Abstract
Purpose of Review
The proposed expert opinion was prepared by a panel of obesity and law specialists from Turkey to review the utility of telemedicine in obesity care and to provide a guidance document with recommendations on a hybrid multidisciplinary integrated care follow-up algorithm and the legislation governing telemedicine practice to assist obesity specialists in practicing the telemedicine.
Recent Findings
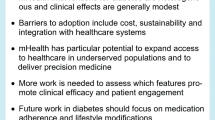
The efficacy and feasibility of telemedicine interventions in supporting obesity management programs even during pandemics confirm that obesity is a particularly well-suited field for telemedicine, emphasizing the strong likelihood of continued utilization of telemedicine in obesity management, beyond the pandemic period.
Summary
Telemedicine has great potential to address several barriers to ongoing weight-management care, such as challenges of access to specialized care, cost, and time limitations as well as patient adherence to treatment. However, telemedicine practice should complement rather than replace the in-person visits which are unique in building rapport and offering social support. Accordingly, the participating experts recommend the use of a hybrid integrated care model in the management of obesity, with the use of telemedicine, as an adjunct to in-person visits, to enable the provision of suggested intensive obesity management via frequent visits by a multidisciplinary team of obesity specialists. Further research addressing the utility of telemedicine in terms of optimal modality and duration for successful long-term obesity management outcomes is necessary to develop specific guidelines on telemedicine practice. In addition, the legislation governing the norms and protocols on confidentiality, privacy, access, and liability needs to be improved.

Similar content being viewed by others
Data Availability
The data supporting the findings of this study are available within the article, further inquiries can be directed to the corresponding author.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
De Lorenzo A, Gratteri S, Gualtieri P, Cammarano A, Bertucci P, Di Renzo L. Why primary obesity is a disease? J Transl Med. 2019;17:169. https://doi.org/10.1186/s12967-019-1919-y.
World Health Organization (WHO). European regional obesity report. Obesity and overweight. Key facts. 2022. https://apps.who.int/iris/bitstream/handle/10665/353747/9789289057738eng.pdf. Accessed 20 Jan 2023.
Dai H, Alsalhe TA, Chalghaf N, Riccò M, Bragazzi NL, Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: an analysis of the Global Burden of Disease Study. PloS Med. 2020;17:e1003198. https://doi.org/10.1371/journal.pmed.1003198.
GBD 2015 Obesity Collaborators; Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27. https://doi.org/10.1056/NEJMoa1614362.
World Health Organization (WHO). Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva, Switzerland: WHO; 2013.
Satman I, Yilmaz T, Sengul A, Salman S, Salman F, Uygur S, et al. Population-based study of diabetes and risk characteristics in Turkey: results of the Turkish diabetes epidemiology study (TURDEP). Diabetes Care. 2002;25:1551–6. https://doi.org/10.2337/diacare.25.9.1551.
Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, et al. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28:169–80. https://doi.org/10.1007/s10654-013-9771-5.
Sonmez A, Yumuk V, Haymana C, Demirci I, Barcin C, Kıyıcı S, et al. Impact of obesity on the metabolic control of type 2 diabetes: results of the Turkish nationwide survey of glycemic and other metabolic parameters of patients with diabetes mellitus (TEMD obesity study). Obes Facts. 2019;12:167–78. https://doi.org/10.1159/000496624.
World Obesity Atlas 2023. https://www.worldobesity.org/resources/resource-library/.
IDF Atlas 10th Edition 2021. https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf.
Ryan DH. Guidelines for obesity management. Endocrinol Metab Clin North Am. 2016;45:501–10. https://doi.org/10.1016/j.ecl.2016.04.003.
Bray GA, Heisel WE, Afshin A, Jensen MD, Dietz WH, Long M, et al. The science of obesity management: an Endocrine Society scientific statement. Endocr Rev. 2018;39:79–132. https://doi.org/10.1210/er.2017-00253.
Kahan S, Look M, Fitch A. The benefit of telemedicine in obesity care. Obesity (Silver Spring). 2022;30:577–86. https://doi.org/10.1002/oby.23382.
Bradley LE, Smith-Mason CE, Corsica JA, Kelly MC, Hood MM. Remotely delivered interventions for obesity treatment. Curr Obes Rep. 2019;8:354–62. https://doi.org/10.1007/s13679-019-00356-y.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376:254–66. https://doi.org/10.1056/NEJMra1514009.
Cueto V, Sanders LM. Telehealth opportunities and challenges for managing pediatric obesity. Pediatr Clin North Am. 2020;67:647–54. https://doi.org/10.1016/j.pcl.2020.04.007.
World Health Organization (WHO). Telemedicine: opportunities and developments in member states. Global Observatory for eHealth series. WHO. 2010. https://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed 15 Jan 2023.
Bodulovic G, Morpurgo M, Saunders EJ. Telehealth around the world: a global guide, DLA Piper Publications. 2020. https://www.dlapiper.com/en/italy/insights/publications/2020/11/telehealth-around-the-world-global-guide/. Accessed 15 Jan 2023.
Clark PA, Capuzzi K, Harrison J. Telemedicine: medical, legal and ethical perspectives. Med Sci Monit. 2010;16:RA261–72.
Patel ML, Wakayama LN, Bennett GG. Self-monitoring via digital health in weight loss interventions: a systematic review among adults with overweight or obesity. Obesity (Silver Spring). 2021;29:478–99. https://doi.org/10.1002/oby.23088.
Vandelanotte C, Müller AM, Short CE, Hingle M, Nathan N, Williams SL, et al. Past, present, and future of eHealth and mHealth research to improve physical activity and dietary behaviors. J Nutr Educ Behav. 2016;48:219–28.e1. https://doi.org/10.1016/j.jneb.2015.12.006.
Hutchesson MJ, Gough C, Müller AM, Short CE, Whatnall MC, Ahmed M, et al. eHealth interventions targeting nutrition, physical activity, sedentary behavior, or obesity in adults: a scoping review of systematic reviews. Obes Rev. 2021;22:e13295. https://doi.org/10.1111/obr.13295.
Patel ML, Wakayama LN, Bass MB, Breland JY. Motivational interviewing in eHealth and telehealth interventions for weight loss: a systematic review. Prev Med. 2019;126:105738. https://doi.org/10.1016/j.ypmed.2019.05.026.
Horne M, Hill A, Murells T, Ugail H, Irving, Chinnadorai R, et al. Using avatars in weight management settings: a systematic review. Internet Interv. 2019;19:100295. https://doi.org/10.1016/j.invent.2019.100295.
Burguera B, Pantalone KM, Griebeler ML, Lansang MC, Rao P, Kashyap S, et al. The need and benefit of implementing telemedicine in clinical practice. Endocr Pract. 2020;26:794–6. https://doi.org/10.4158/EP-2020-0205.
Runfola M, Fantola G, Pintus S, Iafrancesco M, Moroni R. Telemedicine implementation on a bariatric outpatient clinic during COVID-19 pandemic in Italy: an unexpected hill-start. Obes Surg. 2020;30:5145–9. https://doi.org/10.1007/s11695-020-05007-z.
Lewis E, Huang HC, Hassmén P, Welvaert M, Pumpa KL. Adding telephone and text support to an obesity management program improves behavioral adherence and clinical outcomes. A randomized controlled crossover trial. Int J Behav Med. 2019;26:580–90. https://doi.org/10.1007/s12529-019-09815-1.
Ufholz K, Bhargava D. A review of telemedicine interventions for weight loss. Curr Cardiovasc Risk Rep. 2021;15:17. https://doi.org/10.1007/s12170-021-00680-w.
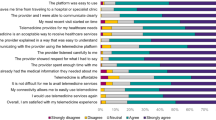
Dario C, Luisotto E, Dal Pozzo E, Mancin S, Aletras V, Newman S, et al. Assessment of patients’ perception of telemedicine services using the service user technology acceptability questionnaire. Int J Integr Care. 2016;16:13. https://doi.org/10.5334/ijic.2219.
Telemedicine practice guidelines enabling registered medical practitioners to provide healthcare using telemedicine. 2020. https://www.mohfw.gov.in/pdf/Telemedicine.pdf. Accessed 20 Jan 2023.
Patient Centered Outcomes Research Institute. Changes to telehealth policy, delivery, and outcomes in response to COVID-19 2020. 2021. https://www.pcori.org/document/changes-telehealth-policy-delivery-and-outcomesresponse-covid-19-landscape-review. Accessed 20 Jan 2023.
Miller EA. Solving the disjuncture between research and practice: telehealth trends in the 21st century. Health Policy. 2007;82:133–41. https://doi.org/10.1016/j.healthpol.2006.09.011.
State Medical Boards’ Appropriate Regulation of Telemedicine (SMART) Workgroup Model policy for the appropriate use of telemedicine technologies in the practice of medicine. 2014. https://www.fsmb.org/siteassets/advocacy/policies/fsmb_telemedicine_policy.pdf. Accessed 20 Jan 2023.
O’Hara VM, Johnston SV, Browne NT. The paediatric weight management office visit via telemedicine: pre- to post-COVID-19 pandemic. Pediatr Obes. 2020;15:e12694. https://doi.org/10.1111/ijpo.12694.
European Commission. Third European Union Health Programme. Market Study on Telemedicine. 2018. https://ec.europa.eu/health/system/files/2019-08/2018_provision_marketstudy_telemedicine_en_0.pdf. Accessed 20 Jan 2023.
Koonin LM, Hoots B, Tsang CA, Leroy Z, Farris K, Jolly T, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic - United States, January-March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1595 –9. https://doi.org/10.15585/mmwr.mm6943a3.
Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;27:1132–5. https://doi.org/10.1093/jamia/ocaa072.
Gelburd R. Telehealth claim lines increase in October 2020 as COVID-19 pandemic surges. AJMC. 2021. https://www.ajmc.com/view/telehealth-claim-lines-increase-inoctober-2020-as-covid-19-pandemic-surges. Accessed 20 Jan 2023.
Sahin E, Kefeli U, Cabuk D, Ozden E, Cakmak Y, Kaypak MA, et al. Perceptions and acceptance of telemedicine among medical oncologists before and during the COVID-19 pandemic in Turkey. Support Care Cancer. 2021;29:7497–503. https://doi.org/10.1007/s00520-021-06290-x.
Brown JD, Hales S, Evans TE, Turner T, Sword DO, O’Neil PM, et al. Description, utilisation and results from a telehealth primary care weight management intervention for adults with obesity in South Carolina. J Telemed Telecare. 2020;26:28–35. https://doi.org/10.1177/1357633X18789562.
Alencar M, Johnson K, Gray V, Mullur R, Gutierrez E, Dionico P. Telehealth-based health coaching increases m-Health device adherence and rate of weight loss in obese participants. Telemed J E Health. 2020;26:365–8. https://doi.org/10.1089/tmj.2019.0017.
Huang JW, Lin YY, Wu NY. The effectiveness of telemedicine on body mass index: a systematic review and meta-analysis. J Telemed Telecare. 2019;25:389–401. https://doi.org/10.1177/1357633X18775564.
Cavero-Redondo I, Martinez-Vizcaino V, Fernandez-Rodriguez R, Saz-Lara A, Pascual-Morena C, Álvarez-Bueno C. Effect of behavioral weight management interventions using lifestyle mhealth self-monitoring on weight loss: a systematic review and meta-analysis. Nutrients. 2020;12:1977. https://doi.org/10.3390/nu12071977.
Carrello J, Hayes A, Baur LA, Lung T. Potential cost-effectiveness of e-health interventions for treating overweight and obesity in Australian adolescents. Pediatr Obes. 2023;18:e13003. https://doi.org/10.1111/ijpo.13003.
Vlahu-Gjorgievska E, Burazor A, Win KT, Trajkovik V. mHealth apps targeting obesity and overweight in young people: app review and analysis. JMIR Mhealth Uhealth. 2023;11:e37716. https://doi.org/10.2196/37716.
• Marsden AM, Hann M, Barron E, Ross J, Valabhji J, Murray E, et al. Comparison of weight change between face-to-face and digital delivery of the English National Health service diabetes prevention programme: an exploratory non-inferiority study with imputation of plausible weight outcomes. Prev Med Rep. 2023;32:102161. https://doi.org/10.1016/j.pmedr.2023.102161. This exploratory study indicates that enrolment in the digital diabetes prevention programme enables clinically significant reductions in weight which were at least equivalent to weight loss in the face-to-face programme and thus digital services can be just as effective as face-to-face in delivering a population-based approach to the prevention of type 2 diabetes.
Sorgente A, Pietrabissa G, Manzoni GM, Re F, Simpson S, Perona S, et al. Web-based interventions for weight loss or weight loss maintenance in overweight and obese people: a systematic review of systematic reviews. J Med Internet Res. 2017;19: e229. https://doi.org/10.2196/jmir.6972.
Chen JL, Wilkosz ME. Efficacy of technology-based interventions for obesity prevention in adolescents: a systematic review. Adolesc Health Med Ther. 2014;5:159–70. https://doi.org/10.2147/AHMT.S39969.
Nguyen B, Kornman KP, Baur LA. A review of electronic interventions for prevention and treatment of overweight and obesity in young people. Obes Rev. 2011;12:e298–314. https://doi.org/10.1111/j.1467-789X.2010.00830.x.
Baulch J, Chester A, Brennan L. Adolescent and parent content preferences and predictors of intention to use an online healthy weight website for adolescents. J Appl Psychol. 2010;6:18–26. https://doi.org/10.7790/ejap.v6i1.173.
Sousa P, Duarte E, Ferreira R, Esperança A, Frontini R, Santos-Rocha R, et al. An mHealth intervention programme to promote healthy behaviours and prevent adolescent obesity (TeenPower): a study protocol. J Adv Nurs. 2019;75:683–91. https://doi.org/10.1111/jan.13905.
Bennett GG, Foley P, Levine E, Whiteley J, Askew S, Steinberg DM, et al. Behavioral treatment for weight gain prevention among black women in primary care practice: a randomized clinical trial. JAMA Intern Med. 2013;173:1770–7. https://doi.org/10.1001/jamainternmed.2013.9263.
Liou TH, Chen CH, Hsu CY, Chou P, Chiu HW. A pilot study of videoconferencing for an Internet-based weight loss programme for obese adults in Taiwan. J Telemed Telecare. 2006;12:370–3. https://doi.org/10.1258/135763306778682350.
Ahrendt AD, Kattelmann KK, Rector TS, Maddox DA. The effectiveness of telemedicine for weight management in the MOVE! Program J Rural Health. 2014;30:113–9. https://doi.org/10.1111/jrh.12049.
Zilliacus E, Meiser B, Lobb E, Dudding TE, Barlow-Stewart K, Tucker K. The virtual consultation: practitioners’ experiences of genetic counseling by videoconferencing in Australia. Telemed J E Health. 2010;16:350–7. https://doi.org/10.1089/tmj.2009.0108.
Armfield NR, Bradford M, Bradford NK. The clinical use of Skype—for which patients, with which problems and in which settings? A snapshot review of the literature. Int J Med Inform. 2015;84:737–42. https://doi.org/10.1016/j.ijmedinf.2015.06.006.
Das SK, Brown C, Urban LE, O’Toole J, Gamache MMG, Weerasekara YK, et al. Weight loss in videoconference and in-person iDiet weight loss programs in worksites and community groups. Obesity (Silver Spring). 2017;25:1033–41. https://doi.org/10.1002/oby.21854.
Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365:1959–68. https://doi.org/10.1056/NEJMoa1108660.
Clark DO, Keith N, Weiner M, Xu H. Outcomes of an RCT of videoconference vs. in-person or in-clinic nutrition and exercise in midlife adults with obesity. Obes Sci Pract. 2019;5:111–9. https://doi.org/10.1002/osp4.318.
Shibuya K, Pantalone KM, Burguera B. Virtual shared medical appointments: a novel tool to treat obesity. Endocr Pract. 2018;24:1108–9. https://doi.org/10.4158/1934-2403-24.12.1108.
West DS, Stansbury M, Krukowski RA, Harvey J. Enhancing group-based internet obesity treatment: a pilot RCT comparing video and text-based chat. Obes Sci Pract. 2019;5:513–20. https://doi.org/10.1002/osp4.371.
Johnson KE, Alencar MK, Coakley KE, Swift DL, Cole NH, Mermier CM, et al. Telemedicine-based health coaching is effective for inducing weight loss and improving metabolic markers. Telemed J E Health. 2019;25:85–92. https://doi.org/10.1089/tmj.2018.0002.
Küçük Yetgin M, Bozdoğan SH, Agopyan A, Kavazoğlu İ, Meriç Y, İşeri C, et al. The effects of home based combined exercises with medical nutritional therapy on body composition, physical performance and quality of life in women with obesity. Turkiye Klinikleri J Sports Sci. 2020;12:283–95. https://doi.org/10.5336/sportsci.2020-74526.
Alencar MK, Johnson K, Mullur R, Gray V, Gutierrez E, Korosteleva O. The efficacy of a telemedicine-based weight loss program with video conference health coaching support. J Telemed Telecare. 2019;25:151–7. https://doi.org/10.1177/1357633X17745471.
Ventura Marra M, Lilly CL, Nelson KR, Woofter DR, Malone J. A pilot randomized controlled trial of a telenutrition weight loss intervention in middle-aged and older men with multiple risk factors for cardiovascular disease. Nutrients. 2019;11:229. https://doi.org/10.3390/nu11020229.
Jaén-Extremera J, Afanador-Restrepo DF, Rivas-Campo Y, Gómez-Rodas A, Aibar-Almazán A, Hita-Contreras F, et al. Effectiveness of telemedicine for reducing cardiovascular risk: a systematic review and meta-analysis. J Clin Med. 2023;12:841. https://doi.org/10.3390/jcm12030841.
Sahin I, Haymana C, Demir T, Demirci I, Tasci I, Atmaca A, et al. Clinical characteristics and outcomes of COVID-19 patients with overweight and obesity: Turkish Nationwide Cohort Study (TurCObesity). Exp Clin Endocrinol Diabetes. 2022;130:115–24. https://doi.org/10.1055/a-1552-4449.
Helvaci N, Eyupoglu ND, Karabulut E, Yildiz BO. Prevalence of obesity and its impact on outcome in patients with COVID-19: a systematic review and meta-analysis. Front Endocrinol (Lausanne). 2021;12:598249. https://doi.org/10.3389/fendo.2021.598249.
Yazıcı D, Fersahoğlu MM, Fersahoğlu T, Bulut NE, Çiğiltepe H, Çeler Ö, et al. Status of weight change, lifestyle behaviors, depression, anxiety, and diabetes mellitus in a cohort with obesity during the COVID-19 lockdown: Turk-Com study group. Obes Facts. 2022;15:528–39. https://doi.org/10.1159/000522658.
Almandoz JP, Xie L, Schellinger JN, Mathew MS, Edwards K, Ofori A, et al. Telehealth utilization among multi-ethnic patients with obesity during the COVID-19 pandemic. J Telemed Telecare. 2021;1357633X21998211. https://doi.org/10.1177/1357633X21998211. Epub ahead of print.
Aras M, Tchang BG, Crawford A, Bledsoe M, Fujioka K, Aronne LJ. Impact of telemedicine during the COVID-19 pandemic on patient attendance. Obesity (Silver Spring). 2021;29:1093–4. https://doi.org/10.1002/oby.23180.
Minsky NC, Pachter D, Zacay G, Chishlevitz N, Ben-Hamo M, Weiner D, et al. Managing obesity in lockdown: survey of health behaviors and telemedicine. Nutrients. 2021;13:1359. https://doi.org/10.3390/nu13041359.
Akbas F, Atmaca HU, Piskinpasa ME. An experience of telemedicine during COVID-19 pandemic: follow-up of patients with obesity via phone interviews. Bagcilar Med Bull. 2020;5:199–203. https://doi.org/10.4274/BMB.galenos.2020.08.052.
Ozturk B, Duruturk N. Effect of telerehabilitation applied during COVID-19 isolation period on physical fitness and quality of life in overweight and obese individuals. Int J Obes (Lond). 2022;46:95–9. https://doi.org/10.1038/s41366-021-00965-5.
Bailly S, Fabre O, Legrand R, Pantagis L, Mendelson M, Terrail R, et al. The impact of the COVID-19 lockdown on weight loss and body composition in subjects with overweight and obesity participating in a nationwide weight-loss program: impact of a remote consultation follow-up-the CO-RNPC study. Nutrients. 2021;13:2152. https://doi.org/10.3390/nu13072152.
2020 State of Telemedicine Report. Examining patient perspectives and physician adoption of telemedicine since the COVID-19 pandemic. 2020. https://c8y.doxcdn.com/image/upload/Press%20Blog/Research%20Reports/2020-state-telemedicine-report.pdf. Accessed 20 Jan 2023.
Hlavin C, Ingraham P, Byrd T, Hyre N, Gabriel L, Agrawal N, et al. Clinical outcomes and hospital utilization among patients undergoing bariatric surgery with telemedicine preoperative care. JAMA Netw Open. 2023;6: e2255994. https://doi.org/10.1001/jamanetworkopen.2022.55994.
Daouadji-Ghazouani A, Aron-Wisnewsky J, Torcivia A, Irigoin-Guichandut M, Poitou C, Faucher P, et al. Follow-up, safety, and satisfaction with tele-bariatric follow-up implemented during the COVID-19 French lockdown: a 2-year follow-up study. Obes Surg. 2023;33:1083–91. https://doi.org/10.1007/s11695-023-06485-7.
• Dhaver S, Al-Badri M, Salah T, Kilroy C, Shahar J, Johnson C, et al. Hybrid model of intensive lifestyle intervention is potentially effective in patients with diabetes & obesity for post-COVID era. Front Endocrinol (Lausanne). 2023;13:1050527. https://doi.org/10.3389/fendo.2022.1050527. This study shows that hybrid model of intensive lifestyle intervention is as effective as virtual model and in-person model in reducing body weight and HbA1c after 12 weeks, emphasizing that it can be offered to more patients with diabetes and obesity who may benefit from its increased flexibility and enhanced accountability without compromising the multidisciplinary approach for a post-COVID era.
Fix O, Serper M. Telemedicine and telehepatology during the COVID-19 pandemic. Clin Liver Dis (Hoboken). 2020;15:187–90. https://doi.org/10.1002/cld.971.
Hoyt K, Reynolds A. The patient perspective on telemedicine. Clin Liver Dis (Hoboken). 2022;19:167–70. https://doi.org/10.1002/cld.1188.
Ramaswamy A, Yu M, Drangsholt S, Ng E, Culligan PJ, Schlegel PN, et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22:e20786. https://doi.org/10.2196/20786.
Al-Sofiani ME, Alyusuf EY, Alharthi S, Alguwaihes AM, Al-Khalifah R, Alfadda A. rapid implementation of a diabetes telemedicine clinic during the coronavirus disease 2019 outbreak: our protocol, experience, and satisfaction reports in Saudi Arabia. J Diabetes Sci Technol. 2021;15:329–38. https://doi.org/10.1177/1932296820947094.
Driscoll S, Meyerowitz-Katz G, Ahlenstiel G, Reynolds T, Reid K, Bishay RH. Efficacy of telephone health coaching integration with standard multidisciplinary care for adults with obesity attending a weight management service: a pilot study. Nutrients. 2021;13:4078. https://doi.org/10.3390/nu13114078.
Bughin F, Bui G, Ayoub B, Blervaque L, Saey D, Avignon A, et al. Impact of a mobile telerehabilitation solution on metabolic health outcomes and rehabilitation adherence in patients with obesity: randomized controlled trial. JMIR Mhealth Uhealth. 2021;9:e28242. https://doi.org/10.2196/28242.
Ahmad F, Wysocki RW, Fernandez JJ, Cohen MS, Simcock XC. Patient perspectives on telemedicine during the COVID-19 pandemic. Hand (N Y). 2021;18:522–6. https://doi.org/10.1177/15589447211030692.
Wang-Selfridge AA, Dennis JF. Management of obesity using telemedicine during the COVID-19 pandemic. Mo Med. 2021;118:442–5.
Anton SD, LeBlanc E, Allen HR, Karabetian C, Sacks F, Bray G, et al. Use of a computerized tracking system to monitor and provide feedback on dietary goals for calorie-restricted diets: the POUNDS LOST study. J Diabetes Sci Technol. 2012;6:1216–25. https://doi.org/10.1177/193229681200600527.
Apovian CM, Istfan NW. Obesity: guidelines, best practices, new research. Endocrinol Metab Clin North Am. 2016;45:xvii-xviii. https://doi.org/10.1016/j.ecl.2016.06.014.
Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, et al. European guidelines for obesity management in adults. Obes Facts. 2015;8:402–24. https://doi.org/10.1159/000442721.
Cliffe M, Di Battista E, Bishop S. Can you see me? Participant experience of accessing a weight management programme via group videoconference to overcome barriers to engagement. Health Expect. 2021;24:66–76. https://doi.org/10.1111/hex.13148.
Shannon HH, Joseph R, Puro N, Darrell E. Use of technology in the management of obesity: a literature review. Perspect Health Inf Manag. 2019;16(Fall):1c.
Cohen GM, Irby MB, Boles K, Jordan C, Skelton JA. Telemedicine and pediatric obesity treatment: review of the literature and lessons learned. Clin Obes. 2012;2:103–11. https://doi.org/10.1111/j.1758-8111.2012.00050.x.
Whitley A, Yahia N. Efficacy of clinic-based telehealth vs. face-to-face interventions for obesity treatment in children and adolescents in the United States and Canada: a systematic review. Child Obes. 2021;17:299–310. https://doi.org/10.1089/chi.2020.0347.
Coppock JH, Ridolfi DR, Hayes JF, St Paul M, Wilfley DE. Current approaches to the management of pediatric overweight and obesity. Curr Treat Options Cardiovasc Med. 2014;16:343. https://doi.org/10.1007/s11936-014-0343-0.
Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11years. Cochrane Database Syst Rev. 2017;6:CD012651. https://doi.org/10.1002/14651858.CD012651.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 8. Obesity and weight management for the prevention and treatment of type 2 diabetes: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S128–39. https://doi.org/10.2337/dc23-S008.
Fleischman A, Hourigan SE, Lyon HN, Landry MG, Reynolds J, Steltz SK, et al. Creating an integrated care model for childhood obesity: a randomized pilot study utilizing telehealth in a community primary care setting. Clin Obes. 2016;6:380–8. https://doi.org/10.1111/cob.12166.
Dvorák M, Tóth M, Ács P. The role of individualized exercise prescription in obesity management-case study. Int J Environ Res Public Health. 2021;18:12028. https://doi.org/10.3390/ijerph182212028.
Prost SG, Ai AL, Ainsworth SE, Ayers J. Mental health professionals and behavioral interventions for obesity: a systematic literature review. J Evid Inf Soc Work. 2016;13:305–30. https://doi.org/10.1080/23761407.2015.1031418.
Macpherson-Sánchez AE. Integrating fundamental concepts of obesity and eating disorders: implications for the obesity epidemic. Am J Public Health. 2015;105:e71-85. https://doi.org/10.2105/AJPH.2014.302507.
Unal Ş, Sevinçer GM, Maner AF. Bariatrik Cerrahi Sonrası Kilo Geri Alımının; Gece Yeme, Duygusal Yeme, Yeme Endişesi, Depresyon ve Demografik Özellikler Tarafından Yordanması [Prediction of weight regain after bariatric surgery by night eating, emotional eating, eating concerns, depression and demographic characteristics]. Turk Psikiyatri Derg. 2019;30:31–41. Turkish.
Varkevisser RDM, van Stralen MM, Kroeze W, Ket JCF, Steenhuis IHM. Determinants of weight loss maintenance: a systematic review. Obes Rev. 2019;20:171–211. https://doi.org/10.1111/obr.12772.
Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6:67–85. https://doi.org/10.1111/j.1467-789X.2005.00170.x.
Teixeira PJ, Carraça EV, Marques MM, Rutter H, Oppert JM, De Bourdeaudhuij I, et al Successful behavior change in obesity interventions in adults: a systematic review of self‐regulation mediators. BMC Med. 2015;13:84. https://doi.org/10.1186/s12916-015-0323-6.
Chaet D, Clearfield R, Sabin JE, Skimming K. Ethical practice in telehealth and telemedicine. J Gen Intern Med. 2017;32:1136–40. https://doi.org/10.1007/s11606-017-4082-2.
Fogel AL, Kvedar JC. Reported cases of medical malpractice in direct-to-consumer telemedicine. JAMA. 2019;321:1309–10. https://doi.org/10.1001/jama.2019.0395.
Turkish Ministry of Health. Regulation on the provision of distance health services. 2022. https://www.resmigazete.gov.tr/eskiler/2022/02/20220210-2.htm. Accessed 20 Jan 2023.
Funding
This expert panel study was supported by Novo Nordisk Turkey. Editorial support was provided by KAPPA Consultancy Training Research Ltd., Istanbul, Turkey (supported by Novo Nordisk).
Author information
Authors and Affiliations
Contributions
All authors contributed to the discussion and preparation of the expert opinion and critically revised and approved the manuscript, and the authors take full responsibility for the contents of the article.
Corresponding author
Ethics declarations
Conflict of Interest
Fahri Bayram participated in clinical studies and adboard meetings conducted by Novo Nordisk, Eli Lilly, Abbott, Sanovel, Novartis, Sandoz, Bilim ilaç, Astrazeneca, Pfizer, Ali raif, Econix and Sanofi. Alper Sonmez was involved as the principal investigator in several phase 3 studies conducted by Novo Nordisk, Novartis, Sanofi, participated in adboard meetings performed by Novo Nordisk, Sanofi, AstraZeneca, Eczacıbaşı, Econix, Roche Diagnostics and took grants congress from Bilim Ilaç, Novo Nordisk and AstraZeneca. Volkan Yumuk participated in speakers’ bureaus and advisory board meetings performed by Novo Nordisk. Sinem Kiyici received speaking fees paid to her Institution for Novo Nordisk, Boehringer Ingelheim, AstraZeneca, Servier, Abbott and Novartis. Other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article is a review of the published literature. This review article does not contain any studies performed with human or animal subjects by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bayram, F., Sonmez, A., Kiyici, S. et al. Expert Opinion on the Utility of Telemedicine in Obesity Care: Recommendations on a Hybrid Multidisciplinary Integrated Care Follow-Up Algorithm. Curr Obes Rep 13, 167–182 (2024). https://doi.org/10.1007/s13679-023-00541-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-023-00541-0