Abstract
Purpose of the Review
Magnetoencephalography (MEG) is a functional neuroimaging technique that records neurophysiology data with millisecond temporal resolution and localizes it with subcentimeter accuracy. Its capability to provide high resolution in both of these domains makes it a powerful tool both in basic neuroscience as well as clinical applications. In neurology, it has proven useful in its ability to record and localize epileptiform activity. Epilepsy workup typically begins with scalp electroencephalography (EEG), but in many situations, EEG-based localization of the epileptogenic zone is inadequate. The complementary sensitivity of MEG can be crucial in such cases, and MEG has been adopted at many centers as an important resource in building a surgical hypothesis. In this paper, we review recent work evaluating the extent of MEG influence of presurgical evaluations, novel analyses of MEG data employed in surgical workup, and new MEG instrumentation that will likely affect the field of clinical MEG.
Recent Findings
MEG consistently contributes to presurgical evaluation and these contributions often change the plan for epilepsy surgery. Extensive work has been done to develop new analytic methods for localizing the source of epileptiform activity with MEG. Systems using optically pumped magnetometry (OPM) have been successfully deployed to record and localize epileptiform activity.
Summary
MEG remains an important noninvasive tool for epilepsy presurgical evaluation. Continued improvements in analytic methodology will likely increase the diagnostic yield of the test. Novel instrumentation with OPM may contribute to this as well, and may increase accessibility of MEG by decreasing cost.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Carreno M, Lüders HO. Chap. 47: General principles of presurgical evaluation. In: Lüders HO, editor. Textbook of epilepsy surgery. 2008. p. 409–22.
Ebersole JS, Ebersole SM. Combining MEG and EEG source modeling in epilepsy evaluations. J Clin Neurophysiol. 2010;27:360–71. https://doi.org/10.1097/WNP.0b013e318201ffc4.
Piastra MC, Nu¨ßing A, Vorwerk J, Clerc M, Engwer C, Wolters CH. A comprehensive study on electroencephalography and magnetoencephalography sensitivity to cortical and subcortical sources. Hum Brain Mapp. 2021;42:978–92. https://doi.org/10.1002/hbm.25272. A detailed modeling study comparing relative sensitivities of EEG and MEG for different brain regions. EEG was found to more sensitive for radial and deep sources, and MEG more sensitive for tangential sources.
Mikuni N, Nagamine T, Ikeda A, Terada K, Taki W, Kimura J, Kikuchi H, Shibasaki H. Simultaneous recording of epileptiform discharges by MEG and subdural electrodes in temporal lobe epilepsy. Neuroimage. 1997;5:298–306. https://doi.org/10.1006/nimg.1997.0272.
Okada YC, Lahteenmäki A, Xu C. Experimental analysis of distortion of magnetoencephalography signals by the skull. Clin Neurophysiol. 1999;110:230–8. https://doi.org/10.1016/S0013-4694(98)00099-6.
Okada Y, Lahteenmaki A, Xu C. Comparison of MEG and EEG on the basis of somatic evoked responses elicited by stimulation of the snout in the juvenile swine. Clin Neurophysiol. 1999;110:214–29. https://doi.org/10.1016/S0013-4694(98)00111-4.
Hämäläinen MS, Hari R, Ilmoniemi RJ, Knuutila J, Lounasmaa OV. Magnetoencephalography—theory, instrumentation, and applications to noninvasive studies of the working human brain. Rev Mod Phys. 1993;65:413–515.
Tamilia E, AlHilani M, Tanaka N, Tsuboyama M, Peters JM, Grant PE, Madsen JR, Stufflebeam SM, Pearl PL, Papadelis C. Assessing the localization accuracy and clinical utility of electric and magnetic source imaging in children with epilepsy. Clin Neurophysiol. 2019;130:491–504. https://doi.org/10.1016/j.clinph.2019.01.009. A study comparing localization accuracy for EEG and MEG, utilizing intracranial EEG and resection as the ground truth. MEG was found to have smaller localization error than both conventional and high-density scalp EEG.
Bagić AI, Knowlton RC, Rose DF, Ebersole JS. American Clinical Magnetoencephalography Society clinical practice guideline 1: recording and analysis of spontaneous cerebral activity. J Clin Neurophysiol. 2011;0:1. https://doi.org/10.1097/WNP.0b013e3182272fed.
Burgess RC, Funke ME, Bowyer SM, Lewine JD, Kirsch HE, Bagić AI. American Clinical Magnetoencephalography Society clinical practice guideline 2: presurgical functional brain mapping using magnetic evoked fields. J Clin Neurophysiol. 2011;28:1. https://doi.org/10.1097/WNP.0b013e3182272ffe.
Bagić AI, Knowlton RC, Rose DF, Ebersole JS. American Clinical Magnetoencephalography Society clinical practice guideline 3. J Clin Neurophysiol. 2011;0:1. https://doi.org/10.1097/WNP.0b013e3182272fed.
Bagić AI, Knowlton RC, Rose DF, Ebersole JS. American Clinical Magnetoencephalography Society clinical practice guideline 4. J Clin Neurophysiol. 2011;0:1. https://doi.org/10.1097/WNP.0b013e3182272fed.
Tenney JR, Fujiwara H, Rose DF. The value of source localization for clinical magnetoencephalography: beyond the equivalent current dipole. J Clin Neurophysiol. 2020;37:537–44. https://doi.org/10.1097/WNP.0000000000000487.
Bowyer SM, Zillgitt AJ, Greenwald M, Lajiness-O’Neill R. Language mapping with magnetoencephalography: an update on the current state of clinical research and practice with considerations for clinical practice guidelines. J Clin Neurophysiol. 2020;37:554–63. https://doi.org/10.1097/WNP.0000000000000489.
De Tiège X, Bourguignon M, Piitulainen H, Jousmäki V. Sensorimotor mapping with MEG: an update on the current state of clinical research and practice with considerations for clinical practice guidelines. J Clin Neurophysiol. 2020;37:564–73. https://doi.org/10.1097/WNP.0000000000000481.
Zillgitt AJ, Barkley GL, Bowyer SM. Visual mapping with magnetoencephalography: an update on the current state of clinical research and practice with considerations for clinical practice guidelines. J Clin Neurophysiol. 2020;37:585–91. https://doi.org/10.1097/WNP.0000000000000483.
Shvarts V, Mäkelä JP. Auditory mapping with MEG: an update on the current state of clinical research and practice with considerations for clinical practice guidelines. J Clin Neurophysiol. 2020;37:574–84. https://doi.org/10.1097/WNP.0000000000000518.
Laohathai C, Ebersole JS, Mosher JC, Bagić AI, Sumida A, Von Allmen G, Funke ME. Practical fundamentals of clinical MEG interpretation in epilepsy. Front Neurol. 2021;12:1–22. https://doi.org/10.3389/fneur.2021.722986. An excellent overview of clinical MEG as used for epilepsy.
Fischer MJ, Scheler G, Stefan H. Utilization of magnetoencephalography results to obtain favourable outcomes in epilepsy surgery. Brain. 2005;128:153–7. https://doi.org/10.1093/brain/awh333.
Mouthaan BE, Rados M, Boon PAJM, Carrette E, Diehl B, Jung J, Kimiskidis VK, Kobulashvili T, Kuchukhidze G, Larsson PG, Leitinger M, Ryvlin P, Rugg-Gunn F, Seeck M, Vulli’emoz S, Huiskamp G, Lei-jten FSS, Van Eijsden P, Trinka E, Braun KPJ. Diagnostic accuracy of interictal source imaging in presurgical epilepsy evaluation: a systematic review from the E-PILEPSY consortium. Clin Neurophysiol. 2019;130:845–55. https://doi.org/10.1016/j.clinph.2018.12.016. A meta-analysis of several studies comparing the relative contributions of EEG and MEG to epilepsy presurgical evaluation. No statistical difference was found between the contributions of the two modalities.
Papanicolaou AC, Pataraia E, Billingsley-Marshall RL, Castillo EM, Wheless JW, Swank P, Breier JI, Sarkari S, Simos PG. Toward the substitution of invasive electroencephalography in epilepsy surgery. J Clin Neurophysiol. 2005;22:231–7. https://doi.org/10.1097/01.WNP.0000172255.62072.E8.
Knowlton RC, Elgavish RA, Bartolucci A, Ojha B, Limdi N, Blount J, Burneo JG, Ver Hoef L, Paige L, Faught E, Kankirawatana P, Riley K, Kuzniecky R. Functional imaging: II. Prediction of epilepsy surgery outcome. Ann Neurol. 2008;64:35–41. https://doi.org/10.1002/ana.21419.
Jeong W, Chung CK, Kim JS. Magnetoencephalography interictal spike clustering in relation with surgical outcome of cortical dysplasia. J Korean Neurosurg Soc. 2012;52:466–71. https://doi.org/10.3340/jkns.2012.52.5.466.
Schneider F, Irene Wang Z, Alexopoulos AV, Almubarak S, Kakisaka Y, Jin K, Nair D, Mosher JC, Najm IM, Burgess RC. Magnetic source imaging and ictal SPECT in MRI-negative neocortical epilepsies: additional value and comparison with intracranial EEG. Epilepsia. 2013;54:359–69. https://doi.org/10.1111/epi.12004.
Wilenius J, Medvedovsky M, Gaily E, Metsähonkala L, Mäkelä JP, Pae-tau A, Valanne L, Paetau R. Interictal MEG reveals focal cortical dysplasias: special focus on patients with no visible MRI lesions. Epilepsy Res. 2013;105:337–48. https://doi.org/10.1016/j.eplepsyres.2013.02.023.
Almubarak S, Alexopoulos A, Von-Podewils F, Wang ZI, Kakisaka Y, Mosher JC, Bulacio J, González-Martínez J, Bingaman W, Burgess RC. The correlation of magnetoencephalography to intracranial EEG in localizing the epileptogenic zone: a study of the surgical resection outcome. Epilepsy Res. 2014;108:1581–90. https://doi.org/10.1016/j.eplepsyres.2014.08.016.
Mu J, Rampp S, Carrette E, Roessler K, Sommer B, Schmitt FC, De Tiège X, Hamer HM, Boon PAJM, Pauli E, Blümcke I, Zhou D, Buchfelder M, Stefan H. Clinical relevance of source location in frontal lobe epilepsy and prediction of postoperative long-term outcome. Seizure. 2014;23:553–9. https://doi.org/10.1016/j.seizure.2014.04.006.
Kim H, Kankirawatana P, Killen J, Harrison A, Oh A, Rozzelle C, Blount J, Knowlton R. Magnetic source imaging (MSI) in children with neocortical epilepsy: surgical outcome association with 3D post-resection analysis. Epilepsy Res. 2013;106:164–72. https://doi.org/10.1016/j.eplepsyres.2013.04.004.
Murakami H, Wang ZI, Marashly A, Krishnan B, Prayson RA, Kakisaka Y, Mosher JC, Bulacio J, Gonzalez-Martinez JA, Bingaman WE, Najm IM, Burgess RC, Alexopoulos AV. Correlating magnetoencephalography to stereo-electroencephalography in patients undergoing epilepsy surgery. Brain a J Neurol. 2016;139:2935–47. https://doi.org/10.1093/brain/aww215.
Rampp S, Stefan H, Wu X, Kaltenhauser M, Maess B, Schmitt FC, Wolters CH, Hamer HM, Kasper BS, Schwab S, Doerfler A, Blumcke I, Rössler K, Buchfelder M. Magnetoencephalography for epileptic focus localization in a series of 1000 cases. Brain. 2019;142:3059–71. https://doi.org/10.1093/brain/awz231. A detailed retrospective study of a large cohort of patients who underwent MEG and epilepsy surgery. Extent of resection of MEG IZ was a postive prognostic factor.
He X, Zhou J, Teng P, Wang X, Guan Y, Zhai F, Li T, Luan G. The impact of MEG results on surgical outcomes in patients with drug-resistant epilepsy associated with focal encephalomalacia: a single-center experience. J Neurol. 2020;267:812–22. https://doi.org/10.1007/s00415-019-09638-w.
Chourasia N, Quach M, Gavvala J. Insular Magnetoencephalography dipole clusters in patients with refractory focal epilepsy. J Clin Neurophysiol. 2021;38:542–6. https://doi.org/10.1097/WNP.0000000000000718.
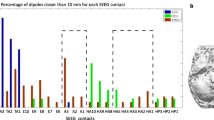
Ntolkeras G, Tamilia E, AlHilani M, Bolton J, Ellen Grant P, Prabhu SP, Madsen JR, Stufflebeam SM, Pearl PL, Papadelis C. Presurgical accuracy of dipole clustering in MRI-negative pediatric patients with epilepsy: validation against intracranial EEG and resection. Clin Neurophysiol. 2022;141:126–38. https://doi.org/10.1016/j.clinph.2021.01.036. This retrospective study evaluated dipole clustering for conventional and high-density scalp EEG as well as MEG. Dipole clustering was found to be a positive prognostic factor for surgical outcome.
Anand A, Magnotti JF, Smith DN, Gadot R, Najera RA, Hegazy MI, Gavvala JR, Shofty B, Sheth SA. Predictive value of magnetoencephalography in guiding the intracranial implant strategy for intractable epilepsy. J Neurosurg. 2022;137:1237–47. https://doi.org/10.3171/2022.1.JNS212943.
Oishi M, Kameyama S, Masuda H, Tohyama J, Kanazawa O, Sasagawa M, Otsubo H. Single and multiple clusters of magnetoencephalographic dipoles in neocortical epilepsy: significance in characterizing the epileptogenic zone. Epilepsia. 2006;47:355–64. https://doi.org/10.1111/j.1528-1167.2006.00428.x.
Englot DJ, Nagarajan SS, Imber BS, Raygor KP, Honma SM, Mizuiri D, Mantle M, Knowlton RC, Kirsch HE, Chang EF. Epileptogenic zone localization using magnetoencephalography predicts seizure freedom in epilepsy surgery. Epilepsia. 2015;56:949–58. https://doi.org/10.1111/epi.13002.
Zhang C, Liu W, Zhang J, Zhang X, Huang P, Sun B, Zhan S, Cao C. Utility of magnetoencephalography combined with stereo-electroencephalography in resective epilepsy surgery: a 2-year follow-up. Seizure. 2022;97:94–101. https://doi.org/10.1016/j.seizure.2022.03.013.
Duez L, Tankisi H, Hansen PO, Sidenius P, Sabers A, Pinborg LH, Fabricius M, Rubboli G, Pedersen B, Leffers AM, Uldall P, Jespersen B, Brennum J, Fuglsang-frederiksen A, Beniczky S. Electromagnetic source imaging in presurgical workup of patients with epilepsy. Neurology. 2019;92:e576–86. https://doi.org/10.1212/WNL.0000000000006877. A prospective study of combined EEG-MEG (EMSI) evaluating the consistency of localizations provided by different algorithms and across two popular software packages (Curry and BESA), as well as the diagnostic yield. EMSI was found to pro- vide new information in 34% of cases.
Plummer C, Vogrin SJ, Woods WP, Murphy MA, Cook MJ, Liley DTJ. Interictal and ictal source localization for epilepsy surgery using high-density EEG with MEG: a prospective long-term study. Brain. 2019;142:932–51. https://doi.org/10.1093/brain/awz015. A detailed retrospective study of patients who underwent both MEG and hd-EEG evaluating the localization accuracy of ECD solutions based on different latencies of the spike waveform, as validated against resection-based EZ. Earliest solutions were found to have greatest accuracy. MEG alone was not found to have superior localization accuracy.
Stefan H, Hummel C, Scheler G, Genow A, Druschky K, Tilz C, Kaltenhäuser M, Hopfengärtner R, Buchfelder M, Romstöck J. Magnetic brain source imaging of focal epileptic activity: a synopsis of 455 cases. Brain. 2003;126:2396–405. https://doi.org/10.1093/brain/awg239.
Pataraia E, Simos PG, Castillo EM, Billingsley-Marshall RL, Sarkari S, Wheless JW, Maggio V, Maggio W, Baumgartner JE, Swank PR, Breier JI, Papanicolaou AC. Does magnetoencephalography add to scalp video-EEG as a diagnostic tool in epilepsy surgery? Neurology. 2004;62:943–8. https://doi.org/10.1212/WNL.63.10.1987.
Paulini A, Fischer M, Rampp S, Scheler G, Hopfengärtner R, Kaltenhäuser M, Dörfler A, Buchfelder M, Stefan H. Lobar localization information in epilepsy patients: MEG-A useful tool in routine presurgical diagnosis. Epilepsy Res. 2007;76:124–30. https://doi.org/10.1016/j.eplepsyres.2007.07.006.
Colon AJ, Ossenblok PP, Nieuwenhuis L, Stam KJ, Boon PAJM. Use of routine MEG in the primary diagnostic process of epilepsy. J Clin Neurophysiol. 2009;26:326–32. https://doi.org/10.1097/WNP.0b013e3181baabef.
Koster I, Ossenblok PP, Brekelmans GJ, van der Linden I, Hillebrand A, Wijnen BF, Colon AJ. Sensitivity of magnetoencephalography as a diagnostic tool for epilepsy: a prospective study. Epileptic Disord. 2020;22:264–72. https://doi.org/10.1684/epd.2020.1160.
Duez L, Beniczky S, Tankisi H, Hansen PO, Sidenius P, Sabers A, Fuglsang-Frederiksen A. Added diagnostic value of magnetoencephalography (MEG) in patients suspected for epilepsy, where previous, extensive EEG workup was unrevealing. Clin Neurophysiol. 2016;127:3301–5. https://doi.org/10.1016/j.clinph.2016.08.006.
Sutherling WW, Mamelak AN, Thyerlei D, Maleeva T, Minazad Y, Philpott L, Lopez N. Influence of magnetic source imaging for planning intracranial EEG in epilepsy. Neurology. 2008;71:990–6. https://doi.org/10.1212/01.wnl.0000326591.29858.1a.
Mohamed IS, Toffa DH, Robert M, Cossette P, Bérubé AA, Saint-Hilaire JM, Bouthillier A, Nguyen DK. Utility of magnetic source imaging in nonlesional focal epilepsy: a prospective study. Neurosurg Focus. 2020;48:1–11. https://doi.org/10.3171/2020.1.FOCUS19877.
Tripathi M, Kaur K, Ramanujam B, Viswanathan V, Bharti K, Singh G, Singh V, Garg A, Bal CS, Tripathi M, Sharma MC, Pandey R, Dash D, Mandal P, Chandra PS. Diagnostic added value of interictal magnetic source imaging in presurgical evaluation of persons with epilepsy: a prospective blinded study. Eur J Neurol. 2021;28:2940–51. https://doi.org/10.1111/ene.14935.
Baule G, McFee R. Theory of magnetic detection of the heart’s electrical activity. J Appl Phys. 1965;36:2066–73. https://doi.org/10.1063/1.1714404.
Grynszpan F, Geselowitz DB. Model studies of the magnetocardiogram. Biophys J. 1973;13:911–25. https://doi.org/10.1016/S0006-3495(73)86034-5.
Cohen D, Hosaka H. Part II magnetic field produced by a current dipole. J Electrocardiol. 1976;9:409–17. https://doi.org/10.1016/S0022-0736(76)80041-6.
Cuffin BN, Cohen D. Magnetic fields produced by models of biological current sources. J Appl Phys. 1977;48:3971–80. https://doi.org/10.1063/1.324230.
Cuffin BN, Cohen D. Magnetic fields of a dipole in special volume conductor shapes. IEEE Trans Biomed Eng. 1977;24:372–81.
Sarvas J. Basic mathematical and electromagnetic concepts of the biomagnetic inverse problem. Phys Med Biol. 1987;32:11–22. https://doi.org/10.1088/0031-9155/32/1/004.
Marquardt DW. An algorithm for least-squares estimation of non-linear parameters. J Soc Ind Appl Math. 1963;11:431–41.
Knowlton RC, Laxer KD, Aminoff MJ, Roberts TP, Wong ST, Row-ley HA. Magnetoencephalography in partial epilepsy: clinical yield and localization accuracy. Ann Neurol. 1997;42:622–31. https://doi.org/10.1002/ana.410420413.
de Munk JC. A linear discretization of the volume conductor bound- ary integral equation using analytically integrated elements. IEEE Trans Biomed Eng. 1992;39:986–90.
Scherg M, Hari R, Hämäläinen MS. Frequency-specific sources of the auditory N19-P30-P50 response detected by a multiple source analysis of evoked magnetic fields and potentials. In: Williamson SJ, Hoke M, Stroink G, Kotani M, editors. Advances in biomagnetism. Plenum; 1989. p. 97–100.
Mosher JC, Spencer ME, Leahy RM, Lewis PS. Error bounds for EEG and MEG dipole source localization. Electroencephalogr Clin Neurophysiol. 1993;86:303–21. https://doi.org/10.1016/0013-4694(93)90043-U.
Van Veen BD, Van Drongelen W, Yuchtman M, Suzuki A. Localization of brain electrical activity via linearly constrained minimum variance spatial filtering. IEEE Trans Biomed Eng. 1997;44:867–80. https://doi.org/10.1109/10.623056.
Shibata S, Matsuhashi M, Kunieda T, Yamao Y, Inano R, Kikuchi T, Imamura H, Takaya S, Matsumoto R, Ikeda A, Takahashi R, Mima T, Fukuyama H, Mikuni N, Miyamoto S. Magnetoencephalography with temporal spread imaging to visualize propagation of epileptic activity. Clin Neurophysiol. 2017;128:734–43. https://doi.org/10.1016/j.clinph.2017.01.010.
Wilenius J, Lauronen L, Kirveskari E, Gaily E, Metsähonkala L, Paetau R. Interictal magnetoencephalography in parietal lobe epilepsy – comparison of equivalent current dipole and beamformer (SAMepi) analysis. Clin Neurophysiol Pract. 2020;5:64–72. https://doi.org/10.1016/j.cnp.2020.02.003.
Li R, Plummer C, Vogrin SJ, Woods WP, Kuhlmann L, Boston RC, Liley DT, Cook MJ, Grayden DB. Interictal spike localization for epilepsy surgery using magnetoencephalography beamforming. Clin Neurophysiol. 2021;132:928–37. https://doi.org/10.1016/j.clinph.2020.12.019.
Tamilia E, Matarrese MAG, Ntolkeras G, Grant PE, Madsen JR, Stuffle-beam SM, Pearl PL, Papadelis C. Noninvasive mapping of ripple onset predicts outcome in epilepsy surgery. Ann Neurol. 2021;89:911–25. https://doi.org/10.1002/ana.26066.
Sidler E, Greiner H, Mangano FT, Skoch J, Arya R, Holland K, Aun-garoon G, Arthur TM, Fujiwara H, Horn PS, Tenney JR. Improving detection of hippocampal epileptiform activity using magnetoencephalography. J Clin Neurophysiol. 2022;39:240–6. https://doi.org/10.1097/WNP.0000000000000822.
Velmurugan J, Badier JM, Pizzo F, Medina Villalon S, Papageorgakis C, Lopez-Madrona V, Jegou A, Carron R, Bartolomei F, Benar CG. Virtual MEG sensors based on beamformer and independent component analysis can reconstruct epileptic activity as measured on simultaneous intracerebral recordings. Neuroimage. 2022;264:119681. https://doi.org/10.1016/j.neuroimage.2022.119681. This study and citation 67 report the results of simultaneous MEG and SEEG, which allows rare direct correlation between these modalities. Beamformer analysis of MEG allowed localization of hippocampal spikes, which is the subject of controversy.
Coelli S, Medina Villalon S, Bonini F, Velmurugan J, Lopez-Madrona VJ, Carron R, Bartolomei F, Badier JM, B’enar CG. Comparison of beamformer and ICA for dynamic connectivity analysis: a simultaneous MEG-SEEG study. Neuroimage. 2023;265:119806. https://doi.org/10.1016/j.neuroimage.2022.119806.
Luria G, Duran D, Visani E, Rossi Sebastiano D, Sorrentino A, Tassi L, Granvillano A, Franceschetti S, Panzica F. Towards the automatic localization of the irritative zone through magnetic source imaging. Brain Topogr. 2020;33:651–63. https://doi.org/10.1007/s10548-020-00789-y.
Auno S, Lauronen L, Wilenius J, Peltola M, Vanhatalo S, Palva JM. Detrended fluctuation analysis in the presurgical evaluation of parietal lobe epilepsy patients. Clin Neurophysiol. 2021;132:1515–25. https://doi.org/10.1016/j.clinph.2021.03.041.
Jiang X, Ye S, Sohrabpour A, Bagić AI, He B. Imaging the extent and location of spatiotemporally distributed epileptiform sources from MEG measurements. NeuroImage Clin. 2022;33:102903. https://doi.org/10.1016/j.nicl.2021.102903. The authors employ the FAST-IRES algorithm to define the spatial extent of the source of epileptiform discharges. This addresses a significant problem with the standard ECD analysis, which models epileptiform discharges via a point source, which is known to be non-physiologic.
Fujita Y, Yanagisawa T, Fukuma R, Ura N, Oshino S, Kishima H. Abnormal phase-amplitude coupling characterizes the interictal state in epilepsy. J Neural Eng. 2022;19:026056. https://doi.org/10.1088/1741-2552/ac64c4.
Edakawa K, Yanagisawa T, Kishima H, Fukuma R, Oshino S, Khoo HM, Kobayashi M, Tanaka M, Yoshimine T. Detection of epileptic seizures using phase-amplitude coupling in intracranial electroencephalography. Sci Rep. 2016;6:1–8. https://doi.org/10.1038/srep25422.
Bartolomei F, Chauvel P, Wendling F, Timone D, Clinique SDN, Saint-pierre R. Epileptogenicity of brain structures in human temporal lobe epilepsy: a quantified study from intracerebral EEG. Brain. 2008;131:1818–30. https://doi.org/10.1093/brain/awn111.
Michalak AJ, Greenblatt A, Wu S, Tobochnik S, Dave H, Raghupathi R, Esengul YT, Guerra A, Tao JX, Issa NP, Cosgrove GR, Lega B, Warnke P, Chen HI, Lucas T, Sheth SA, Banks GP, Kwon CS, Feldstein N, Youngerman BE, McKhann GM, Davis KA, Schevon CA. Seizure on- set patterns predict outcome after stereo-electroencephalography-guided laser amygdalohippocampotomy. Epilepsia. 2023;64:1568–81. https://doi.org/10.1111/epi.17602.
Staba RJ. Normal and pathological high-frequency oscillations. Jasper’s basic mech. epilepsies. Ed. by Noebels JL, Avoli M, Rogawski MA, Olsen RW, and Delgado-Escueta AV. 4th ed. Oxford University Press, 2012. Chap. 16:202–12
Frauscher B, von Ellenrieder N, Zelmann R, Rogers C, Nguyen DK, Ka-hane P, Dubeau F, Gotman J. High-frequency oscillations in the normal human brain. Ann Neurol. 2018;84:374–85. https://doi.org/10.1002/ana.25304.
Chrobak JJ, Buzsaki G. High-frequency oscillations in the output networks of the hippocampal-entorhinal axis of the freely behaving rat. J Neurosci. 1996;16:3056–66. https://doi.org/10.1523/jneurosci.16-09-03056.
Bragin A, Mody I, Wilson CL, Engel J. Local generation of fast ripples in epileptic brain. J Neurosci. 2002;22:2012–21. https://doi.org/10.1523/jneurosci.22-05-02012.2002.
Zelmann R, Lina JM, Schulze-Bonhage A, Gotman J, Jacobs J. Scalp EEG is not a blur: it can see high frequency oscillations although their generators are small. Brain Topogr. 2014;27:683–704. https://doi.org/10.1007/s10548-013-0321-y.
Jacobs J, Zijlmans M, Zelmann R, Chatillon CE, Hall JA, Olivier A, Dubeau F, Gotman J. High-frequency electroencephalographic oscillations correlate with outcome of epilepsy surgery. Ann Neurol. 2010;67:209–20. https://doi.org/10.1002/ana.21847.
Jacobs J, Wu JY, Perucca P, Zelmann R, Mader M, Dubeau F, Mathern GW, Schulze-Bonhage A, Gotman J. Removing high-frequency oscillations: a prospective multicenter study on seizure outcome. Neurology. 2018;91:e1040–52. https://doi.org/10.1212/WNL.0000000000006158.
Roehri N, Pizzo F, Lagarde S, Lambert I, Nica A, McGonigal A, Giu-siano B, Bartolomei F, B’enar CG. High-frequency oscillations are not better biomarkers of epileptogenic tissues than spikes. Ann Neurol. 2018;83:84–97. https://doi.org/10.1002/ana.25124.
Schevon CA, Trevelyan AJ, Schroeder CE, Goodman RR, McKhann G, Emerson RG. Spatial characterization of interictal high frequency oscillations in epileptic neocortex. Brain. 2009;132:3047–59. https://doi.org/10.1093/brain/awp222.
Velmurugan J, Nagarajan SS, Mariyappa N, Kandavel GR, Ravindranadh T, Kenchaiah CM, Rose R, Bharath D, Saini J, Arivazhagan A, Rajan J, Mahadevan A, Rao MB, Satishchandra P, Sinha S. Magnetoencephalographic imaging of ictal high-frequency oscillations (80–200 Hz) in pharmacologically resistant focal epilepsy. Epilepsia. 2018;59:190–202. https://doi.org/10.1111/epi.13940.
Nissen IA, van Klink NE, Zijlmans M, Stam CJ, Hillebrand A. Brain areas with epileptic high frequency oscillations are functionally isolated in MEG virtual electrode networks. Clin Neurophysiol. 2016;127:2581–91. https://doi.org/10.1016/j.clinph.2016.04.013.
Papadelis C, Tamilia E, Stufflebeam SM, Grant PE, Madsen JR, Pearl PL, Tanaka N. Interictal high frequency oscillations detected with simultaneous magnetoencephalography and electroencephalography as biomarker of pediatric epilepsy. J Vis Exp. 2016;2016:1–13. https://doi.org/10.3791/54883.
van Klink N, Hillebrand A, Zijlmans M. Identification of epileptic high frequency oscillations in the time domain by using MEG beamformer-based virtual sensors. Clin Neurophysiol. 2016;127:197–208. https://doi.org/10.1016/j.clinph.2015.06.008.
Velmurugan J, Nagarajan SS, Mariyappa N, Mundlamuri RC, Raghaven-dra K, Bharath RD, Saini J, Arivazhagan A, Rajeswaran J, Mahadevan A, Malla BR, Satishchandra P, Sinha S. Magnetoencephalography imaging of high frequency oscillations strengthens presurgical localization and outcome prediction. Brain. 2019;142:3514–29. https://doi.org/10.1093/brain/awz284.
Tamilia E, Dirodi M, Alhilani M, Grant PE, Madsen JR, Stufflebeam SM, Pearl PL, Papadelis C. Scalp ripples as prognostic biomarkers of epileptogenicity in pediatric surgery. Ann Clin Transl Neurol. 2020;7:329–42. https://doi.org/10.1002/acn3.50994.
Xiang J, Maue E, Tong H, Mangano FT, Greiner H, Tenney JR. Neuromagnetic high frequency spikes are a new and noninvasive biomarker for localization of epileptogenic zones. Seizure. 2021;89:30–7. https://doi.org/10.1016/j.seizure.2021.04.024.
Xiang J, Maue E, Fujiwara H, Mangano FT, Greiner H, Tenney JR. Delineation of epileptogenic zones with high frequency magnetic source imaging based on kurtosis and skewness. Epilepsy Res. 2021;172:1–10. https://doi.org/10.1016/j.eplepsyres.2021.106602.
Shi LJ, Li CC, Lin YC, Ding CT, Wang YP, Zhang JC. The association of magnetoencephalography high-frequency oscillations with epilepsy types and a ripple-based method with source-level connectivity for mapping epilepsy sources. CNS Neurosci Ther. 2023;29:1423–33. https://doi.org/10.1111/cns.14115.
Vasilica AM, Litvak V, Cao C, Walker M, Vivekananda U. Detection of pathological high-frequency oscillations in refractory epilepsy patients undergoing simultaneous stereo-electroencephalography and magnetoen- cephalography. Seizure. 2023;107:81–90. https://doi.org/10.1016/j.seizure.2023.03.015.
von Ellenrieder N, Pellegrino G, Hedrich T, Gotman J, Lina JM, Grova C, Kobayashi E. Detection and magnetic source imaging of fast oscillations (40–160 Hz) recorded with magnetoencephalography in focal epilepsy patients. Brain Topogr. 2016;29:218–31. https://doi.org/10.1007/s10548-016-0471-9.
van Klink NEC, van Rosmalen F, Nenonen J, Burnos S, Helle L, Taulu S, Furlong PL, Zijlmans M, Hillebrand A. Automatic detection and visualisation of MEG ripple oscillations in epilepsy. NeuroImage Clin. 2017;15:689–701. https://doi.org/10.1016/j.nicl.2017.06.024.
Dirodi M, Tamilia E, Grant PE, Madsen JR, Stufflebeam SM, Pearl PL, and Papadelis C. Noninvasive localization of high-frequency oscillations in children with epilepsy: validation against intracranial gold-standard. Proc Annu Int Conf IEEE Eng Med Biol Soc EMBS 2019 :1555–8. https://doi.org/10.1109/EMBC.2019.8857793
Meng L. A Magnetoencephalography study of pediatric interictal neuromagnetic activity changes and brain network alterations caused by epilepsy in the high frequency (80–1000 Hz). IEEE Trans Neural Syst Rehabil Eng. 2019;27:389–99. https://doi.org/10.1109/TNSRE.2019.2898683.
Foley E, Quitadamo LR, Walsh AR, Bill P, Hillebrand A, Seri S. MEG detection of high frequency oscillations and intracranial-EEG vali- dation in pediatric epilepsy surgery. Clin Neurophysiol. 2021;132:2136–45. https://doi.org/10.1016/j.clinph.2021.06.005.
van Klink NEC, Zijlmans M. High frequency oscillations in MEG: next steps in source imaging for focal epilepsy. Brain. 2019;142:3318–20. https://doi.org/10.1093/brain/awz318.
Yin C, Zhang X, Chen Z, Li X, Wu S, Lv P, Wang Y. Detection and localization of interictal ripples with magnetoencephalography in the presurgical evaluation of drug-resistant insular epilepsy. Brain Res. 2019;1706:147–56. https://doi.org/10.1016/j.brainres.2018.11.006.
Reis J, Rosenow F. Chap. 95: Eloquent cortex and tracts: overview and noninvasive evaluation methods. In: Lüders HO, editor. Textbook of epilepsy surgery. 2008. p. 871–80.
Kreidenhuber R, De Tiège X, Rampp S. Presurgical functional cortical mapping using electromagnetic source imaging. Front Neurol. 2019;10:1–14. https://doi.org/10.3389/fneur.2019.00628.
Papanicolaou AC, Rezaie R, Narayana S, Choudhri AF, Boop FA, Wheless JW. On the relative merits of invasive and non-invasive pre-surgical brain mapping: new tools in ablative epilepsy surgery. Epilepsy Res. 2018;142:153–5. https://doi.org/10.1016/j.eplepsyres.2017.07.002.
Binder JR, Sabsevitz DS, Swanson SJ, Hammeke TA, Raghavan M, Mueller WM. Use of preoperative functional MRI to predict verbal memory decline after temporal lobe epilepsy surgery. Epilepsia. 2008;49:1377–94. https://doi.org/10.1111/j.1528-1167.2008.01625.x.
Sanai N, Mirzadeh Z, Berger MS. Functional outcome after language mapping for glioma resection. N Engl J Med. 2008;358:18–27. https://doi.org/10.1056/nejmoa067819.
Loddenkemper T, Morris HH, Möddel G. Complications during the Wada test. Epilepsy Behav. 2008;13:551–3. https://doi.org/10.1016/j.yebeh.2008.05.014.
Tandon N, Tong BA, Friedman ER, Johnson JA, Von Allmen G, Thomas MS, Hope OA, Kalamangalam GP, Slater JD, Thompson SA. Analysis of morbidity and outcomes associated with use of subdural grids vs stereoelectroencephalography in patients with intractable epilepsy. JAMA Neurol. 2019;76:672–81. https://doi.org/10.1001/jamaneurol.2019.0098.
Stippich C. Presurgical functional MRI and diffusion tensor imaging. Clin. funct. MRI presurical funct. neuroimaging. Ed. by Stippich C. 3rd ed. Springer, 2022. Chap. 1:1–20
Chougar L, Leclercq D, Van de Moortele PF, and Lehericy S. Presurgical functional localization possibilities limitations, and validity. Clin. funct. MRI presurical funct. neuroimaging. Ed. by Stippich C. 3rd ed. Springer, 2022. Chap. 9:343–72
Sporns O. Contributions and challenges for network models in cognitive neuroscience. Nat Neurosci. 2014;17:652–60. https://doi.org/10.1038/nn.3690.
Bagić AI, Bowyer SM, Kirsch HE, Funke ME, Burgess RC. American clinical MEG society (ACMEGS) position statement #2: the value of magnetoencephalography (MEG)/magnetic source imaging (MSI) in noninvasive presurgical mapping of eloquent cortices of patients preparing for surgical interventions. J Clin Neurophysiol. 2017;34:189–95. https://doi.org/10.1097/WNP.0000000000000366.
Youssofzadeh V, Stout J, Ustine C, Gross WL, Conant LL, Humphries CJ, Binder JR, Raghavan M. Mapping language from MEG beta power modulations during auditory and visual naming. Neuroimage. 2020;220: 117090. https://doi.org/10.1016/j.neuroimage.2020.117090.
Herfurth K, Harpaz Y, Roesch J, Mueller N, Walther K, Kaltenhaeuser M, Pauli E, Goldstein A, Hamer HM, Buchfelder M, Doerfler A, Prell J, Rampp S. Localization of beta power decrease as measure for lateralization in pre-surgical language mapping with magnetoencephalography, compared with functional magnetic resonance imaging and validated by Wada test. Front Hum Neurosci. 2022;16:1–21. https://doi.org/10.3389/fnhum.2022.996989.
Babajani-Feremi A, Pourmotabbed H, Schraegle WA, Calley CS, Clarke DF, Papanicolaou AC. MEG language mapping using a novel automatic ECD algorithm in comparison with MNE, dSPM, and DICS beamformer. Front Neurosci. 2023;17:1–17. https://doi.org/10.3389/fnins.2023.1151885.
Foley E, Wood AG, Furlong PL, Walsh AR, Kearney S, Bill P, Hillebrand A, Seri S. Mapping language networks and their association with verbal abilities in paediatric epilepsy using MEG and graph analysis. NeuroImage Clin. 2020;27: 102265. https://doi.org/10.1016/j.nicl.2020.102265.
Tierney TM, Holmes N, Mellor S, Lopez JD, Roberts G, Hill RM, Boto E, Leggett J, Shah V, Brookes MJ, Bowtell R, Barnes GR. Optically pumped magnetometers: from quantum origins to multi-channel magne- toencephalography. Neuroimage. 2019;199:598–608. https://doi.org/10.1016/j.neuroimage.2019.05.063.
Feys O, Corvilain P, Van Hecke A, Sculier C, Rikir E, Legros B, Gaspard N, Leurquin-Sterk G, Holmes N, Brookes MJ, Goldman S, Wens V, De Tiège X. Recording of ictal epileptic activity using on-scalp magnetoencephalography. Ann Neurol. 2022;93:419–21. https://doi.org/10.1002/ana.26562.
Alem O, Hughes KJ, Buard I, Cheung TP, Maydew T, Griesshammer A, Holloway K, Park A, Lechuga V, Coolidge C, Gerginov M, Quigg E, Seames A, Kronberg E, Teale P, Knappe S. An integrated full-head OPM-MEG system based on 128 zero-field sensors. Front Neurosci. 2023;17:1–8. https://doi.org/10.3389/fnins.2023.1190310. One of the first reports of a high-density whole-head OPM MEG system.
Hillebrand A, Holmes N, Sijsma N, Neill GCO, Tierney TM, Liberton N, Stam AH, van Klink N, Stam CJ, Bowtell R, Brookes MJ, Barnes GR. Non-invasive measurements of ictal and interictal epileptiform activity using optically pumped magnetometers. Nat Sci Reports. 2023;13:1–15. https://doi.org/10.1038/s41598-023-31111-y.
Tierney TM, Levy A, Barry DN, Meyer SS, Shigihara Y, Everatt M, Mel-lor S, Lopez JD, Bestmann S, Holmes N, Roberts G, Hill RM, Boto E, Leggett J, Shah V, Brookes MJ, Bowtell R, Maguire EA, Barnes GR. Mouth magnetoencephalography: a unique perspective on the human hippocampus. Neuroimage. 2021;225:117443. https://doi.org/10.1016/j.neuroimage.2020.117443.
Kramer D. Helium is again in short supply. Phys Today. 2022. https://doi.org/10.1063/PT.6.2.20220404a.
Kramer D. Helium prices surge to record levels as shortage continues. Phys Today. 2023;76:18–20. https://doi.org/10.1063/pt.3.5305.
Author information
Authors and Affiliations
Contributions
ASG, PT, and JSE wrote the manuscript. All authors reviewed its content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics Approval
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geller, A.S., Teale, P., Kronberg, E. et al. Magnetoencephalography for Epilepsy Presurgical Evaluation. Curr Neurol Neurosci Rep 24, 35–46 (2024). https://doi.org/10.1007/s11910-023-01328-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-023-01328-5