Abstract
To adequately evaluate the corticospinal and spinal plasticity in health and disease, it is essential to understand whether and to what extent the corticospinal and spinal responses fluctuate systematically across multiple measurements. Thus, in this study, we examined the session-to-session variability of corticospinal excitability for the ankle dorsiflexor tibialis anterior (TA) in people with and without incomplete spinal cord injury (SCI). In neurologically normal participants, the following measures were obtained across 4 days at the same time of day (N = 13) or 4 sessions over a 12-h period (N = 9, at 8:00, 12:00, 16:00, and 20:00): maximum voluntary contraction (MVC), maximum M-wave and H-reflex (Mmax and Hmax), motor evoked potential (MEP) amplitude, and silent period (SP) after MEP. In participants with chronic incomplete SCI (N = 17), the same measures were obtained across 4 days. We found no clear diurnal variation in the spinal and corticospinal excitability of the TA in individuals with no known neurological conditions, and no systematic changes in any experimental measures of spinal and corticospinal excitability across four measurement days in individuals with or without SCI. Overall, mean deviations across four sessions remained in a range of 5–13% for all measures in participants with or without SCI. The study shows the limited extent of non-systematic session-to-session variability in the TA corticospinal excitability in individuals with and without chronic incomplete SCI, supporting the utility of corticospinal and spinal excitability measures in mechanistic investigation of neuromodulation interventions. The information provided through this study may serve as the reference in evaluating corticospinal plasticity across multiple experimental sessions.
Similar content being viewed by others
Introduction
Corticospinal activity is essential in human motor control (Ridding and Rothwell 1997; Capaday et al. 1999; Petersen et al. 2001; Pascual-Leone et al. 2002; Siebner and Rothwell 2003; Wirth et al. 2008a, 2008b; Barthelemy et al. 2010), and its plasticity is the key for learning motor skills and for re-learning them after central nervous system lesions (Classen et al. 1998; Karni et al. 1998; Butefisch et al. 2000; Liepert et al. 2000a, b; Rioult-Pedotti et al. 2000; Nudo 2003; Ziemann 2004; Ziemann et al. 2004, 2006; Ramanathan et al. 2006). To properly evaluate the corticospinal plasticity in health and disease, it is critical to establish whether and to what extent the corticospinal and spinal responses fluctuate systematically across multiple measurement times. In monkeys, rats, mice, and humans, the excitability of the soleus H-reflex pathway changes systematically throughout day (i.e., diurnal variation) (Wolpaw et al. 1984; Chen and Wolpaw 1994; Carp et al. 2006a; Lagerquist et al. 2006), but not across days (i.e., day-to-day variation) (Wolpaw 1987; Chen and Wolpaw 1995; Carp et al. 2006b; Thompson et al. 2009). In persons with no known neurological conditions, the soleus H-reflex and maximum voluntary contraction (MVC) force increase from the morning to evening, while the flexor carpi radialis (wrist flexor) H-reflex and MVC force do not change throughout day (Lagerquist et al. 2006), suggesting that diurnal variations in voluntary activation of the muscle and spinal reflex excitability may differ between muscles. Appearance of diurnal rhythm may also differ between the spinal reflex excitability and the corticospinal excitability, even in the same muscle; when the soleus corticospinal excitability was measured as the size of corticospinal motor evoked potential (MEP), its diurnal rhythm differed between participant chronotypes [i.e., morning people vs. evening people (Tamm et al. 2009)]. Thus, what emerges from the available studies is that the presence, pattern, and extent of systematic excitability variation likely differs between the pathways examined.
Currently, the presence of diurnal variation or the extent of the stability of the corticospinal excitability for the ankle dorsiflexor tibialis anterior (TA) is not known. Since the corticospinal drive is important for TA activation (Brouwer and Ashby 1992; Schubert et al. 1997, 1999; Capaday et al. 1999) and in particular during the swing phase of locomotion, enhancing the corticospinal drive for the TA could be an effective therapeutic strategy for augmenting rehabilitation of gait function in people after spinal cord injury (SCI) and other neuromuscular disorders (Thomas and Gorassini 2005; Everaert et al. 2010; Urbin et al. 2017; Thompson et al. 2019; Thompson and Sinkjaer 2020). To ensure the proper interpretation of clinical and mechanistic study findings involving TA corticospinal functions, this study set out to establish the variability and stability of TA corticospinal excitability in individuals with and without corticospinal lesions.
Specifically, in adults with no known neurological conditions, we examined diurnal (within-day) variability in the measures of spinal and corticospinal excitability for the TA and compared its extent and pattern with those of day-to-day variability. If, for instance, one of the measures showed a trend of increasing or decreasing in amplitude from the first (8:00) measurement to the last (20:00) measurement (i.e., diurnal variability is present), examining the variation trend across four days of measurements would allow us to see if such variation occurs when the measurements are simply repeated multiple times.
In adults with chronic incomplete SCI, we examined the extent of day-to-day variability in spinal and corticospinal excitability for the TA, across multiple days of measurements made at the same time of day. Note that, in the present study, we opted not to examine diurnal variability in participants with SCI. It would not be possible to control for the effects of medication that most of those individuals had been taking chronically daily; medication’s peak plasma levels, bioavailability, and pharmacological and physiological effects (Ghanavatian and Derian 2022) would not be the same throughout day, and medication effectiveness would also be hard to estimate or control for throughout day for each person. Thus, in individuals with SCI, we focused on estimating the day-to-day variability in various measures of spinal and corticospinal excitability.
Methods
Study participants
In the present study, to examine the variability in the corticospinal and spinal responses within and across days, measurements were made in two separate series of experiments. Of 16 individuals with no known neurological conditions who participated in the study, 9 (3 men and 6 women aged 36 ± 10 years) were studied with the within-day series of experiments and 13 (6 men and 7 women, aged 33 ± 7 years) were studied with the across-day series of experiments. Six individuals participated in both the within-day and across-day experiments. In this study, we set the minimum sample size of N = 9 for each experiment, assuming a 20% change in the H-reflex value as observed in Lagerquist et al. (2006). Over the four measurement time points, the sample size of N = 9 would detect a statistically significant systematic within-day or across-day change with 84% power.
Seventeen adults (13 men and 4 women, aged 50 ± 11 years) with well-defined stable impairment of weak ankle dorsiflexion (i.e., foot drop) due to a chronic spinal cord lesion participated in the across-day series of experiments. Thus, participants with SCI were studied only with the across-day experiments. For each participant with SCI, a physiatrist or a neurologist determined each prospective individual’s eligibility for the study. The profiles of participants with SCI are summarized in Table 1. The inclusion criteria were (1) neurologically stable (> 1 year post SCI); (2) medical clearance to participate; (3) ability to ambulate at least 10 m with or without an assistive device (e.g., walker, cane, and crutches); (4) signs of weak ankle dorsiflexion at least unilaterally (i.e., manual muscle strength test score < 5); (5) medically stable at the time of study enrollment. Stable use of anti-spasticity medication (e.g., baclofen, diazepam, tizanidine) was permitted. Exclusion criteria were (1) motoneuron injury; (2) known cardiac condition (e.g., history of myocardial infarction, congestive heart failure, pacemaker use); (3) medically unstable condition; (4) severe cognitive impairment; (5) a history of epileptic seizures; (6) metal implants in the cranium, (7) implanted biomedical device in or above the chest (e.g., a cardiac pacemaker, cochlear implant), (8) no measurable H-reflex or MEP on elicitation, and (9) unable to produce any voluntary TA electromyography (EMG) activity. The inclusion criteria for the participants with no known neurological conditions were no history of neurologic injury or disease and no history of orthopedic injury to the tested side.
The study protocol was approved by the Institutional Review Boards of Helen Hayes Hospital New York State Department of Health and the Medical University of South Carolina, and all participants gave written consent prior to participation.
General procedure
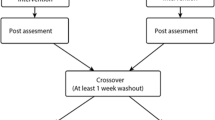
In the present study, the corticospinal and spinal responses were examined in two separate series of experiments: the within-day protocol and the across-day protocol. With the within-day protocol, the measurements were made at 8:00, 12:00, 16:00, and 20:00 within a 12-h period of the same day. With the across-day protocol, the measurements were made in 4 separate sessions that occurred at the same time across 4 different days, separated by at least one day of rest. Participants were instructed to not refrain from their usual activities or diet but were asked not to introduce anything new or different during or in between testing days. Current medications and dietary and exercise habits were recorded during the screening sessions.
All measurements were made while the participant comfortably sat in a chair with the testing leg fixed in a custom-made apparatus that held the hip, knee, ankle joint angles at approximately 70°, 60°, and − 10° (i.e., 10° of plantarflexion at the ankle), respectively. After EMG recording electrodes were placed over the TA and soleus, and the common peroneal nerve (CPn) stimulating electrodes were placed at the neck of fibula, the maximum voluntary contraction (MVC) level of TA EMG was measured as the mean rectified EMG amplitude. The TA H-reflex–M-wave recruitment curve was then measured using the CPn stimulation while the participant maintained about 15% MVC level of rectified TA EMG activity (in participants with no known neurological injuries) and at rest (in participants with SCI) (see below, Electrical stimulation and EMG recording). Stimulus intensity was increased from the H-reflex or M-wave (whichever occurs at a weaker stimulus) threshold to the maximum H-reflex (Hmax) to an intensity just above that needed to elicit the maximum M-wave (Mmax) in increments of 1.25–2.5 mA (Kido et al. 2004a, b; Thompson et al. 2006, 2013a; Makihara et al. 2014). Approximately ten different intensities were used to obtain each recruitment curve, and four EMG responses were averaged to measure the H-reflex and M-wave at each intensity. Following the CPn stimulation, the input–output relation of the corticospinal pathway for the TA was obtained by increasing the transcranial magnetic stimulation (TMS) intensity from below the MEP threshold to the level at which the MEP reached its maximum amplitude (MEPmax). Ten-to-twenty MEPs were then measured at the TMS intensity that originally produced a half-maximum MEP (MEPh; typically, 10–20% above threshold) (Knash et al. 2003; Kido Thompson and Stein 2004; Thompson et al. 2011). All MEP measurements were made while the participant voluntarily maintained ≈ 15% MVC level (for participants without SCI) or ≈ 30% MVC level (for participants with SCI) of TA EMG activity. Silent periods after MEP were also measured at the MEPmax (SPmax) and at the MEPh (SPh). A typical first measurement session took approximately 45 min, including the time for determining the TMS optimum location and mapping all the stimulating and EMG recording electrode locations. For subsequent sessions, all the measurements were completed within 20 min.
EMG recordings and electrical stimulation
EMG signals were obtained from the TA and soleus using surface self-adhesive Ag–AgCl electrodes (2.2 × 3.5 cm, Vermed, Inc., Bellows Falls, VT). EMG recording electrodes were placed over the muscle belly for the TA approximately 1/3 the distance between the fibular head and the medial malleolus and about 2 cm below the gastrocnemius in line with the Achilles tendon for the soleus, with their centers ~ 3 cm apart. The signals were amplified and band-pass filtered at 10–1000 Hz (Bortec Biomedical Ltd., Calgary, Canada), and sampled at 3200–5000 Hz. During experimental sessions, EMG signals were also rectified online, averaged every 100 ms, and shown on the feedback screen in front of the participant, so that the participant could monitor the ongoing EMG activity level. For the TA MVC EMG amplitude measurements, the absolute EMG was measured in three trials of ≈ 3-s maximum isometric dorsiflexion effort, separated by at least 1 min of rest in-between.
For the CPn stimulation, the cathode electrode (2.2 × 2.2 cm, Vermed, Inc.) was placed at the neck of fibula and the anode electrode (2.2 × 3.5 cm, Vermed, Inc.) was located at about 2 cm anterior to the cathode. Positions of the stimulating electrode pair were carefully adjusted such that the least amount of stimulus current was required to elicit the M-wave in the TA. CPn stimuli to elicit the M-wave and H-reflex in the TA were 0.5-ms single square pulses delivered from Grass S48 stimulator with SIU-5 stimulation isolation unit and CCU1 constant current unit (Natus Neurology, Warwick, RI). The stimulation was triggered when the participant maintained about 15% MVC level of TA and the resting level (i.e., < 7 μV) of soleus background EMG activity (in participants without SCI) or the resting level (i.e., < 7 μV) of TA and soleus background EMG activity (in participants with SCI) for at least 2 s and at least 5 s had passed since the last stimulus. Note that in participants with SCI, the TA H-reflex–M-wave recruitment curve was measured at rest to reduce the number of trials for which the participant would have to produce and maintain a preset level of voluntary TA activation; this was done to minimize the potential muscle fatigue from affecting MEP measurements.
To avoid session-to-session variability in electrode placement, CPn stimulating, and EMG recording electrode positions were carefully mapped in relation to landmarks on the skin (e.g., scars or moles), and the same investigator prepared the skin and placed the electrodes every session for every participant.
Transcranial magnetic stimulation
In each experimental session, MEP measurements were made while the participant was seated comfortably in a chair with hip, knee, and ankle joints fixed in a custom-made apparatus, keeping the angles of these joints at approximately 70°, 60°, and − 10°, respectively. Single-pulse monophasic TMS was delivered from MagStim 200–2 (Jali Medical Inc., Woburn, MA) via a custom-made, batwing coil with radii of 8 cm; the coil is a modified version of figure-of-8 coil with the outer halves of the two circular coils slightly (25°) bent inward. The coil was held over the scalp such that the induced current flowed in the posterior–anterior direction in the brain. TMS was triggered when the participant had voluntarily maintained ≈ 15% MVC level (in participants without SCI) or ≈ 30% MVC level (for participants with SCI) of TA EMG activity for at least 2 s and at least 5.5 s has passed since the last stimulus. Note that the TA background EMG level differed between neurologically normal participants (≈ 15% MVC) and participants with SCI (≈ 30% MVC), due to their typical differences in ease of voluntary EMG control, MEP size development, and MEP stability at different background EMG levels (Devanne et al. 1997; Garvey et al. 2001). In this study, for background TA activity level for MEP measurements in participants with no injuries, we chose ≈ 15% MVC level, because it is roughly the level of TA activity observed across the swing-phase of walking (Kido et al. 2004a, b). Then, in participants with SCI, in whom higher background EMG (i.e., higher than ≈ 15% MVC level) would help to reduce the TMS intensity to elicit MEPs and help to measure MEPs of more substantial amplitudes (Davey et al. 1999), we aimed to set TA background EMG amplitude close to the level (in mV) generated by individuals without SCI; this led us to using ≈ 30% MVC level for TA background EMG in previous MEP studies in people with weak dorsiflexion due to SCI (Thompson et al. 2011, 2018) and it worked well. Thus, in this study, in participants with SCI, the TA background EMG level was generally aimed at ≈ 30% MVC level.
In the initial session, the optimal TMS location was determined as the location at which the lowest stimulus intensity was required to activate the TA, by moving the coil over the motor areas of the scalp, typically from 0 to 2 cm lateral to and from − 1 to 2 cm posterior to the vertex (corresponding to Cz of the international 10–20 system for EEG). For all subsequent sessions, the same investigator measured and located the participant’s vertex; the same investigator held the TMS coil to minimize the session-to-session variability in a given participant’s MEP measurements; and TMS was applied at the optimal location (e.g., 1 cm lateral and 1 cm posterior to the vertex) determined in the initial session. At the optimal location, the input–output curve was measured by increasing the TMS intensity, expressed as a percentage of the maximum stimulator output (MSO), in steps of 5% from below the MEP threshold until the MEP reached its plateau (MEPmax). A typical TMS intensity range used for the input–output curve measurement was 40–70% MSO for participants without SCI, and the range was the same for participants with SCI in whom MEPmax could be obtained. Four MEPs were collected at each stimulus level, and the intensity eliciting a half-maximum MEP (MEPh) was determined as the closest to the estimated parameter h, after fitting the data with a sigmoid curve of the form:
where y is the MEP, b is the background activity in the absence of an MEP, x is % of the TMS maximum stimulator output, m is the maximum MEP, h is the stimulus level producing a half-maximum MEP, and w is a measure of the width of the curve (Devanne et al. 1997; Knash et al. 2003; Kido Thompson and Stein 2004; Thompson et al. 2011). We collected 10–20 MEPs evoked at this TMS intensity for a MEPh (typically 10–20% above estimated threshold [as the minimum TMS intensity required to induce MEPs of > 0.1 mV in 50% of the trials (Rossini et al. 1994)].
Note that in 9 participants with SCI the full MEP recruitment curve could not be obtained and the MEPmax could not be determined; this was because the maximum stimulator output of TMS was not sufficient to attain the MEPmax or the higher TMS intensity needed for MEPmax measurement could not be tolerated. In those individual, MEPh measurements were made at the TMS intensity of 10–20% above the estimated threshold, based on the slope of the available MEP recruitment curve data.
Data analysis
In this study, we measured the TA MVC, Mmax, Hmax, MEPmax, MEPh, SPmax (SP duration at the MEPmax) and SPh (SP duration at the MEPh). For the evoked potentials (i.e., Mmax, Hmax, MEPmax, MEPh) the mean value was calculated as the peak-to-peak amplitude in each session in each participant. For the MVC, the mean EMG amplitude (in absolute value) over the period of MVC effort was calculated in each of the three MVC attempts, and then the average of the three was reported as the TA MVC. Silent periods (SPmax and SPh) were measured as the period from the end of the MEP to the recovery of background EMG activity in 50% of responses (Garvey et al. 2001; Knash et al. 2003; Kido Thompson and Stein 2004; Thompson et al. 2011). End of MEP was determined, on the full wave rectified EMG signal, as the time when the MEP EMG burst diminished and fell below the pre-stimulus (i.e., background) EMG level. Note that in 4 participants with SCI, SPh could not be determine as the recovery of background EMG activity was not observed.
Statistical analysis
For each of the seven above-mentioned EMG measures (i.e., MVC, Mmax, Hmax, MEPmax, MEPh, SPmax, and SPh) we perform the following analyses. First, for the within-day dataset and across-day dataset in participants without SCI, and for the across-day dataset in participants with SCI, we calculated the standard error of measurement (SEM). We also calculated the coefficient of variation (CV) per individual. Then, the CV values were compared between the protocols (within-day and across-day) and cohorts (participants with SCI and participants without SCI) by t test. For each participant and for each measure, the mean absolute deviation of four measurements was also calculated. We computed the intraclass correlation (ICC) assuming random participants and random sessions (ICC(2, 1)) (McGraw and Wong 1996). ICC values range from 0 to 1, with 1 denoting perfect repeatability across sessions. ICC values of greater than 0.6 are considered supportive of reasonably high repeatability (McGraw and Wong 1996). To quantify the mean variance across the four sessions and to test for significant predictors of the EMG measures, for the data from participants with no neurological injuries, linear mixed models (LMM) that considered the fixed effects of PROTOCOL (i.e., within-day vs. across-day) and SESSION (i.e., four measurement time points either within-day or across-days) with participant as the random effect (intercept) were used for analyses. These models assumed random intercepts and slopes for each participant to account for the longitudinal (i.e., repeated measures) design. For the data from participants with SCI, a similar mixed effects model was employed to assess the effect of SESSION with participant level random intercepts and slopes and an overall fixed slope effect.
The R language (version 4.3.1, R Core Team 2023) was used for all statistical analyses. We used the R packages lme4 for mixed effects modeling (Bates et al. 2015) and irr for ICC estimates (Gamer et al. 2019). Power calculations were performed using the simr package (Green and MacLeod 2016) in R.
Results
Reliability and stability of repeated EMG measurements
Prior to assessing the presence and extent of physiological variability in EMG measures, we assessed the reliability and variability of repeated measurements by calculating SEM and CV. Mean and SEM values for Mmax, Hmax, MEPmax, MEPh, SPmax, SPh, and MVC are summarized in Table 2. For CV in participants without SCI, the values were compared between the within-day and across-day protocol groups. CVs were below 20% on average (except for Mmax for which CVs were even smaller) and did not differ between the protocol groups; Mmax: 6.9 ± 2.6 (mean ± SD)% vs. 5.8 ± 3.1% (p = 0.37 by two-tailed t test); Hmax: 17.2 ± 9.5% vs. 14.6 ± 6.9% (p = 0.51); MEPmax: 10.5 ± 5.8% vs. 15.1 ± 6.2% (p = 0.09); MEPh: 14.6 ± 7.1% vs. 18.7 ± 10.9% (p = 0.30); SPmax: 11.7 ± 9.5% vs. 14.6 ± 8.5% (p = 0.48); SPh: 16.7 ± 9.0% vs. 11.6 ± 5.3% (p = 0.15); and MVC: 13.0 ± 6.8% vs. 9.5 ± 7.2% (p = 0.27). CVs in participants with SCI were 10.3 ± 3.0% for Mmax, 21.3 ± 12.8% for Hmax, 19.1 ± 5.5% for MEPmax, 8.9 ± 4.1% for MEPh, 8.8 ± 4.5% for SPmax, 11.8 ± 5.6% for SPh, and 11.7 ± 7.5% for MVC. When these CVs were compared to the across-day group of participants without SCI by t test, p = 0.002, 0.41, 0.72, 0.005, 0.32, 0.84, and 0.87 for these seven measures, respectively.
We also assessed the reproducibility of EMG measurements by calculating the ICC. For the within-day protocol in participants with no known neurological injuries, ICCs were 0.83, 0.93, 0.89, 0.68, 0.82, 0.70, and 0.90 for Mmax, Hmax, MEPmax, MEPh, SPmax, SPh, and MVC, respectively. For the across-day protocol in participants with no known neurological injuries, ICCs were 0.98, 0.90, 0.89, 0.71, 0.68, 0.73, and 0.84 for Mmax, Hmax, MEPmax, MEPh, SPmax, SPh, and MVC, respectively. For the across-day protocol in participants with SCI, ICCs were 0.95, 0.98, 0.93, 0.97, 0.75, 0.90, and 0.96 for Mmax, Hmax, MEPmax, MEPh, SPmax, SPh, and MVC, respectively (see Fig. 1).
TA background EMG for these measurements were, on average, 43 μV (with SEM of 3.0 μV) for the within-day protocol group and 47 μV (with SEM of 3.5 μV) for the across-day protocol group of participants without SCI, corresponding to 17% MVC and 15% MVC, respectively. For the participants with SCI, TA background EMG for MEP measures were 35 μV (with SEM of 2.9 μV) on average, corresponding to 30% MVC. The ICCs calculated for TA background EMG for these measurements were all > 0.95 (not shown) for the within- and across-day protocols in the non-SCI group and for the across-day protocol in the SCI group. Thus, we can reasonably assume that TA background EMG was maintained stable across multiple sessions for each protocol and group in this study.
Within-day and across-day variability in the excitability of corticospinal and spinal pathways in people without neurological injuries
TA Mmax, Hmax, MEPmax, MEPh, SPmax, SPh, and MVC in participants without SCI, across four measurement time points within-day and across 4 days, are expressed in %mean (i.e., the mean of the four measurements) and presented in Figs. 2, 3. As seen here there are no clear systematic (e.g., linear, or monotonic) increases or decreases across 4 sessions in the measures obtained in this study in participants without neurological disease or injury.
Measures of corticospinal and spinal excitability for the tibialis anterior (TA) repeated at 4 different times during a single day in participants with no known neurological disorders. a–c Peristimulus TA EMG sweeps for the Mmax, Hmax and MEPmax from a single participant. For each sweep ≈ 4 responses are averaged together. The grey/shaded area indicates the time window for which each variable was measured. d–j The mean value across all participants (thick black line) and individual participant values (each line for each participant) for Mmax, Hmax, MEPmax, MEPh, SPmax, SPh, and MVC (N = 9). All values are expressed as %mean value
Measures of corticospinal and spinal excitability for the tibialis anterior (TA) repeated over four different days at approximately the same time of day in participants with no known neurological disorders. a–c Peristimulus TA EMG sweeps for the Mmax, Hmax and MEPmax from a single participant. For each sweep ≈ 4 responses are averaged together. The grey/shaded area indicates the time window for which each variable was measured. d–j The mean value across all participants (thick black line) and individual participant values (each line for each participant) for Mmax, Hmax, MEPmax, MEPh, SPmax, SPh, and MVC (N = 13). All values are expressed as %mean value
To examine if within-day or across-day protocol affected the EMG measures over the course of four repeated measurements, we fitted a LMM to predict change in those EMG measures with PROTOCOL and SESSION. For Mmax, the model’s total explanatory power was very large (conditional R2 = 0.96), and the part related to the fixed effects alone was very small (marginal R2 = 0.002). The main effect of SESSION (p = 0.48), PROTOCOL (p = 0.24), or PROTOCOL × SESSION interaction (p = 0.32) was not significant. For Hmax, conditional R2 = 0.90 and marginal R2 = 0.007; the effect of SESSION (p = 0.22), PROTOCOL (p = 0.27), or PROTOCOL × SESSION interaction (p = 0.82) was not significant. For MEPmax, conditional R2 = 0.87 and marginal R2 = 0.002; the effect of SESSION (p = 0.44), PROTOCOL (p = 0.99), or PROTOCOL × SESSION interaction (p = 0.47) was not significant. For MEPh, conditional R2 = 0.71 and marginal R2 = 0.036; the effect of SESSION (p = 0.87), PROTOCOL (p = 0.11), or PROTOCOL × SESSION interaction (p = 0.87) was not significant. For SPmax, conditional R2 = 0.68 and marginal R2 = 0.001; the effect of SESSION (p = 0.65), PROTOCOL (p = 0.90), or PROTOCOL × SESSION interaction (p = 0.67) was not significant. For SPh, conditional R2 = 0.68 and marginal R2 = 0.001; the effect of SESSION (p = 0.11), PROTOCOL (p = 0.47), or PROTOCOL × SESSION interaction (p = 0.40) was not significant. For MVC, conditional R2 = 0.83 and marginal R2 = 0.046; the effect of SESSION (p = 0.35), PROTOCOL (p = 0.07), or PROTOCOL × SESSION interaction (p = 0.72) was not significant.
To estimate the extent of within-day and across-day variability, the mean (absolute) deviation across 4 sessions was calculated for each measure, and the values are summarized in Table 3.
Across-day variability in the excitability of corticospinal and spinal pathways in people with SCI
TA Mmax, Hmax, MEPmax, MEPh, SPmax, SPh, and MVC in participants with SCI, across 4 days of measurements are expressed in % mean and presented in Fig. 4. Besides some inter-individual variabilities, there are no obvious systematic increases or decreases across 4 sessions in the measures obtained. Values of the mean deviation across 4 sessions are summarized in Table 3.
Measures of corticospinal and spinal excitability for the tibialis anterior (TA) repeated over 4 different days at approximately the same time of day in participants with chronic incomplete SCI. a–c Peristimulus TA EMG sweeps for the Mmax, Hmax and MEPmax from a single participant. For each sweep ≈ 4 responses are averaged together. The grey/shaded area indicates the time window for which each variable was measured. d–j The mean value across all participants (thick black line) and individual participant values (each line for each participant) for Mmax (N = 17), Hmax (N = 17), MEPmax (N = 8), MEPh (N = 17), SPmax (N = 8), SPh (N = 13), and MVC (N = 17). All values are expressed as % mean value
To examine the trend of variation in the EMG measures over the course of 4 repeated measurements, we fitted a LMM to predict change in those EMG measures with SESSION. For Mmax, the model's total explanatory power was very large (conditional R2 = 0.95), and the part related to the fixed effects alone was small (marginal R2 = 0.001). The effect of SESSION (p = 0.41) was not significant. For Hmax, conditional R2 = 0.99 and marginal R2 = 0.000; the effect of SESSION (p = 0.39) was not significant. For MEPmax, conditional R2 = 0.92 and marginal R2 = 0.000; the effect of SESSION (p = 0.78) was not significant. For MEPh, conditional R2 = 0.98 and marginal R2 = 0.001; the effect of SESSION (p = 0.21) was not significant. For SPmax, conditional R2 = 0.83 and marginal R2 = 0.002; the effect of SESSION (p = 0.56) was not significant. For SPh, conditional R2 = 0.93 and marginal R2 = 0.010; the effect of SESSION (p = 0.09) was not significant. For MVC, conditional R2 = 0.93 and marginal R2 = 0.002; the effect of SESSION (p = 0.21) was not significant.
Discussion
This study aimed to examine the variability and stability of TA corticospinal excitability across repeated measurement sessions in individuals with and without corticospinal lesions. For all 7 EMG measures, which would help to evaluate corticospinal and spinal reflex excitability for TA, calculation of SEM and assessment of CV and ICC suggested generally high reliability and low variability of those measures across 4 repeated experimental sessions. Through LMM analyses, we found no systematic fluctuation in those EMG measures over 4 days or over 12 h within the same day in participants without SCI, and across 4 days in participants with chronic incomplete SCI. Below we discuss implications of those repeatability and variability assessments and the absence of systematic day-to-day or diurnal variability in the measures of TA corticospinal and spinal excitability for the existing and future clinical research studies that investigate corticospinal plasticity.
Repeatability and variability in corticospinal or spinal evoked responses across multiple measurements
In the present study, the mean absolute deviations across four measurements remained in a range of 5–13% in all the corticospinal and spinal excitability measures. In participants without SCI, CVs, which indicate the extent of variability in relation to the mean of the multiple measurements, were 6–19% across 7 different EMG measures. These percentages are in support of limited variability in these measures when the measurements are repeated. The fact that CVs did not differ between the within-day and across-day protocols suggest that the extent of potential diurnal variability in corticospinal and spinal reflex excitability (if present) remains within a day-to-day (or session-to-session) variability range. ICC values, which indicate the repeatability of the measurements, were also high (i.e., ≥ 0.68, often over 0.90) for the present measures, suggesting excellent measurement-to-measurement reliability/reproducibility (Koo and Li 2016) can be achieved in participants without SCI. The present values are in agreement with a couple of existing studies; Palmieri et al. (2002) reported ICC values of 0.78–0.997 for the TA Hmax, Mmax, and Hmax/Mmax ratio, and Tallent et al. (2012) reported ICC values of 0.81–0.94 for TA MEPs across 3 days and ICC values of > 0.66 for TA H-reflex across 3 days during isometric and dynamic muscle contraction. Together with our history of successful long-term repeated (i.e., 30–40 sessions) EMG evoked response measurement studies (Thompson et al. 2009, 2013b, 2018, 2022; Makihara et al. 2014; Mrachacz-Kersting et al. 2019; Thompson and Wolpaw 2019, 2021) and existing studies by the other groups, the present CV and ICC results support that well-maintained experimental setups and stable administration of experimental procedures would lead to low variability and high repeatability of EMG measures across multiple measurement sessions, which in turn would help us assess the presence and extent of physiological changes and plasticity.
In addition, based on the limited measurement-to-measurement variabilities observed in the present study, we may assume that in people with no known neurological conditions, the measures of TA corticospinal and spinal excitability may vary but would remain generally within a ± 15% range across multiple measurement sessions when the experimental conditions are kept the same. Still, the variability in corticospinal and spinal excitability measures would likely be affected by specific methodologies employed in each study; those include (but not limited to) sample size, number of responses averaged together, participants' characteristics, experimental setup (e.g., background EMG feedback vs. force feedback, or active EMG vs. no active EMG), EMG amplifier that affects the signal-to-noise ratio, and so on. Thus, the assessment of TA corticospinal excitability, for example, in response to a neuromodulatory intervention, resulting in small (e.g., less than 15%) changes in EMG evoked response measures, may need to be considered carefully through rigorous statistical and qualitative analyses.
In participants with SCI, CVs were 9–21% across different EMG measures. Within a relatively small range, the CV for Mmax was larger and the CV for MEPh was smaller than that in participants without SCI. Besides the difference in background EMG setting used during these measurements potentially affecting the measurement-to-measurement variability (note that background EMG concerns are discussed further in the section Methodological considerations, limitations, and clinical implications), these differences in CVs may be partly related to the raw amplitude of those measures in individuals with SCI. As shown in Tables 2 and 3, TA Mmax tends to be smaller in mV in participants with SCI than participant without while their SEMs and mean deviations are comparable to those in participants without SCI; these would result in larger CVs in participants with SCI. For MEPh, its smaller CV may be because the entire MEP recruitment curve tends to reside within a narrower range in participants with SCI; that is, because not only MEPh but also MEPmax is small, the range within which MEPh can fluctuate would naturally be limited. As a result, the CV for MEPh would be small (and so as SEM and mean deviation). It should be noted that despite its statistical difference from non-SCI, the CV for Mmax in participant with SCI is 10% (and mean deviation is 7%) on average, and thus, the physiological significance of such a limited extent of variability is not clear. For the MEPh, it is also not clear if the CV of 9% (and mean deviation of 6%) implies anything positive or negative in terms of how the corticospinal pathway functions in this population. In participants with SCI, ICC values were all high (i.e., 0.90–0.98 except for 0.75 in SPmax), suggesting excellent measurement-to-measurement reproducibility (Koo and Li 2016) for the TA EMG measures in people with SCI.
Absence of the effects of repeated measurements either within-day or across days
In individuals with no known neurological conditions, the present LMM analyses yielded no effects of SESSION, indicating that there were no systematic fluctuations across four time points of measurements in any of the EMG measures that reflect corticospinal or spinal reflex excitability. This implies two things. First, repeating the same measurements four times with 3+ h intervals (i.e., within-day protocol) or > 23-h intervals do not produce systematic effects on the EMG measures that were obtained in this study. Second, the corticospinal or spinal reflex excitability for the TA would not vary systematically within or across days (over four measurement sessions).
In individuals with chronic incomplete SCI, LMM analyses on the session-to-session across-day variability in the EMG measures of TA corticospinal and spinal excitability exhibited no systematic changes across measurements, similarly to the findings in individuals with no known neurological conditions. This further indicates that in individuals with SCI who are medically stable and in good health, partial damage to the spinal cord does not necessarily create some unknown cumulative effects of four repeated measurements with > 23-h intervals.
Note that the extent of session-to-session variability appeared less for Mmax than other measures in individuals with no known neurological conditions (Figs. 2 and 3 and Table 3). This was expected, because Mmax is from stimulating all motor axons (Pierrot-Deseilligny and Burke 2012), its values would not be affected by the motoneuron pool excitability or synaptic input converging onto motoneurons. Therefore, the stability of Mmax supports the reproducibility of experimental setup across multiple experiments. In contrast, the H-reflex and MEP are from transsynaptic excitation of motoneurons, and thus, would reflect the above factors and presynaptic mechanisms that influence the efficacy of synaptic input onto motoneurons (Capaday and Stein 1987; Stein 1995). In the present study, because the experiments were set up to keep the task, posture, and ongoing EMG activity consistent across different MEP and H-reflex measurements, the session-to-session variability in motoneuron pool excitability and task- and posture-dependent pre- and postsynaptic inhibition was presumably minimum. Interpretation of the resulting variability could, therefore, be about what was measured and when. We found no consistent changes in magnitude and/or pattern, for the measures of corticospinal excitability (i.e., MEPmax and MEPh), spinal reflex excitability (i.e., Hmax), and cortical (at least partly) inhibition (i.e., SPmax and SPh), across 4 days (in individuals with or without SCI) or over 12 h period (in individuals without SCI) for the ankle dorsiflexor TA; and none varied more (or less) or systematically when the same measurements are simply repeated multiple times.
Absence of clear diurnal variation in the corticospinal and spinal excitability for the TA
In this study, we did not observe any diurnal variation in the corticospinal or spinal reflex excitability of the TA in individuals with no known neurological conditions. To our knowledge, this is the first study to look at diurnal variation in the TA. Previous studies have shown diurnal variation exists in the corticospinal excitability (Tamm et al. 2009) and H-reflex amplitude (Lagerquist et al. 2006) of other muscles (e.g., the triceps surae). This suggests that diurnal variation in the corticospinal and spinal excitability is not a universal phenomenon across leg muscles. This was somewhat unexpected since diurnal rhythms exist in multiple physiological processes throughout the human body, including body temperature (Aschoff 1983; Refinetti and Menaker 1992), blood pressure and heart rate (Millar-Craig et al. 1978; Weber et al. 1984; Degaute et al. 1991), hormonal regulation (Bailey and Heitkemper 2001), sleep/wake cycle (Santhi et al. 2016), and torque/force production (Freivalds et al. 1983; Gauthier et al. 1996, 2001; Martin et al. 1999; Guette et al. 2005b; Lagerquist et al. 2006; Sedliak et al. 2008; Andrews et al. 2010; Hodge et al. 2019; Douglas et al. 2021). The effect of diurnal rhythm on these measures can further be influenced by chronotype (Tamm et al. 2009), gender (Duffy et al. 2011; Santhi et al. 2016), and age (Silva et al. 2021). In particular, voluntary maximal and submaximal isometric force production has been reported to increase throughout the day in several different muscles, such as triceps surae (Castaingts et al. 2004; Guette et al. 2005a, 2006; Lagerquist et al. 2006), quadriceps femoris (Callard et al. 2000; Guette et al. 2005b; Sedliak et al. 2008), biceps brachii (Freivalds et al. 1983; Gauthier et al. 1997, 2001), and adductor pollicis (Martin et al. 1999). At the same time, the extent of diurnal variation in EMG activity during isometric force production could differ even among synergist muscles (Tamm et al. 2009). In a recent review, Douglas et al. (2021) suggested that time of day difference in muscle strength could be a circadian rhythm linked to intrinsic muscle properties such as myosin type and calcium and/or kinase regulation that would affect contractile proteins (Zhi 2005; Andrews et al. 2010; Schroder et al. 2015; Perrin et al. 2018; Hodge et al. 2019; Altıntaş et al. 2020; Swist et al. 2020), rather than neural activation and drive or extrinsic factors such as temperature or wakefulness (Gauthier et al. 1996; Martin et al. 1999; Nicolas et al. 2008; Sedliak et al. 2008; Gueldich et al. 2017). The present study's observations are in line with this view; EMG activity during MVC and the corticospinal and spinal excitability did not exhibit systematic changes throughout the day (i.e., not beyond random variations), leaving the intrinsic muscle property change as a possible mechanism of force production increase throughout the day.
This brings us to the question of why and how diurnal variations in the corticospinal and spinal excitability appear differently between the soleus/triceps surae (Lagerquist et al. 2006; Tamm et al. 2009) and TA (i.e., present study). In the soleus, diurnal rhythms exist both for the corticospinal and spinal excitability (Wolpaw et al. 1984; Chen and Wolpaw 1994; Carp et al. 2006a; Lagerquist et al. 2006; Tamm et al. 2009). In rats, Chen et al. (2002) showed that transection of the corticospinal tract (CST), not lateral column or dorsal column, results in reduction of rhythm amplitude and phase, implying that the soleus H-reflex diurnal rhythm depends on the CST activity that reflects descending drive from sensory and motor-related areas of the cortex. In humans, diurnal rhythms in the soleus corticospinal excitability are observed with chronotypes (Tamm et al. 2009), i.e., the corticospinal excitability is high in the AM in the morning people and high in the PM in the evening people. In parallel, the soleus H-reflex excitability increases throughout the day, regardless of chronotype (Lagerquist et al. 2006; Tamm et al. 2009). These observations are different from the present ones, which showed no systematic increases or decreases in TA MVC, H-reflex, and MEP measures made over a course of 12 h within-day. The difference in the strength of cortical or corticospinal drive may partially explain this TA − soleus difference. Bawa et al. (2002) showed the existence of corticomotoneuronal connections for both the soleus and TA, with more prominent connection for the TA compared to the soleus. Differing strengths in corticospinal drive between these two muscles have also been demonstrated in other studies (Advani and Ashby 1990; Brouwer and Ashby 1992). Thus, it is theoretically possible that in the muscle that is largely controlled by abundant corticospinal drive, relatively small diurnal variations in the drive may be obscured by its random variations and not be readily detectable in EMG measures.
Methodological considerations, limitations, and clinical implications
In the present study, we used the custom-made batwing coil, which was originally designed to stimulate the leg motor areas of the cortex more effectively than the standard figure-of-8 coil and more focal than the double-cone coil (although the produced electric field might not penetrate deep into the lower leg motor area as effectively as the double-cone coil). While the batwing coil has been used successfully in a number of studies (Barthelemy et al. 2011; Needle et al. 2013; Palmer et al. 2016, 2017a, b; Cai et al. 2012), since the created electric fields would differ between different coil designs, whether and to what extent the current findings with the batwing coil may be replicated with the double-cone coil stimulation are yet to be determined.
In the present study, the TA background EMG levels differed between neurologically normal participants and participants with SCI for Mmax and Hmax measurements (≈ 15% MVC level in non-SCI vs. at rest in SCI) and for MEP measurements (≈ 15% MVC level in non-SCI vs. ≈ 30% MVC level in SCI). Such methodological limitations warrant further consideration in interpreting the data. In this study, we prioritized on measuring MEPs that reflect corticospinal excitability while background EMG was actively controlled so that the motoneuron pool’s excitability could be controlled during the measurements. (Note that eliciting MEPs at rest is possible, but at rest, we could never be certain of the subthreshold level of motoneuron pool’s excitability, which would affect MEPs.) To consider potential concurrent systematic fluctuations in the excitability of corticospinal and spinal reflex pathways, ideally EMG measures to peripheral nerve stimulation should also be made during the same level of background EMG activation as MEP elicitation. However, since it was difficult for many of the current study participants with chronic incomplete SCI (with weak dorsiflexion) to go through many trials with the controlled amount of active background EMG, we elected to drop the H-reflex measurement with active EMG in this group. Admittedly, this resulted in measuring H-reflexes with uncontrolled variability in the subthreshold level of motoneuron pool’s excitability, and thus, the present H-reflex measurements in SCI are not immediately relatable to the variability in MEP amplitude across repeated measurement sessions. Mmax, on the other hand, would still serve as an estimate of the response of the entire motoneuron pool (that can be recorded with the specific EMG electrode configuration that is used); and as long as the posture, skin preparation, and electrode positions are consistent, Mmax should be comparable between the measurements and could help to explain potential variations in MEP amplitude. Indeed, the present data (i.e., low CVs and high ICCs) support our confidence in within-participant measurement repeatability, for a give participant and for a given protocol/participant group. That being said, we are aware that the SCI vs. non-SCI comparisons (i.e., comparisons of CVs) are not ideal. Difference in background EMG activity levels could have affected the assessment of session-to-session variability in MEP and H-reflex measures. To our knowledge, whether and to what extent different levels of active background EMG may affect session-to-session variability in MEP measures is currently unknown. Despite such uncertainties, the present study found the session-to-session variability of these measures within a quite reasonable range in participants with SCI.
In this study, we examined the measurement-to-measurement variability in the TA corticospinal and spinal excitability measures in individuals without known neurological conditions across 4 time points within the same day and across 4 days (at the same time of day). By examining the extent and pattern of variability in two different timelines, we hoped to differentiate any potential effect of repeated measurements from a potential diurnal effect on corticospinal and spinal excitability measures if one existed at all. Here we observed no clear effect of repeated measures either over 12 h or across days, with the magnitude of variations being similar within and across days. Because we performed these examinations only in individuals without injuries, some may wonder why we did not do the same in individuals with SCI. It is important to note that in individuals with chronic SCI, examining whether and to what extent the diurnal variation may exist would most likely be meaningless. Many of those individuals are on chronic daily medication and medication effects would not be the same throughout day. Thus, estimating (and accounting for) changes in medication effectiveness throughout day for each individual and across different individuals would not be possible in reality. Since this study did not find diurnal variation in the corticospinal and spinal excitability for TA of the intact CNS, an implication of this for neurorehabilitation is that there is no specific time of day that is neurophysiological optimum for rehabilitation therapy involving TA dysfunction (e.g., therapy aiming to alleviate foot drop). What might be more important in therapy administration is to maintain the intervention/training schedule in relation to daily chronic medication regimens.
Variability will always exist in human neurophysiology and thus in experimental measures. Therefore, knowing what a normal range of variability in a given measure (including the variability introduced by human experimenters) can help to detect neurophysiological changes that are beyond random variations and attributable to a therapeutic protocol or intervention. What this study provides are some reference values as to how much the TA corticospinal and spinal excitability measures may vary in people of stable health with and without chronic incomplete SCI.
Conclusion
In this study, we examined whether session-to-session variability existed in corticospinal and spinal excitability for the ankle dorsiflexor TA in people with and without incomplete SCI. We found no clear diurnal variation in the measures of spinal and corticospinal excitability of the TA in individuals with no known neurological conditions, and no systematic changes in any experimental measures of spinal and corticospinal excitability across four measurement days in individuals with or without SCI. This study demonstrates that it is possible to repeatedly measure the corticospinal and spinal evoked responses for the TA with stability in people of stable health with or without chronic SCI. This supports the utility of corticospinal and spinal excitability measures in mechanistic investigation of neuromodulation interventions. While systematic variation of corticospinal excitability was not found for the TA, considering complex diurnal variations in multiple human physiological processes and possible effects of daily scheduled medication, the consistency in the time of day to administer an intervention remains essential for scientific integrity and therapeutic efficacy in long-term rehabilitation studies in people with SCI and other neuromuscular disorders.
Data availability
Study data are available upon request.
References
Advani A, Ashby P (1990) Corticospinal control of soleus motoneurons in man. Can J Physiol Pharmacol 68:1231–1235
Altıntaş A, Laker RC, Garde C, Barres R, Zierath JR (2020) Transcriptomic and epigenomics atlas of myotubes reveals insight into the circadian control of metabolism and development. Epigenomics 12:701–713
Andrews JL, Zhang X, McCarthy JJ et al (2010) CLOCK and BMAL1 regulate MyoD and are necessary for maintenance of skeletal muscle phenotype and function. Proc Natl Acad Sci 107:19090–19095
Aschoff J (1983) Circadian control of body temperature. J Thermal Biol 8:143–147
Bailey SL, Heitkemper MM (2001) Circadian rhythmicity of cortisol and body temperature: morningness-eveningness effects. Chronobiol Int 18:249–261
Barthelemy D, Willerslev-Olsen M, Lundell H, Conway BA, Knudsen H, Biering-Sorensen F, Nielsen JB (2010) Impaired transmission in the corticospinal tract and gait disability in spinal cord injured persons. J Neurophysiol 104:1167–1176. https://doi.org/10.1152/jn.00382.2010
Barthelemy D, Grey MJ, Nielsen JB, Bouyer L (2011) Involvement of the corticospinal tract in the control of humangait. Prog Brain Res 192:181–197
Bates D, Maechler M, Bolker B, Walker S (2015) Fitting Linear Mixed-Effects Models Using lme4. J Statistical Software 67(1):1–48. https://doi.org/10.18637/jss.v067.i01
Bawa P, Chalmers GR, Stewart H, Eisen AA (2002) Responses of ankle extensor and flexor motoneurons to transcranial magnetic stimulation. J Neurophysiol 88:124–132
Brouwer B, Ashby P (1992) Corticospinal projections to lower limb motoneurons in man. Exp Brain Res 89:649–654
Butefisch CM, Davis BC, Wise SP, Sawaki L, Kopylev L, Classen J, Cohen LG (2000) Mechanisms of use-dependent plasticity in the human motor cortex. Proc Natl Acad Sci 97:3661–3665
Cai W, George JS, Chambers CD, Stokes MG, Verbruggen F, Aron AR (2012) Stimulating deep cortical structures with the batwing coil: How to determine the intensity for transcranial magnetic stimulation using coil–cortex distance. J Neurosci Methods 204:238–241
Callard D, Davenne D, Gauthier A, Lagarde D, Van Hoecke J (2000) Circadian rhythms in human muscular efficiency: continuous physical exercise versus continuous rest. A crossover study. Chronobiol Int 17:693–704
Capaday C, Stein RB (1987) A method for simulating the reflex output of a motoneuron pool. J Neurosci Methods 21:91–104
Capaday C, Lavoie BA, Barbeau H, Schneider C, Bonnard M (1999) Studies on the corticospinal control of human walking. I. Responses to focal transcranial magnetic stimulation of the motor cortex. J Neurophysiol 81:129–139
Carp JS, Tennissen AM, Chen XY, Wolpaw JR (2006a) Diurnal H-reflex variation in mice. Exp Brain Res 168:517–528. https://doi.org/10.1007/s00221-005-0106-y
Carp JS, Tennissen AM, Chen XY, Wolpaw JR (2006b) H-reflex operant conditioning in mice. J Neurophysiol 96:1718–1727. https://doi.org/10.1152/jn.00470.2006
Castaingts V, Martin A, Van Hoecke J, Perot C (2004) Neuromuscular efficiency of the triceps surae in induced and voluntary contractions: morning and evening evaluations. Chronobiol Int 21:631–643
Chen XY, Wolpaw JR (1994) Circadian rhythm in rat H-reflex. Brain Res 648:167–170
Chen XY, Wolpaw JR (1995) Operant conditioning of H-reflex in freely moving rats. J Neurophysiol 73:411–415
Chen XY, Chen L, Wolpaw JR, Jakeman LB (2002) Corticospinal tract transection reduces H-reflex circadian rhythm in rats. Brain Res 942:101–108
Classen J, Liepert J, Wise SP, Hallett M, Cohen LG (1998) Rapid plasticity of human cortical movement representation induced by practice. J Neurophysiol 79:1117–1123
Davey NJ, Smith HC, Savic G, Maskill DW, Ellaway PH, Frankel HL (1999) Comparison of input-output patterns in the corticospinal system of normal subjects and incomplete spinal cord injured patients. Exp Brain Res 127:382–390
Degaute J-P, Van De Borne P, Linkowski P, Van Cauter E (1991) Quantitative analysis of the 24-hour blood pressure and heart rate patterns in young men. Hypertension 18:199–210
Devanne H, Lavoie BA, Capaday C (1997) Input-output properties and gain changes in the human corticospinal pathway. Exp Brain Res 114:329–338
Douglas CM, Hesketh SJ, Esser KA (2021) Time of day and muscle strength: a circadian output? Physiology (bethesda) 36:44–51. https://doi.org/10.1152/physiol.00030.2020
Duffy JF, Cain SW, Chang A-M et al (2011) Sex difference in the near-24-hour intrinsic period of the human circadian timing system. Proc Natl Acad Sci 108:15602–15608
Everaert DG, Thompson AK, Chong SL, Stein RB (2010) Does functional electrical stimulation for foot drop strengthen corticospinal connections? Neurorehabil Neural Repair 24:168–177
Freivalds A, Chaffin DB, Langolf GD (1983) Quantification of human performance circadian rhythms. Am Ind Hygiene Assoc 44:643–648
Gamer M, Lemon J, Fellows I, Singh P (2019) IFPS_irr: various coefficients of interrater reliability and agreement. R package version 0.84.1. https://CRAN.R-project.org/package=irr
Garvey MA, Ziemann U, Becker DA, Barker CA, Bartko JJ (2001) New graphical method to measure silent periods evoked by transcranial magnetic stimulation. Clin Neurophysiol 112:1451–1460
Gauthier A, Davenne D, Martin A, Cometti G, Hoecke JV (1996) Diurnal rhythm of the muscular performance of elbow flexors during isometric contractions. Chronobiol Int 13:135–146
Gauthier A, Davenne D, Gentil C, Hoecke JV (1997) Orcadian rhythm in the torque developed by elbow flexors during isometric contraction effect of sampling schedules. Chronobiol Int 14:287–294
Gauthier A, Davenne D, Martin A, Van Hoecke J (2001) Time of day effects on isometric and isokinetic torque developed during elbow flexion in humans. Eur J Appl Physiol 84:249–252
Ghanavatian S, Derian A (2022) Tizanidine. In: StatPearls. StatPearls Publishing, TreasureIsland
Green P, MacLeod CJ (2016) simr: an R package for power analysis of generalised linear mixed models by simulation. Methods Ecol Evol 7(4):493–498. https://doi.org/10.1111/2041-210X.12504
Gueldich H, Zarrouk N, Chtourou H, Zghal F, Sahli S, Rebai H (2017) Electrostimulation training effects on diurnal fluctuations of neuromuscular performance. Int J Sports Med 38:41–47
Guette M, Gondin J, Martin A (2005a) Morning to evening changes in the electrical and mechanical properties of human soleus motor units activated by H reflex and M wave. Eur J Appl Physiol 95:377–381
Guette M, Gondin J, Martin A (2005b) Time-of-day effect on the torque and neuromuscular properties of dominant and non-dominant quadriceps femoris. Chronobiol Int 22:541–558
Guette M, Gondin J, Martin A, Pérot C, Van Hoecke J (2006) Plantar flexion torque as a function of time of day. Int J Sports Med 27:171–177
Hodge BA, Zhang X, Gutierrez-Monreal MA et al (2019) MYOD1 functions as a clock amplifier as well as a critical co-factor for downstream circadian gene expression in muscle. Elife 8:e43017
Karni A, Meyer G, Rey-Hipolito C, Jezzard P, Adams MM, Turner R, Ungerleider LG (1998) The acquisition of skilled motor performance: fast and slow experience-driven changes in primary motor cortex. Proc Natl Acad Sci 95:861–868
Kido A, Tanaka N, Stein RB (2004a) Spinal excitation and inhibition decrease as humans age. Can J Physiol Pharmacol 82:238–248
Kido A, Tanaka N, Stein RB (2004b) Spinal reciprocal inhibition in human locomotion. J Appl Physiol 96:1969–1977
Kido Thompson A, Stein RB (2004) Short-term effects of functional electrical stimulation on motor-evoked potentials in ankle flexor and extensor muscles. Exp Brain Res 159:491–500
Knash ME, Kido A, Gorassini M, Chan KM, Stein RB (2003) Electrical stimulation of the human common peroneal nerve elicits lasting facilitation of cortical motor-evoked potentials. Exp Brain Res 153:366–377
Koo T, Li M (2016) Cracking the code: providing insight into the fundamentals of research and evidence-based practice a guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Lagerquist O, Zehr EP, Baldwin ER, Klakowicz PM, Collins DF (2006) Diurnal changes in the amplitude of the Hoffmann reflex in the human soleus but not in the flexor carpi radialis muscle. Exp Brain Res 170:1–6. https://doi.org/10.1007/s00221-005-0172-1
Liepert J, Bauder H, Wolfgang HR, Miltner WH, Taub E, Weiller C (2000a) Treatment-induced cortical reorganization after stroke in humans. Stroke 31:1210–1216
Liepert J, Graef S, Uhde I, Leidner O, Weiller C (2000b) Training-induced changes of motor cortex representations in stroke patients. Acta Neurol Scand 101:321–326
Makihara Y, Segal RL, Wolpaw JR, Thompson AK (2014) Operant conditioning of the soleus H-reflex does not induce long-term changes in the gastrocnemius H-reflexes and does not disturb normal locomotion in humans. J Neurophysiol 112:1439–1446. https://doi.org/10.1152/jn.00225.2014
Martin A, Carpentier A, Guissard N, Van Hoecke J, Duchateau J (1999) Effect of time of day on force variation in a human muscle. Muscle Nerve 22:1380–1387
McGraw KO, Wong SP (1996) Forming Inferences about Some Intraclass Correlation Coefficients. Psychol Methods 1:30–46. https://doi.org/10.1037/1082-989X.1.1.30
Millar-Craig M, Bishop C, Raftery E (1978) Circadian variation of blood-pressure. Lancet 311:795–797
Mrachacz-Kersting N, Kersting UG, de Brito SP, Makihara Y, Arendt-Nielsen L, Sinkjaer T, Thompson AK (2019) Acquisition of a simple motor skill: task-dependent adaptation and long-term changes in the human soleus stretch reflex. J Neurophysiol 122:435–446. https://doi.org/10.1152/jn.00211.2019
Needle AR, Palmer JA, Kesar TM, Binder-Macleod SA, Swanik CB (2013) Brain regulation of muscle tone in healthy and functionally unstable ankles. J Sport Rehabil 22:202–211
Nicolas A, Gauthier A, Bessot N, Moussay S, Thibault G, Sesboüé B, Davenne D (2008) Effect of time-of-day on neuromuscular properties of knee extensors after a short exhaustive cycling exercise. Isokinetics Exer Sci 16:33–40
Nudo RJ (2003) Adaptive plasticity in motor cortex: implications for rehabilitation after brain injury. J Rehabil Med 35:7–10
Palmer JA, Needle AR, Pohlig RT, Binder-Macleod SA (2016) Atypical cortical drive during activation of the paretic and nonparetic tibialis anterior is related to gait deficits in chronic stroke. Clin Neurophysiol 127:716–723
Palmer JA, Hsiao H, Wright T, Binder-Macleod SA (2017a) Single session of functional electrical stimulation-assisted walking produces corticomotor symmetry changes related to changes in poststroke walking mechanics. Phys Ther 97:550–560
Palmer JA, Zarzycki R, Morton SM, Kesar TM, Binder-Macleod SA (2017b) Characterizing differential poststroke corticomotor drive to the dorsi-and plantarflexor muscles during resting and volitional muscle activation. J Neurophysiol 117:1615–1624
Palmieri RM, Hoffman MA, Ingersoll CD (2002) Intersession reliability for H-reflex measurements arising from the soleus, peroneal, and tibialis anterior musculature. Int J Neurosci 112:841–850
Pascual-Leone A, Davey NJ, Rothwell J, Wassermann EM, Puri BK (2002) Handbook of transcranial magnetic stimulation. Arnold, a member of the Hodder Headline Group, London
Perrin L, Loizides-Mangold U, Chanon S et al (2018) Transcriptomic analyses reveal rhythmic and CLOCK-driven pathways in human skeletal muscle. Elife 7:e34114
Petersen NT, Butler JE, Marchand-Pauvert V et al (2001) Suppression of EMG activity by transcranial magnetic stimulation in human subjects during walking. J Physiol 537:651–656
Pierrot-Deseilligny E, Burke D (2012) The circuitry of the human spinal cord: spinal and corticospinal mechanisms of movement. Cambridge University Press, Cambridge
R Core Team (2023) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org
Ramanathan D, Conner JM, Tuszynski MH (2006) A form of motor cortical plasticity that correlates with recovery of function after brain injury. Proc Natl Acad Sci 103:11370–11375
Refinetti R, Menaker M (1992) The circadian rhythm of body temperature. Physiol Behav 51:613–637
Ridding MC, Rothwell JC (1997) Stimulus/response curves as a method of measuring motor cortical excitability in man. Electroencephalogr Clin Neurophysiol 105:340–344
Rioult-Pedotti MS, Friedman D, Donoghue JP (2000) Learning-induced LTP in neocortex. Science 290:533–536
Rossini PM, Barker A, Berardelli A et al (1994) Non-invasive electrical and magnetic stimulation of the brain, spinal cord, and roots: basic principles and procedures for routine clinical application. Report of an IFCN committee. Electroencephalogr Clin Neurophysiol 91:79–92
Santhi N, Lazar AS, McCabe PJ, Lo JC, Groeger JA, Dijk D-J (2016) Sex differences in the circadian regulation of sleep and waking cognition in humans. Proc Natl Acad Sci 113:E2730–E2739
Schroder EA, Harfmann BD, Zhang X et al (2015) Intrinsic muscle clock is necessary for musculoskeletal health. J Physiol 593:5387–5404
Schubert M, Curt A, Jensen L, Dietz V (1997) Corticospinal input in human gait: modulation of magnetically evoked motor responses. Exp Brain Res 115:234–246
Schubert M, Curt A, Colombo G, Berger W, Dietz V (1999) Voluntary control of human gait: conditioning of magnetically evoked motor responses in a precision stepping task. Exp Brain Res 126:583–588
Sedliak M, Finni T, Peltonen J, Häkkinen K (2008) Effect of time-of-day-specific strength training on maximum strength and EMG activity of the leg extensors in men. J Sports Sci 26:1005–1014
Siebner HR, Rothwell J (2003) Transcranial magnetic stimulation: new insights into representational cortical plasticity. Exp Brain Res 148:1–16
Silva BSdA, Uzeloto JS, Lira FS, Pereira T, Coelho-E-Silva MJ, Caseiro A (2021) Exercise as a peripheral circadian clock resynchronizer in vascular and skeletal muscle aging. Int J Environ Res Pub Health 18:12949
Stein RB (1995) Presynaptic inhibition in humans. Prog Neurobiol 47:533–544
Swist S, Unger A, Li Y et al (2020) Maintenance of sarcomeric integrity in adult muscle cells crucially depends on Z-disc anchored titin. Nat Commun 11:1–18
Tallent J, Goodall S, Hortobagyi T, St Clair Gibson A, French DN, Howatson G (2012) Repeatability of corticospinal and spinal measures during lengthening and shortening contractions in the human tibialis anterior muscle. PLoS ONE 7:e35930. https://doi.org/10.1371/journal.pone.0035930
Tamm AS, Lagerquist O, Ley AL, Collins DF (2009) Chronotype influences diurnal variations in the excitability of the human motor cortex and the ability to generate torque during a maximum voluntary contraction. J Biol Rhythms 24:211–224. https://doi.org/10.1177/0748730409334135
Thomas SL, Gorassini MA (2005) Increases in corticospinal tract function by treadmill training after incomplete spinal cord injury. J Neurophysiol 94:2844–2855
Thompson AK, Sinkjaer T (2020) Can operant conditioning of EMG-evoked responses help to target corticospinal plasticity for improving motor function in people with multiple sclerosis? Front Neurol 11:552. https://doi.org/10.3389/fneur.2020.00552
Thompson AK, Wolpaw JR (2021) H-reflex conditioning during locomotion in people with spinal cord injury. J Physiol 599:2453–2469. https://doi.org/10.1113/JP278173
Thompson AK, Doran B, Stein RB (2006) Short-term effects of functional electrical stimulation on spinal excitatory and inhibitory reflexes in ankle extensor and flexor muscles. Exp Brain Res 170:216–226
Thompson AK, Chen XY, Wolpaw JR (2009) Acquisition of a simple motor skill: task-dependent adaptation plus long-term change in the human soleus H-reflex. J Neurosci 29:5784–5792. https://doi.org/10.1523/JNEUROSCI.4326-08.2009
Thompson AK, Lapallo B, Duffield M, Abel BM, Pomerantz F (2011) Repetitive common peroneal nerve stimulation increases ankle dorsiflexor motor evoked potentials in incomplete spinal cord lesions. Exp Brain Res 210:143–152. https://doi.org/10.1007/s00221-011-2607-1
Thompson AK, Chen XY, Wolpaw JR (2013a) Soleus H-reflex operant conditioning changes the H-reflex recruitment curve. Muscle Nerve 47:539–544. https://doi.org/10.1002/mus.23620
Thompson AK, Pomerantz FR, Wolpaw JR (2013b) Operant conditioning of a spinal reflex can improve locomotion after spinal cord injury in humans. J Neurosci 33:2365–2375. https://doi.org/10.1523/JNEUROSCI.3968-12.2013
Thompson AK, Favale BM, Velez J, Falivena P (2018) Operant up-conditioning of the tibialis anterior motor-evoked potential in multiple sclerosis: feasibility case studies. Neural Plast 2018:4725393. https://doi.org/10.1155/2018/4725393
Thompson AK, Fiorenza G, Smyth L, Favale B, Brangaccio J, Sniffen J (2019) Operant conditioning of the motor-evoked potential and locomotion in people with and without chronic incomplete spinal cord injury. J Neurophysiol 121:853–866. https://doi.org/10.1152/jn.00557.2018
Thompson AK, Gill CR, Feng W, Segal RL (2022) Operant down-conditioning of the soleus H-reflex in people afterstroke. Frontiers Rehabil Sci 3:859724
Urbin MA, Ozdemir RA, Tazoe T, Perez MA (2017) Spike-timing-dependent plasticity in lower-limb motoneurons after human spinal cord injury. J Neurophysiol 118:2171–2180. https://doi.org/10.1152/jn.00111.2017
Weber MA, Drayer JI, Nakamura DK, Wyle FA (1984) The circadian blood pressure pattern in ambulatory normal subjects. The Am J Cardiol 54:115–119
Wirth B, van Hedel HJ, Curt A (2008a) Ankle paresis in incomplete spinal cord injury: relation to corticospinal conductivity and ambulatory capacity. J Clin Neurophysiol 25:210–217. https://doi.org/10.1097/WNP.0b013e318183f4e300004691-200808000-00005[pii]
Wirth B, van Hedel HJ, Kometer B, Dietz V, Curt A (2008b) Changes in activity after a complete spinal cord injury as measured by the spinal cord independence measure II (SCIM II). Neurorehabil Neural Repair 22:145–153. https://doi.org/10.1177/1545968307306240
Wolpaw JR (1987) Operant conditioning of primate spinal reflexes: the H-reflex. J Neurophysiol 57:443–459
Wolpaw JR, Noonan PA, O’Keefe JA (1984) Adaptive plasticity and diurnal rhythm in the primate spinal stretch reflex are independent phenomena. Brain Res 300:385–391
Zhi G (2005) Ryder JW, Huang J, Ding P, Chen Y, Zhao Y, Kamm KE, Stull JT. Myosin light chain kinase and myosin phosphorylation effect frequency-dependent potentiation of skeletal muscle contraction. Proc Natl Acad Sci USA 102:17519–17524
Ziemann U (2004) LTP-like plasticity in human motor cortex. Suppl Clin Neurophysiol 57:702–707
Ziemann U, Ilic TV, Pauli C, Meintzschel F, Ruge D (2004) Learning modifies subsequent induction of long-term potentiation-like and long-term depression-like plasticity in human motor cortex. J Neurosci 24:1666–1672. https://doi.org/10.1523/JNEUROSCI.5016-03.200
Ziemann U, Ilic TV, Jung P (2006) Long-term potentiation (LTP)-like plasticity and learning in human motor cortex–investigations with transcranial magnetic stimulation (TMS). Suppl Clin Neurophysiol 59:19–25
Acknowledgements
We thank Drs. Jonathan R. Wolpaw, James JS Norton, and Russell L. Hardesty for helpful comments on the manuscript. Ms. Gina Fiorenza and Mr. Alex J. Amsterdam for assistance in data analysis. This work was supported in part by the National Institute of Neurological Disorders and Stroke [NS069551 and NS114279 to AKT], the Morton Cure Paralysis Fund to AKT, South Carolina Spinal Cord Injury Research Fund [SCIRF #2019 PD-01 and #2021 PD-01 to AKT], the National Institute of Biomedical Imaging and Bioengineering [P41-EB018783 to Wolpaw], and the Eunice Kennedy Shriver National Institute of Child Health and Human Development [P2C HD086844 to Kautz].
Author information
Authors and Affiliations
Contributions
JAB and AKT conceived the study. JAB and AKT were responsible for the design. JAB, JS, AMP, and AKT performed the experiments. JAB, AKT, and DEG performed the analysis. JAB, JS, AMP, DEG, and AKT interpreted the results. JAB drafted the manuscript. JAB, JS, AMP, DEG, and AKT edited the manuscript. All authors approved the final version submitted and are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
Communicated by Bill J Yates.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brangaccio, J.A., Phipps, A.M., Gemoets, D.E. et al. Variability of corticospinal and spinal reflex excitability for the ankle dorsiflexor tibialis anterior across repeated measurements in people with and without incomplete spinal cord injury. Exp Brain Res 242, 727–743 (2024). https://doi.org/10.1007/s00221-024-06777-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-024-06777-z