Abstract
Background and Objective
Pregabalin is steadily gaining popularity worldwide, with epidemiological studies indicating an increase in labeled, off-labeled, and recreational uses. In Israel, pregabalin prescriptions are not regulated by the controlled substances legislations, prompting a need to examine its usage trends for potential policy adjustments. The objective of this study was to assess trends in pregabalin prescribing during a 10-year period, to characterize demographic and clinical characteristics of individuals prescribed pregabalin, and to identify risk factors associated with high-intensity pregabalin use.
Methods
This retrospective, longitudinal study examined trends in pregabalin prescribing from 2010 to 2019 based on data extracted from the Clalit Health Services (CHS) electronic database. Annual pregabalin prescribing rate was calculated individually for each reporting year. A univariable analysis was conducted to compare the demographic and clinical characteristics of pregabalin users in 2019 with those in 2010. Multivariable regression analysis was performed to assess dose-related patterns by specific demographic and clinical characteristics.
Results
Pregabalin prescription rate more than doubled over 10 years [odds ratio (OR) 2.3, p = 0.001], reaching 7.2 [95% confidence interval (CI) 7.18–7.28] prescriptions per 100 CHS members in 2019. The highest prescription rates were observed among the elderly population (13.2 and 24.1 prescriptions per 100 CHS members for those aged 55–74 and over 75 years old, respectively). Same-year administration of pregabalin with opioids, benzodiazepines, and Z-drugs was common; however, the percentage of patients using these drugs together declined in 2019 compared with 2010 (p < 0.001). Males, patients with low socioeconomic status, patients aged 35–54 years, and those who consumed opioids, benzodiazepines, and Z-drugs received higher pregabalin doses.
Conclusion
Pregabalin use has increased significantly in the Israeli adult-based CHS population, consistent with worldwide data. A growing use over time may indicate overprescription. More studies are needed on misuse patterns to identify populations most susceptible to high-dose and high-intensity pregabalin use.
Similar content being viewed by others
Pregabalin intake increased by two-fold among the Israeli adult population in the last decade. |
Males, younger age, low socioeconomic status, and opioids/benzodiazepines use are linked to high-dose pregabalin. |
The proportion of patients using pregabalin with opioids or benzodiazepines has declined in the past decade. |
1 Introduction
Pregabalin is a widely used prescription medication worldwide, belonging to the gabapentinoids class, alongside gabapentin [1]. The European Medicines Agency (EMA) has approved pregabalin for the treatment of epilepsy (as adjunctive therapy), neuropathic pain, and anxiety disorders [2]. The Israeli Drug Registry also lists pregabalin for the treatment of fibromyalgia, however, it is not listed for epilepsy [3].
Recent years have seen steep increases in pregabalin use in the USA, the UK, Europe, and Australia, which raises concerns about overprescription [4,5,6,7]. Further, despite pregabalin’s licensed indications, its use has been extended beyond into other off-label chronic pain conditions, as well as for recreational purposes [1]. This may be because pregabalin has the potential to improve sociability and induce relaxation, dissociation, and euphoria, while enhancing the effects of opioids and other central nervous system (CNS) depressants [8].
Since pregabalin was first marketed, it has been classified in the USA as a Schedule V drug, which controls psychoactive substances with low abuse potential [9, 10]. Despite its reputation as a drug with minimal abuse potential, pregabalin has been reported to be misused and abused. This trend was first identified in 2008 with several cases reported to the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) [11]. Further worldwide epidemiological studies have confirmed this signal of abuse and misuse [12, 13]. There are growing concerns about potential harm stemming from supratherapeutic doses or combined use with opioids, including respiratory depression and overdose-related mortality [10, 12, 14]. These concerns have led the UK to reclassify pregabalin as a class C controlled substance with tighter legal controls over its prescribing in April 2019 [10, 15]. In contrast, pregabalin prescriptions are not regulated by the Israeli legislation of controlled substances.
Worldwide data regarding pregabalin use patterns, misuse, and abuse are still limited. In recent years, several research reported pregabalin misuse among Israeli patients addicted to opioids [1, 16]. However, no updated data on the pregabalin use patterns among general Israeli adult population is available. The current study aims to assess temporal patterns of pregabalin usage in Israel over a decade. An understanding of pregabalin use trends in the Israeli general population is necessary to consider appropriate drug policy changes.
2 Methods
2.1 Data Source
This is a retrospective analysis of the database of Clalit Health Services (CHS). CHS is the largest health medical organization in Israel and provides medical coverage to over 52% of the population [17]. CHS’s patient population closely reflects the Israeli population in terms of demographics, geography, and ethnicity, as shown in previous studies [18,19,20]. The CHS database is highly reliable and quality-controlled and contains clinical, administrative, and financial data collected from primary care and specialists’ clinics, hospitals, pharmacies, and laboratories. Among the data collected are physician visits, patient diagnoses, laboratory and imaging test results, and smoking status [17]. The CHS members’ medication prescriptions and purchases data are available in the CHS database, classified by Anatomical Therapeutic Chemical (ATC) codes and defined daily doses (DDDs) [17, 21]. In addition to prescribed medications, data on consumption of over-the-counter medications from CHS pharmacies are available. Clinical and demographic data are combined with sociodemographic information derived from Israeli national databases [17].
2.2 Study Design
The study consisted of two stages. First, we performed a repeated 10-year descriptive cross-sectional study to evaluate annual pregabalin use between 1 January 2010 and 31 December 2019, by assessing annual pregabalin purchase rate. As a second component of the study, we compared two pregabalin users’ cohorts (2010 and 2019) to estimate changes in patients’ characteristics over the decade and further to identify characteristics associated with high-intensity or high-dose pregabalin use.
2.3 Patient Population and Use Patterns
The study population included all subjects aged 18 years and older who enrolled in CHS and purchased at least one prescription for pregabalin (Anatomical Therapeutic Chemical 5 (ATC5): N03AX16) each calendar year during the study period. For the study cohort, additional data were obtained, including sociodemographic characteristics (age, sex, ethnicity, and socioeconomic status), diagnoses associated with pregabalin indications, and same-year purchases of opioids, benzodiazepines, and/or hypnotic Z-drugs. We categorized the patients into four age groups: 18–34, 35–54, 55–74, and 75 years and older. The diagnoses were coded using International Classification of Diseases Version 10 (ICD-10) (Table S1) [22]. The medications were classified using ATC5 codes and extracted as aggregated data on pharmacologic group level (Table S2) [23]. The definitions of pregabalin user and the calculation of cumulative pregabalin dose are based on purchased prescriptions for pregabalin.
This study was conducted according to regulatory requirements and approved by the institutional review board of CHS under the number 0153-21-COM2.
2.4 Statistical Analyses
The crude and age- and sex-standardized annual pregabalin prescribing rate for 100 CHS members (prescription rate) with corresponding 95% confidence intervals (CIs) were calculated by dividing the annual number of pregabalin prescriptions, by the number of total mid-year CHS members. The p values were adjusted by the Šidák method to counteract the multiple comparisons problem [24].
The temporal trends in annual pregabalin usage and absolute changes in pregabalin prescriptions rates from 2010 to 2019 were assessed using the Cochran–Armitage test for trends. Age-specific and sex-specific analyses were applied.
We used Pearson’s chi-squared test and Welch two-sample t-test to evaluate the change in sociodemographic and clinical characteristics of pregabalin users during the study period including pregabalin dose-dependent usage patterns. The categorical variables are presented as numbers and percentages. Pregabalin cumulative dose is presented as median defined daily dose (DDD) and first and third quartile range (QR), where pregabalin DDD is 300 mg/day [23].
We conducted a multivariable linear regression analysis to assess the difference in annual DDDs between the years 2010 and 2019 while adjusting for covariates, including sex, age, socioeconomic status, and ethnicity [25, 26]. In addition, we evaluated if the changed pregabalin dose-dependent use was associated with same-year use of opioids, benzodiazepines, and Z-drugs. Same-year use was defined when the drug was purchased at least once during the relevant year.
We applied a threshold of p < 0.05 (two-sided) for statistical significance. All statistical analyses were conducted using IBM SPSS (IBM Corp., Armonk, NY, USA) Statistics 29.0 and R Studio 2022.02.0.
3 Results
3.1 The 10-Year Trends of Pregabalin Prescription Rate (2010–2019)
The median pregabalin prescription rate increased over a 10-year period (Table 1). The crude pregabalin prescription rate increased 2.3-fold [odds ratio (OR) 2.3, p < 0.001] from 2010 (3.1%, [95% CI 3.09–3.13%]) to 2019 (7.2%, [95% CI 7.18–7.28%]) (Table 1).
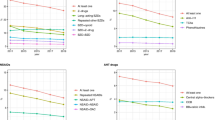
Figure 1 illustrates trends in sex-standardized, age-grouped annual pregabalin prescription rate through the decade.
A consistent increase in the pregabalin prescription rate was observed among all age groups, with a more pronounced increase among the youngest age group (18–34 years) (Fig. 1, Tables S3–6). However, most of the pregabalin users are elderly (24.1 purchases per 100 CHS members in 2019 for those aged over 75 years old). In contrast, the prescription rate among young adults (18–34 years) was comparatively low (0.8 dispensing per 100 CHS members in 2019) (Table S3).
The results of the sex-specific analysis indicated higher pregabalin prescription rate among males than females in the 18–34 and 35–54 age groups (Fig. 1A, B). However, the results could not reach statistical significance due to the limited number of pregabalin users within those age groups.
3.2 Characteristics of Pregabalin Users (2010 Versus 2019)
We analyzed demographic and clinical characteristics of total 51,675 pregabalin users: 15,088 from 2010 and 36,587 users in 2019.
3.2.1 Change in Pregabalin Dose
During the study period, there was significant 50% increase in pregabalin dose (adjusted mean difference (MD) 51.9 DDDs, p < 0.001) (Table 3). During 2010, the median cumulative dose of pregabalin was 49.1 (first and third QR: 14.0–140.0) DDDs compared with 84.0 (first and third QR 24.5–217.0) DDDs in 2019 (Table 2).
3.2.2 Change in Demographic Factors of Pregabalin Users
The median age [standard deviation (SD)] of pregabalin users was 65.6 (14.0) years in 2010 versus 64.8 (15.6) years in 2019 (Table 2). There was a significant increase in pregabalin dose in each age group compared with the youngest one (age group 18–34 years as reference) during those years (Table 3). However, the increase in DDDs MD moderates and becomes smaller with the increase in the following age groups. Between 2010 and 2019, the greatest increase in DDDs was observed in the 35–54 age group, followed by those in the 55–74 age group, and finally in those aged 75 years and over (Table 3).
Overall, most pregabalin recipients were women (55 and 53% in 2010 and 2019, respectively) (Table 2). However, female sex was associated with lower pregabalin doses (adjusted MD − 25.09 DDDs, p < 0.001) (Table 3).
There was an increase of pregabalin users as well an increase in cumulative dose over the decade in all origin groups with no difference between general (non-religious) Jewish, religious Jewish, and Arab populations. Decrease in DDDs MD was observed among Bedouins’ pregabalin users (MD − 24.84 DDDs, p < 0.001) (Tables 2, 3).
A third of pregabalin users were categorized as medium socioeconomic status (SES) (Table 2). Multivariable regression analysis revealed an inverse association between SES and change in cumulative pregabalin dose (Table 3).
3.2.3 Change in Clinical Factors of Pregabalin Users
There are three pregabalin label indications in Israel, including peripheral and central neuropathic pain, generalized anxiety disorder, and fibromyalgia [3]. The vast majority of pregabalin users received treatment for one of the labeled drug indications (98 and 97% in 2010 and 2019, respectively). The most common diagnosis among pregabalin patients was peripheral neuropathy (91% on average, 13,721 in 2010 and 33,328 in 2019). An average of 85.5% of all patients [12,377 (82%) in 2010 and 31,825 (87%) in 2019] were diagnosed with fibromyalgia, and only 0.1% [36 (0.2%) in 2010 and 36 (0.09%) in 2019] were diagnosed with generalized anxiety disorder. It should be noted that a patient might have more than one diagnosis that is labeled indication for pregabalin use. The proportion of each labeled indication remained stable between 2010 and 2019 (Table 2).
Among pregabalin users, we evaluated purchases of opioids, benzodiazepines, and/or Z-drugs. Same-year purchase was common, with an overall amount of 61% of pregabalin users were dispensed at least one prescription of opioid, benzodiazepine, or a Z-drug. However, a significant decrease in opioid use (24 versus 45%, p < 0.001), benzodiazepine use (36 versus 59%, p < 0.001) and Z-drug use (19 versus 33%, p < 0.001) among pregabalin users was observed in 2019 compared with 2010 (Table 2). Same-year purchase of opioids, benzodiazepines, or Z-drugs was associated with statistically significant increased cumulative pregabalin dose based on multivariate analysis (MD of 35.95 DDDs, 23.93 DDDs, and 24.06 DDDs, respectively; p < 0.001) (Table 3).
4 Discussion
To our knowledge, this study presents the most comprehensive analysis to date of cross-sectional comparisons and longitudinal trends in pregabalin use in the Israeli adult population. Our results showed an increase of 2.3-fold in pregabalin use among the adult population between 2010 and 2019, which is consistent with other studies [6, 27,28,29,30]. Several factors may have contributed to this trend. In part, it is possible that the perception that pregabalin poses a lower potential for abuse than opioids has prompted its consideration as an alternative to general pain management. This includes acute perioperative treatments and chronic pain management, aiming to reduce opioid consumption due to the sharp increase observed in the use of opioids, as previously reported in the USA, UK, and Europe [10, 28, 29, 31,32,33]. In this regard, between 2008 and 2018, the use of strong opioids in Israel increased two-fold among elderly patients without cancer and more than seven-fold among patients younger than 65 years old [34]. The Israeli health system is making efforts to control opioid consumption. As social and medical attitudes shift towards pain-intensive management, pregabalin has become more widely accepted and prescribed. The use of pregabalin to enhance analgesia has been observed in cases of chronic neuropathic pain caused by advanced cancer, which is being used alongside the primary treatment of opioids [35, 36]. Economic factors also likely contribute to this trend. Since 2012, pregabalin has become more affordable and economically accessible for patients due to its inclusion in the discount list of drugs provided as part of the complementary health insurance program, Clalit MUSHLAM. Removing the requirement for individual MUSHLAM approval for a discount has also enhanced pregabalin’s accessibility, allowing a wider range of patients to use it.
As observed in other countries, the vast majority of pregabalin prescriptions in our study were for neuropathic pain and pain indications in general [4, 29]. While pregabalin is also registered in Israel for the treatment of generalized anxiety disorder, it is not commonly used for this indication in practice, as shown by our results (0.2 and 0.09% prescriptions dispensed in 2010 and 2019, respectively). A German study also reported an uncommon use for generalized anxiety disorder within the corresponding years [29]. Pregabalin’s infrequent prescription for generalized anxiety disorder in Israel may be related to several factors; however, it is beyond the scope of the current study.
While pregabalin dispensing was most prevalent among the elderly population, a noticeable but non-statistically significant increase in pregabalin prescription rate was observed among young adults aged 18–34 years. Higher doses of pregabalin use were observed in males, patients with low socioeconomic status, patients aged 35–54 years (followed by those aged 55–74), and patients who used opioids, benzodiazepines, and/or Z-drugs. These trends were also noted in other studies; however, higher dose consumption was noted in a younger age group (18–29 years) [37, 38]. We did not find the trend of higher pregabalin doses among youngest group (aged 18–34 years), maybe due to the relatively small sample size of those ages during the study period. A higher pregabalin dose use by young adults may indicate clinical ineffectiveness, no need for dose adjustment in renal failure, which is common in elderly, as well as drug abuse and misuse among patients seeking psychoactive effects [37].
The upward trend in pregabalin use and pregabalin’s DDD was hypothesized to be more dominant among adults who also use opioids, benzodiazepines, and/or Z-drugs. This was based on studies suggesting pregabalin is also being utilized by individuals to enhance the psychoactive effects of these substances including enhanced sociability, euphoria, and, at higher doses, dissociation and sedation [39, 40]. Additionally, other studies have observed a rise in concurrent prescribing, further indicating coadministration potential [30, 41, 42]. This group of patients was found to have higher pregabalin doses, as we had expected. However, our findings suggest a decrease in same-year administration between 2010 and 2019. It is possible that this may be attributed in part to the effectiveness of Israeli policies concerning prescription drug monitoring programs for opioid use. This includes the use of prescription drug monitoring programs, limitations on days’ supply, and the need for special approvals for the long-term use of certain opioids. Therefore, despite the increase in pregabalin use in the past years, the number of same-year prescriptions remained steady or even decreased. In terms of benzodiazepines, the National Program for Quality Indicators in Community Healthcare (QICH) has made significant strides in addressing benzodiazepine use among individuals over 65 years old. The QICH data reveals a decrease in long-term benzodiazepine utilization within this age group, which might be reflected in our results [43, 44]. It is also imperative to acknowledge the unique circumstances of Holocaust survivors, who have been identified as prone to benzodiazepine overuse [45, 46]. Over time, their numbers have naturally decreased, potentially influencing the decline in same-year benzodiazepines and pregabalin prescriptions.
Our retrospective study had several limitations to consider. Due to the nature of our study, we were limited to analyzing prescriptions issued and could not take into account instances in which patients were not taking their prescribed medication as directed. Thus, purchased prescriptions may not always be equivalent to the ones that are actually consumed by patients.
Although several studies in the UK, the USA, and Australia have reported widespread off-label prescribing of pregabalin mostly for treating chronic pain [4, 30, 47], our findings indicate a minimal increase in off-label use. In most cases, CHS insurance covers drug therapy for labeled indications only. Off-label indications treatment is purchased outside the CHS services and data are not available in the CHS database. This fact explains the very low off-label pregabalin use in our study. In addition, prescription indications were derived from the medical history of the patients. It is therefore possible that some indications may be incorrectly classified due to inaccurate coding or outdated medical histories. In view of these limitations and assuming that there are some illegal pregabalin sales for recreational purposes, our findings may contain some inaccuracies.
Finally, we evaluated the purchase of benzodiazepines, Z-drugs, and opioids by pregabalin users. Same-year use was defined when the drug was purchased at least once during the relevant year. Consequently, our results cannot confirm coadministration, as it may be concurrent administration, drug substitution, or unrelated events.
Despite the previously mentioned limitations, this study is the first to examine pregabalin use trends over a 10-year period in Israel. It presents the most comprehensive analysis of cross-sectional comparisons and longitudinal trends in pregabalin use in the Israeli adult population to date. The analysis was based on databases maintained by CHS, the largest healthcare organization in Israel. The large CHS-insured population and its diversity make our findings generalizable to Israel’s adult population. The study results can serve as a foundation for further research in Israel aimed at providing a clear and precise depiction of pregabalin utilization patterns, particularly regarding high-intensity use, which may be at increased odds of misuse and abuse.
5 Conclusion
Our study revealed an overall consistent increase in pregabalin use in Israel between 2010 and 2019. The study detected several changes in drug consumption characteristics over the 10-year study period. Most of the trends in use correlate with previous worldwide publications.
References
Sason A, Adelson M, Schreiber S, Peles E. Pregabalin misuse in methadone maintenance treatment patients in Israel: prevalence and risk factors. Drug Alcohol Depend. 2018;189:8–11. https://doi.org/10.1016/j.drugalcdep.2018.04.025.
The European Public Assessment Report (EPAR) for Lyrica. European Medicines Agency (EMA); n.d. https://www.ema.europa.eu/en/medicines/human/EPAR/lyrica. Accessed 23 Dec 2023.
Lyrica: prescribing information. The Israeli Drug Registry, Ministry of Health; n.d. https://israeldrugs.health.gov.il/#!/medDetails/132. Accessed 22 Dec 2023.
Schaffer AL, Busingye D, Chidwick K, Brett J, Blogg S. Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study. BJGP Open. 2021;5:1–10. https://doi.org/10.3399/bjgpopen20X101120.
Johansen ME. Gabapentinoid use in the United States 2002 through 2015. JAMA Intern Med. 2018;178:292–4. https://doi.org/10.1001/JAMAINTERNMED.2017.7856.
Torrance N, Veluchamy A, Zhou Y, Fletcher EH, Moir E, Hebert HL, et al. Trends in gabapentinoid prescribing, co-prescribing of opioids and benzodiazepines, and associated deaths in Scotland. Br J Anaesth. 2020;125:159–67. https://doi.org/10.1016/J.BJA.2020.05.017.
Goodman CW, Brett AS. Gabapentin and pregabalin for pain—is increased prescribing a cause for concern? New Engl J Med. 2017;377:411–4. https://doi.org/10.1056/NEJMP1704633/SUPPL_FILE/NEJMP1704633_DISCLOSURES.PDF.
Elliott SP, Burke T, Smith C. Determining the toxicological significance of pregabalin in fatalities. J Forensic Sci. 2017;62:169–73. https://doi.org/10.1111/1556-4029.13263.
Drug Enforcement Administration D o. J. Schedules of controlled substances: placement of pregabalin into schedule V. Final rule, vol 70. 2005.
Bonnet U, Scherbaum N. How addictive are gabapentin and pregabalin? A systematic review. Eur Neuropsychopharmacol. 2017;27:1185–215. https://doi.org/10.1016/J.EURONEURO.2017.08.430.
World Health organization. PREGABALIN pre-review report. Expert Committee on Drug Dependence, Thirty-ninth Meeting. 2017.
Evoy KE, Sadrameli S, Contreras J, Covvey JR, Peckham AM, Morrison MD. Abuse and misuse of pregabalin and gabapentin: a systematic review update. Drugs. 2020;81(1):125–56. https://doi.org/10.1007/S40265-020-01432-7.
Hägg S, Jönsson AK, Ahlner J. Current evidence on abuse and misuse of gabapentinoids. Drug Saf. 2020;43:1235. https://doi.org/10.1007/S40264-020-00985-6.
Evoy KE, Covvey JR, Peckham AM, Reveles KR. Gabapentinoid misuse, abuse and non-prescribed obtainment in a United States general population sample. Int J Clin Pharm. 2021;43(4):1055–64. https://doi.org/10.1007/S11096-020-01217-8.
Nahar LK, Andrews R, Murphy KG, Paterson S. Misuse of gabapentin and pregabalin may be underestimated. BMJ. 2017;359: j5312. https://doi.org/10.1136/BMJ.J5312.
Peles E, Sason A, Schreiber S, Adelson M. Pregabalin misuse: motives, pattern, and knowledge about its risks among patients in methadone maintenance treatment. J Psychoact Drugs. 2021;53:238–46. https://doi.org/10.1080/02791072.2020.1861392.
Clalit Research Institute. n.d. http://clalitresearch.org/about-us/our-data/. Accessed 19 July 2023.
Eder L, Cohen AD, Feldhamer I, Greenberg-Dotan S, Batat E, Zisman D. The epidemiology of psoriatic arthritis in Israel—a population-based study. Arthritis Res Ther. 2018. https://doi.org/10.1186/s13075-017-1497-4.
Gendelman O, Shapira R, Tiosano S, Kuntzman Y, Tsur AM, Hakimian A, et al. Utilisation of healthcare services and drug consumption in fibromyalgia: a cross-sectional analysis of the Clalit Health Service database. Int J Clin Pract. 2021. https://doi.org/10.1111/ijcp.14729.
Yavne Y, Tiosano S, Watad A, Comaneshter D, Cohen AD, Amital H. Investigating the link between ischemic heart disease and Behcet’s disease: a cross-sectional analysis. Int J Cardiol. 2017;241:41–5. https://doi.org/10.1016/j.ijcard.2017.02.135.
Marom O, Rennert G, Stein N, Landsman K, Pillar G. Characteristics and trends in hypnotics consumption in the largest health care system in Israel. Sleep Disord. 2016. https://doi.org/10.1155/2016/8032528.
Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM). n.d. https://icd10cmtool.cdc.gov/?fy=FY2023. Accessed 10 July 2021.
ATC/DDD Index 2021. n.d. https://www.whocc.no/atc_ddd_index/. Accessed 10 July 2021.
Sidak Z. Rectangular confidence regions for the means of multivariate normal distributions. J Am Stat Assoc. 1967;62:626–33. https://doi.org/10.2307/2283989.
Shaked O, Korn L, Shapiro Y, Koren G, Zigdon A. Socio-demographic characteristics and their relation to medical service consumption among elderly in Israel during the COVID-19 lockdown in 2020 as compared to the corresponding period in 2019. PLoS ONE. 2022. https://doi.org/10.1371/journal.pone.0278893.
Abdel-Rahman N, Yoffe N, Siman-Tov M, Radomislensky I, Peleg K. Achieving ethnic equality in the Israel trauma healthcare system: the case of the elderly population. Isr J Health Policy Res. 2019. https://doi.org/10.1186/s13584-019-0294-8.
Viniol A, Ploner T, Hickstein L, Haasenritter J, Klein KM, Walker J, et al. Prescribing practice of pregabalin/gabapentin in pain therapy: an evaluation of German claim data. BMJ Open. 2019. https://doi.org/10.1136/bmjopen-2018-021535.
Ashworth J, Bajpai R, Muller S, Bailey J, Helliwell T, Harrisson SA, et al. Trends in gabapentinoid prescribing in UK primary care using the Clinical Practice Research Datalink: an observational study. Lancet Reg Health Eur. 2023;27:100579. https://doi.org/10.1016/j.lanepe.2022.100579.
Flemming R. Patterns of pregabalin prescribing in four German federal states: analysis of routine data to investigate potential misuse of pregabalin. BMJ Open. 2022. https://doi.org/10.1136/bmjopen-2021-060104.
Montastruc F, Loo SY, Renoux C. Trends in first gabapentin and pregabalin prescriptions in primary care in the United Kingdom, 1993–2017. New Engl J Med. 2018;320:2149–51. https://doi.org/10.1001/jama.2018.12358.
Bonnie RJ, Ford MA, Phillips JK, editors. Pain Management and the opioid epidemic. Washington, DC: National Academies Press; 2017. https://doi.org/10.17226/24781.
Grant MC, Betz M, Hulse M, Zorrilla-Vaca A, Hobson D, Wick E, et al. The effect of preoperative pregabalin on postoperative nausea and vomiting: a meta-analysis. Anesth Analg. 2016;123:1100–7. https://doi.org/10.1213/ANE.0000000000001404.
Zhang J, Ho KY, Wang Y. Efficacy of pregabalin in acute postoperative pain: a meta-analysis. Br J Anaesth. 2011;106:454–62. https://doi.org/10.1093/bja/aer027.
Miron O, Zeltzer D, Shir T, Balicer RD, Einav L, Feldman BS. Rising opioid prescription fulfillment among non-cancer and non-elderly patients-Israel's alarming example. Reg Anesth Pain Med. 2021;46(5):455–6. https://doi.org/10.1136/rapm-2020-101924.
Swarm RA, Paice JA, Anghelescu DL, Are M, Bruce JY, Buga S, et al. Adult cancer pain, version 3.2019. JNCCN J Natl Compr Cancer Netw. 2019;17:977–1007. https://doi.org/10.6004/jnccn.2019.0038.
Shkodra M, Caraceni A. Treatment of neuropathic pain directly due to cancer: an update. Cancers (Basel). 2022. https://doi.org/10.3390/cancers14081992.
Cairns R, Schaffer AL, Ryan N, Pearson SA, Buckley NA. Rising pregabalin use and misuse in Australia: trends in utilization and intentional poisonings. Addiction. 2019;114:1026–34. https://doi.org/10.1111/ADD.14412.
Bodén R, Wettermark B, Brandt L, Kieler H. Factors associated with pregabalin dispensing at higher than the approved maximum dose. Eur J Clin Pharmacol. 2014;70:197–204. https://doi.org/10.1007/s00228-013-1594-5.
Lancia M, Gambelunghe A, Gili A, Bacci M, Aroni K, Gambelunghe C. Pregabalin abuse in combination with other drugs: monitoring among methadone patients. Front Psychiatry. 2020. https://doi.org/10.3389/fpsyt.2019.01022.
Snellgrove BJ, Steinert T, Jaeger S. Pregabalin use among users of illicit drugs: a cross-sectional survey in southern Germany. CNS Drugs. 2017;31:891–8. https://doi.org/10.1007/s40263-017-0467-3.
Chen C, Lo-Ciganic WH, Winterstein AG, Tighe P, Wei YJJ. Concurrent use of prescription opioids and gabapentinoids in older adults. Am J Prev Med. 2022;62:519–28. https://doi.org/10.1016/j.amepre.2021.08.024.
Evoy KE, Covvey JR, Peckham AM, Reveles KR. Gabapentinoid misuse, abuse and non-prescribed obtainment in a United States general population sample. Int J Clin Pharm. 2021;43:1055–64. https://doi.org/10.1007/s11096-020-01217-8.
Manor O, Abu Ahmad W, Ben-Yehuda A, Horwitz E, Wolff-Sagy Y, Paltiel O, et al. The 2011–2015 National Program for Quality Indicators in Community Healthcare in Israel (QICH) Report. https://israelhealthindicators.org.
Calderon-Margalit, Abu-Ahmed W, Ben-Yehuda A, Horwitz E, Krieger M, Manor O, et al. The 2015–2017 National Program for Quality Indicators in Community Healthcare in Israel (QICH) Report. https://israelhealthindicators.org.
Blumstein T, Benyamini Y, Chetrit A, Mizrahi EH, Lerner-Geva L. Prevalence and correlates of psychotropic medication use among older adults in Israel: cross-sectional and longitudinal findings from two cohorts a decade apart. Aging Ment Health. 2012;16:636–47. https://doi.org/10.1080/13607863.2011.644262.
Ayalon L, Gross R, Yaari A, Feldhamer E, Balicer RD, Goldfracht M. Patients’ and physicians’ characteristics associated with the purchase of benzodiazepines by older primary care patients in Israel. Adm Policy Ment Health Ment Health Serv Res. 2013;40:117–23. https://doi.org/10.1007/s10488-011-0381-9.
Peet ED, Dana B, Sheng FY, Powell D, Shetty K, Stein BD. Trends in the concurrent prescription of opioids and gabapentin in the US, 2006 to 2018. JAMA Intern Med. 2022. https://doi.org/10.1001/jamainternmed.2022.5268.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by {institution name}. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Conflict of interest
The authors have no relevant conflicts of interests to disclose.
Availability of data and material
Data supporting the findings of this study are accessible from the corresponding author upon reasonable request.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki and approved by the institutional review board of Clalit Health Services (CHS). The ethic approval number is 0153-21-COM2.
Consent to participate
The authors received a full exemption from informed consent because this study consists of existing data and given that anonymized data were used.
Consent for publication
Not applicable.
Code availability
Not applicable.
Author contributions
All authors contributed to the study conception and design. WAA conducted the statistical analyses with guidance from VR and NBK. The first draft of the manuscript was written by NBK. All authors contributed significantly to draft refinement and data interpretation. All authors have read and approved the final submitted manuscript and agree to be accountable for the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Benassayag Kaduri, N., Dressler, R., Abu Ahmad, W. et al. Trends in Pregabalin Use and Prescribing Patterns in the Adult Population: A 10-Year Pharmacoepidemiologic Study. CNS Drugs 38, 153–162 (2024). https://doi.org/10.1007/s40263-024-01064-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-024-01064-5