Abstract
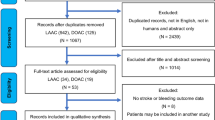
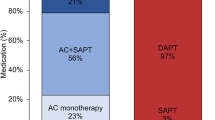
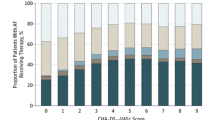
This meta-analysis compared the efficacy and safety of different antithrombotic regimens after left atrial appendage closure (LAAC). PubMed, Embase, Medline, Cochrane Library databases were systematically searched from their inception to March 2023. Patients were divided into short-term oral anticoagulation (OAC) group and antiplatelet therapy (APT) group. The incidence of events were performed using RevMan 5.4. The events including device-related thrombus (DRT), ischemic stroke/systemic embolization (SE), major bleeding, any bleeding, any major adverse event and all-cause mortality. Subgroup analysis were based on OAC alone or OAC plus single antiplatelet therapy (SAPT) in OAC group. Oral anticoagulants include warfarin and direct oral anticoagulant (DOAC). Fourteen studies with 35,166 patients were included. We found that the incidence of DRT (OR = 0.49, 95% CI 0.36–0.66, P<0.0001) and all-cause mortality (OR = 0.71, 95% CI 0.57–0.89, P = 0.002) were significantly lower in OAC group than APT group. However, there was no statistical differences in the incidence rates of ischemic stroke/SE (OR = 0.77, 95% CI 0.49–1.20, P = 0.25), major bleeding (OR = 0.84, 95% CI 0.55–1.27, P = 0.84), any bleeding (OR = 0.83, 95% CI 0.56–1.22, P = 0.34) and any major adverse event (OR = 0.56, 95% CI 0.30–1.03, P = 0.06) in the two groups. Subgroup analysis found that the incidence of DRT, all-cause mortality and any major adverse event in OAC monotherapy were lower than that in APT group (P<0.05), but not statistically different from other outcome. The incidence of DRT, all-cause mortality, any major adverse event and any bleeding in DOAC were significantly better than APT group (P<0.05). While warfarin only has better incidence of DRT than APT (P<0.05), there was no statistical difference between the two groups in other outcome (P>0.05). The incidence of DRT was significantly lower than APT group (P<0.05), major bleeding were higher, and the rest of the outcome did not show any statistically significant differences(P>0.05) when OAC plus SAPT. Based on the existing data, short-term OAC may be favored over APT for patients who undergo LAAC. DOAC monotherapy may be favored over warfarin monotherapy or OAC plus APT, when selecting anticoagulant therapies.




Similar content being viewed by others
Data availability
The authors confirm that all data collected and analyzed for this study are included in the article or its supplementary materials.
References
Hindricks G, Potpara T, Dagres N et al (2021) 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 42(5):373–498
Ogilvie IM, Newton N, Welner Sharon A et al (2010) Underuse of oral anticoagulants in atrial fibrillation: a systematic review. Am J Med 123(7):638–645
Kong B, Liu Y, Huang H et al (2015) Left atrial appendage closure for thromboembolism prevention in patients with atrial fibrillation: advances and perspectives. J Thorac Dis 7(2):199–203
January CT, Wann LS, Calkins H et al (2019) 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS Guideline for the management of patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines and the heart rhythm society in collaboration with the Society of thoracic surgeons. Circulation 140(2):e125–151
Osmancik P, Herman D, Neuzil P et al (2022) 4-Year outcomes after left atrial appendage Closure Versus nonwarfarin oral anticoagulation for Atrial Fibrillation. J Am Coll Cardiol 79(1):1–14
Sedaghat A, Vij V, Al-Kassou B et al (2021) Device-related thrombus after left atrial appendage closure: data on thrombus characteristics, treatment strategies, and clinical outcomes from the EUROC-DRT-Registry. Circulation 14(5):e010195
Chinese society of cardiology of Chinese medical association, editorial board of Chinese journal of cardiology (2019) 2019 Chinese Society of Cardiology (CSC) expert consensus statement on left atrial appendage closure in the prevention of Stroke in patients with atrial fibrillation. Zhonghua Xin xue guan bing za zhi 47(12):937–955
Nogami A, Kurita T, Kusano K et al (2022) JCS/JHRS 2021 Guideline focused update on Non-pharmacotherapy of Cardiac Arrhythmias. Circ J 86(2):337–363
Faroux L, Cruz-González I, Arzamendi D et al (2021) Short-term direct oral anticoagulation or dual antiplatelet therapy following left atrial appendage closure in patients with relative contraindications to chronic anticoagulation therapy. Int J Cardiol 333:77–82
Søndergaard L, Wong YH, Reddy VY et al (2019) Propensity-matched comparison of oral anticoagulation versus antiplatelet therapy after left atrial appendage closure With WATCHMAN. JACC Cardiovasc Interv 12(11):1055–1063
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–34
Higgins JP, Altman DG, Gøtzsche PC et al (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Wells G, Shea B, O’Connell D et al The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Online]. Ottawa Hospital Research Institute Research Programs. Available at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Su F, Gao C, Liu J et al (2022) Periprocedural outcomes Associated with Use of a left atrial appendage occlusion device in China. JAMA Netw Open 5(5):e2214594
Freeman JV, Higgins AY, Wang Y et al (2022) Antithrombotic therapy after left atrial appendage occlusion in patients with Atrial Fibrillation. J Am Coll Cardiol 79(18):1785–1798
Ledwoch J, Staubach S, Akin I et al (2022) Anticoagulation versus antiplatelet therapy after percutaneous left atrial appendage closure-subanalysis from the multicenter LAARGE registry. J Interv Card Electrophysiol 64(2):489–496
Mazzone P, Laricchia A, D’Angelo G et al (2021) Role of Different Antithrombotic Regimens after Percutaneous Left Atrial Appendage Occlusion: A Large Single Center Experience. J Clin Med 10(9):1959
Cepas-Guillen PL, Flores-Umanzor E, Regueiro A et al (2021) Low Dose of Direct Oral Anticoagulants after Left Atrial Appendage Occlusion. J Cardiovasc Dev Dis 8(11):142
Duthoit G, Silvain J, Marijon E et al (2020) Reduced rivaroxaban dose versus dual antiplatelet therapy after left atrial appendage closure: ADRIFT a randomized pilot study. Circulation 13(7):e008481
Asmarats L, O’Hara G, Champagne J et al (2020) Short-term oral anticoagulation versus antiplatelet therapy following transcatheter left atrial appendage closure. Circulation 13(8):e009039
Ledwoch J, Sievert K, Boersma LVA et al (2020) Initial and long-term antithrombotic therapy after left atrial appendage closure with the WATCHMAN. Europace 22(7):1036–1043
Liu XX, Kleinecke C, Busch S et al (2020) Propensity-matched comparison of antiplatelet versus anticoagulant after left atrial appendage closure with the Watchman. Pace 43(11):1242–1251
Bergmann MW, Betts TR, Sievert H et al (2017) Safety and efficacy of early anticoagulation drug regimens after WATCHMAN left atrial appendage closure: three-month data from the EWOLUTION prospective, multicentre, monitored international WATCHMAN LAA closure registry. Eurointervention 13(7):877–884
Tung MK, Ramkumar S, Cameron JD et al (2017) Retrospective cohort study examining reduced intensity and duration of anticoagulant and antiplatelet therapy following left atrial appendage occlusion with the WATCHMAN device. Heart Lung circ 26(5):477–485
Bösche LI, Afshari F, Schöne D et al (2015) Initial experience with novel oral anticoagulants during the First 45 days after left atrial appendage Closure with the Watchman device. Clin Cardiol 38(12):720–724
Wiebe J, Franke J, Lehn K et al (2015) Percutaneous left atrial appendage closure with the watchman device: long-term results up to 5 years. JACC Cardiovasc Interv 8(15):1915–1921
Saw J, Nielsen-Kudsk JE, Bergmann M et al (2019) Antithrombotic therapy and device-related thrombosis following endovascular left atrial appendage closure. JACC Cardiovasc Interv 12(11):1067–1076
Rodés-Cabau J, O’Hara G, Paradis JM et al (2017) Changes in coagulation and platelet activation markers following transcatheter left Atrial Appendage Closure. Am J Cardiol 120(1):87–91
Schwartz RS, Holmes DR, Van Tassel RA et al (2010) Left atrial appendage obliteration: mechanisms of healing and intracardiac integration. JACC Cardiovasc Interv 3(8):870–877
Fauchier L, Cinaud A, Brigadeau F et al (2018) Device-related Thrombosis after percutaneous left atrial appendage occlusion for Atrial Fibrillation. J Am Coll Cardiol 71(14):1528–1536
Holmes DR, Reddy VY, Turi ZG et al (2009) Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of Stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet 374(9689):534–542
Mesnier J, Cepas-Guillén P, Freixa X et al (2023) Antithrombotic management after left atrial appendage closure: current evidence and future perspectives. Circulation 16(5):e012812
Li SY, Wang J, Hui X et al (2020) Meta-analysis of postoperative antithrombotic therapy after left atrial appendage occlusion. J Int Med Res 48(11):300060520966478
Osman M, Busu T, Osman K et al (2020) Short-term antiplatelet versus anticoagulant therapy after left atrial appendage occlusion: a systematic review and meta-analysis. Clin Electrophysiol 6(5):494–506
Prasad RM, Al-Abcha A, Radwan Y et al (2021) Meta-analysis comparing antiplatelet therapy Versus Direct oral anticoagulation in Percutaneous Left Atrial Appendage Closure. Am J Cardiol 153:144–146
Peternel P, Terbizan M, Tratar G et al (2002) Markers of hemostatic system activation during treatment of deep vein Thrombosis with subcutaneous unfractionated or low-molecular weight heparin. Thromb Res 105(3):241–246
Amirtabar A, Vazquez SR, Saunders J et al (2023) Antiplatelet therapy indication in patients also prescribed direct oral anticoagulants. J Thromb Thrombolys 55(1):185–188
Angiolillo DJ, Bhatt DL, Cannon CP et al (2021) Antithrombotic therapy in patients with atrial fibrillation treated with oral anticoagulation undergoing percutaneous coronary intervention: a north American perspective: 2021 update. Circulation 143(6):583–596
Ge H, Zhang C, Qiao ZQ et al (2022) Risk of device-related Thrombosis following short-term oral anticoagulation with low-dose dabigatran versus warfarin after Watchman left atrial appendage occlusion. Sci Prog 105(3):1–14
Li X, Zhang X, Jin Q et al (2021) Clinical efficacy and safety comparison of Rivaroxaban and Dabigatran for Nonvalvular Atrial Fibrillation patients undergoing Percutaneous Left Atrial Appendage Closure Operation. Front Pharmacol 12:614762
Della Rocca DG, Magnocavallo M, Di Biase L et al (2021) Half-dose direct oral anticoagulation versus standard antithrombotic therapy after left atrial appendage occlusion. Cardiovasc Interv 14(21):2353–2364
Della Rocca DG, Horton RP, Di Biase L et al (2021) Incidence of device-related thrombosis in watchman patients undergoing a genotype-guided antithrombotic strategy. Clin Electrophysiol 7(12):1533–1543
Acknowledgements
None.
Funding
This study was supported by the grants from the National Natural Science Foundation of China (61905280, 82104303).
Author information
Authors and Affiliations
Contributions
QZ and XL were involved in the study conception and design. QZ, XL, CZG and XY performed statistical analysis. MW, CZG and ZYW critically revised original study design and the manuscript. QZ, MW, YYT, HXH and XL contributed to the data acquisition, analysis, and interpretation. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interests in this work.
Ethical approval
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, Q., Liu, X., Gu, ZC. et al. Short-term antiplatelet versus anticoagulant therapy after left atrial appendage closure: a systematic review and meta-analysis. J Thromb Thrombolysis 57, 194–203 (2024). https://doi.org/10.1007/s11239-023-02919-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-023-02919-2