79.2.0217.
Sharma RR, Gurusinghe NT, Lynch PG, Parekh HC, Bertolis G. Intraparenchymatous schwannoma of the cerebellum. Br J Neurosurg. 1993;7(1):83–9. https://doi.org/10.3109/02688699308995061.
Weiner HL, Zagzag D, Babu R, Weinreb HJ, Ransohoff J. Schwannoma of the fourth ventricle presenting with hemifacial spasm. A report of two cases. J Neurooncol. 1993;15(1):37–43. https://doi.org/10.1007/BF01050261.
Luo W, Ren X, Chen S, Liu H, Sui D, Lin S. Intracranial intraparenchymal and intraventricular schwannomas: report of 18 cases. Clin Neurol Neurosurg. 2013;115(7):1052–7. https://doi.org/10.1016/j.clineuro.2012.10.029.
Barnard ZR. Sporadic primary malignant intracerebral nerve sheath tumors: case report and literature review. J Neurooncol. 2011;104(2):605–10. https://doi.org/10.1007/s11060-011-0531-7.
Redekop G, Elisevich K, Gilbert J. Fourth ventricular schwannoma: case report. J Neurosurg. 1990;73(5):777–81. https://doi.org/10.3171/jns.1990.73.5.0777.
Esiri M. Russell and Rubinstein’s Pathology of Tumors of the Nervous System. Sixth Edition. J Neurol Neurosurg Psych. 2000;68(4):538. https://doi.org/10.1136/jnnp.68.4.538d.
Adelman LS, Aronson SM. Intramedullary nerve fiber and Schwann cell proliferation within the spinal cord (schwannosis). Neurology. 1972;22(7):726–31. https://doi.org/10.1212/wnl.22.7.726.
Takei H, Schmiege L, Buckleair L, Goodman JC, Powell SZ. Intracerebral schwannoma clinically and radiologically mimicking meningioma. Pathol Int. 2005;55(8):514–9. https://doi.org/10.1111/j.1440-1827.2005.01862.x.
Menkü A, Oktem IS, Kontaş O, Akdemir H. Atypical intracerebral schwannoma mimicking glial tumor: case report. Turk Neurosurg. 2009;19(1):82–5.
Khoo HM, Taki T. Periventricular intraparenchymal schwannoma. Neurologia medico-chirurgica. 2012;52(8):603–7. https://doi.org/10.2176/nmc.52.603.
Ten H, Adachi K, Yamaguchi F, Matsuno A, Teramoto A, Morita A. Occipital lobe epilepsy was presented in a patient with intracerebral schwannoma: a case report and literature review. Int J Neurosci. 2019;129(3):308–12. https://doi.org/10.1080/00207454.2018.1526797.
Jessen KR, Mirsky R. The origin and development of glial cells in peripheral nerves. Nat Rev Neurosci. 2005;6(9):9. https://doi.org/10.1038/nrn1746.
Abstracts of the 20th International Congress of Neuropathology Berlin, Germany, September 13 - 16, 2023. Brain pathol. 2023;33(Suppl 1(Suppl 1)):e13194. PS1‐NO‐A53.VGLL‐altered CNS schwannoma is a new tumor entity with distinct DNA‐methylation profile and recurrent gene fusions of either VGLL3 or VGLL1. https://doi.org/10.1111/bpa.13194.
Acknowledgements
The authors want to thank S. Welsch and H. Blatt for their technical support on the molecular cytogenetic analysis.
Code Availability
Not applicable
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Scientific support and paper writing: MH (1)
Surgery and paper writing: SL (1)
FISH based analysis and paper writing: SU (1)
Pathological analysis and LOH: WJS-S, JB-K (2)
Magnet resonance imaging: MG (3)
Principal investigator: JO (1)
Idea, scientific support, statistical analysis, surgery and paper writing: RK (1)
Corresponding author
Ethics declarations
Consent to Participate
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Consent for Publication
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Henia, M., Linsler, S., Schulz-Schaeffer, W.J. et al. Intracranial Intracerebral Schwannoma: a Case Report and Review of the Literature. SN Compr. Clin. Med. 5, 289 (2023). https://doi.org/10.1007/s42399-023-01631-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01631-9