Abstract
Introduction
Breast cancer subtypes based on estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) expression have significant implications for prognosis. HER2-positive tumors historically demonstrated poorer survival, but anti-HER2 targeted therapy improved outcomes. However, hormone receptor (HR)-positive patients may experience reduced benefit due to HER2-HR signaling crosstalk.
Methods
Data from two databases, the Shanghai Jiao Tong University Breast Cancer Data Base (SJTUBCDB) and the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) database, were analyzed. Propensity score adjustments were used to balance patient characteristics between ER+/PR+/HER2+ and ER+/PR−/HER2+ subtypes. Kaplan–Meier survival curves estimated disease-free survival (DFS), breast cancer-specific survival (BCSS), overall survival (OS) for these subtypes in the SJTUBCDB, while subgroup analyses using multivariable models were performed based on menstruation, pN stage, HER2-targeted therapy, and endocrinotherapy.
Results
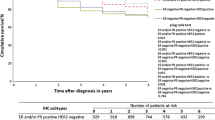
The ER+/PR+/HER2+ group showed significantly better DFS and BCSS than the ER+/PR−/HER2+ group, particularly in postmenopausal and pN0 stage patients. Survival outcomes were similar after anti-HER2 therapy or endocrine aromatase inhibitor (AI) therapy in both groups. However, among patients receiving selective estrogen receptor modulator (SERM) treatment, those in the ER+/PR−/HER2+ group had a significantly worse prognosis compared to ER+/PR+/HER2+ patients.
Conclusions
HER2-positive breast cancers with different HR statuses exhibit distinct clinicopathological features and survival outcomes. Patients in the ER+/PR+/HER2+ group generally experience better survival, particularly in postmenopausal and pN0 stage patients. Treatment strategies should consider HR status and specific modalities for better personalized management.




Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SJTUBCDB:
-
Shanghai Jiao Tong University Breast Cancer Data Base
- SEER:
-
Surveillance, Epidemiology, and End Results
- IPTW:
-
Inverse probability of treatment weighting
- HR:
-
Hormone receptor
- ER:
-
Estrogen-receptor
- PR:
-
Progesterone receptor
- HER2:
-
Human epidermal growth factor receptor-2
- FISH:
-
Fluorescence in situ hybridization
- SISH:
-
Silver in situ hybridization
- IDC:
-
Invasive ductal carcinoma
- ILC:
-
Invasive lobular carcinoma
- BCSS:
-
Breast cancer-specific survival
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
- SEER:
-
Surveillance Epidemiology and End Results
- HRs:
-
Hazard ratios
- CI:
-
Confidence interval
- SERM:
-
Selective estrogen receptor modulator
- AI:
-
Aromatase inhibitor
References
Parise CA, Bauer KR, Brown MM, et al. Breast cancer subtypes as defined by the estrogen receptor (ER), progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2) among women with invasive breast cancer in California, 1999–2004. Breast J. 2009;15(6):593–602.
Cheang MC, Chia SK, Voduc D, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101(10):736–50.
Mendes D, Alves C, Afonso N, et al. The benefit of HER2-targeted therapies on overall survival of patients with metastatic HER2-positive breast cancer—a systematic review. Breast Cancer Res. 2015;17(17):140.
Adusumilli P, Konatam ML, Gundeti S, et al. Treatment challenges and survival analysis of human epidermal growth factor receptor 2-positive breast cancer in real world. Indian J Med Paediatr Oncol. 2017;38(1):22–7.
Sundquist M, Brudin L, Tejler G. Improved survival in metastatic breast cancer 1985–2016. Breast. 2017;31:46–50.
Dawood S, Broglio K, Buzdar AU, et al. Prognosis of women with metastatic breast cancer by HER2 status and trastuzumab treatment: an institutional-based review. J Clin Oncol. 2010;28(1):92–8.
Pogue-Geile KL, Kim C, Jeong JH, et al. Predicting degree of benefit from adjuvant trastuzumab in NSABP trial B-31. J Natl Cancer Inst. 2013;105(23):1782–8.
Howlader N, Altekruse SF, Li CI, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5):055.
National Comprehensive Cancer Network Breast Cancer (version 3.2020). Invasive breast cancer, systemic adjuvant treatment (BINV-4). https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 1 May 2020.
Rakha EA, El-Sayed ME, Green AR, et al. Biologic and clinical characteristics of breast cancer with single hormone receptor positive phenotype. J Clin Oncol. 2007;25(30):4772–8.
Bardou V-J, Arpino G, Elledge RM, et al. Progesterone receptor status significantly improves outcome prediction over estrogen receptor status alone for adjuvant endocrine therapy in two large breast cancer databases. J Clin Oncol. 2003;21(10):1973–9.
Arpino G, Weiss H, Lee AV, Schif R, De Placido S, Osborne CK, Elledge RM. Estrogen receptor-positive, progesterone receptor-negative breast cancer: association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst. 2005;97(17):1254–61.
Cancello G, Maisonneuve P, Rotmensz N, et al. Progesterone receptor loss identifies Luminal B breast cancer subgroups at higher risk of relapse. Ann Oncol. 2013;24(3):661–8.
Prat A, Cheang MC, Martin M, et al. Prognostic significance of progesterone receptor-positive tumor cells within immunohistochemically defined luminal A breast cancer. J Clin Oncol. 2013;31(2):203–9.
Braun L, Mietzsch F, Seibold P, et al. Intrinsic breast cancer subtypes defined by estrogen receptor signalling-prognostic relevance of progesterone receptor loss. Mod Pathol. 2013;26(9):1161–71.
Cui X, Schiff R, Arpino G, et al. Biology of progesterone receptor loss in breast cancer and its implications for endocrine therapy. J Clin Oncol. 2005;23(30):7721–35.
Bae SY, Kim S, Lee JH, et al. Poor prognosis of single hormone receptor–positive breast cancer: similar outcome as triple-negative breast cancer. BMC Cancer. 2015;18(15):138.
Zhao H, Gong Y. The prognosis of single hormone receptor-positive breast cancer stratified by HER2 status. Front Oncol. 2021;17(11): 643956.
Sagara Y, Mallory MA, Wong S, et al. Survival benefit of breast surgery for low-grade ductal carcinoma in situ: a population based cohort study. JAMA Surg. 2015;150(8):739–45.
Sagara Y, Freedman RA, Vaz-Luis I, et al. Patient prognostic score and associations with survival improvement offered by radiotherapy after breast-conserving surgery for ductal carcinoma in situ: a population-based longitudinal cohort study. J Clin Oncol. 2016;34(11):1190–6.
Squires BS, Quinn TJ, Nandalur SR, et al. Adjuvant radiotherapy improves overall survival when added to surgery and chemotherapy for uterine carcinosarcoma: a surveillance, epidemiology, and end results analysis. Int J Clin Oncol. 2021;26(12):2282–94.
Diggs A, Sia TY, Huang Y, et al. Utilization and outcomes of adjuvant therapy for stage II and III uterine leiomyosarcoma. Gynecol Oncol. 2022;166(2):308–16.
Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–64.
Ding NH, Liu CF, Hu C, et al. Prognostic factors for luminal B-like breast cancer. Curr Med Sci. 2019;39(3):396–402.
Colditz GA, Rosner BA, Chen WY, et al. Risk factors for breast cancer according to estrogen and progesterone receptor status. J Natl Cancer Inst. 2004;96(3):218–28.
Schif R, Massarweh SA, Shou J, Bharwani L, Mohsin SK, Osborne CK. Cross-talk between estrogen receptor and growth factor pathways as a molecular target for overcoming endocrine resistance. Clin Cancer Res. 2004;10:331s-s336.
Osborne CK, Shou J, Massarweh S, Schif R. Crosstalk between estrogen receptor and growth factor receptor pathways as a cause for endocrine therapy resistance in breast cancer. Clin Cancer Res. 2005;11:865s-s870.
Zhang Y, Su H, Rahimi M, et al. EGFRvIII-induced estrogen-independence, tamoxifen-resistance phenotype correlates with PgR expression and modulation of apoptotic molecules in breast cancer. Int J Cancer. 2009;125(9):2021–8.
Punglia RS, Kuntz KM, Winer EP, et al. The impact of tumor progesterone receptor status on optimal adjuvant endocrine therapy for postmenopausal patients with early-stage breast cancer: a decision analysis. Cancer. 2006;106(12):2576–82.
Montemurro F, Di Cosimo S, Arpino G. Human epidermal growth factor receptor 2 (HER2)-positive and hormone receptor-positive breast cancer: new insights into molecular interactions and clinical implications. Ann Oncol. 2013;24(11):2715–24.
Lønning PE. Poor-prognosis estrogen receptor-positive disease: present and future clinical solutions. Ther Adv Med Oncol. 2012;4(3):127–37.
Montemurro F, Rossi V, Cossu Rocca M, et al. Hormone-receptor expression and activity of trastuzumab with chemotherapy in HER2-positive advanced breast cancer patients. Cancer. 2012;118(1):17–26.
Kay C, Martínez-Pérez C, Meehan J, et al. Current trends in the treatment of HR+/HER2+ breast cancer. Future Oncol. 2021;17(13):1665–81.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Conception and design: WD, DY, HC, CT. Administrative support: YL, ZL. Collection and assembly of data: WD, YL, ZL. Data analysis and interpretation: WD, DY, HC. Manuscript writing: all authors. Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Our study was approved by the independent ethics committee/institutional review board at Shaoxing Second Hospital Ethical Committee. The data from the SEER datasets are publicly available and therefore do not require informed patient consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Ding, W., Ye, D., Chen, H. et al. Clinicopathological differences and survival benefit in ER+/PR+/HER2+ vs ER+/PR−/HER2+ breast cancer subtypes. Breast Cancer 31, 295–304 (2024). https://doi.org/10.1007/s12282-023-01538-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-023-01538-2