Abstract
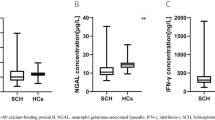
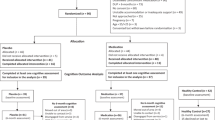
This study aimed to investigate the association between serum prolactin levels and psychiatric symptoms and cognitive function in drug-naïve schizophrenia patients. The study recruited 91 drug-naïve schizophrenia patients and 67 healthy controls. Sociodemographic and clinical data were collected, and cognitive function was assessed using the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) Consensus Cognitive Battery (MCCB). Serum prolactin levels were measured, and statistical analyses were performed to examine the relationship between prolactin levels, clinical symptoms, and cognitive function. The study found that drug-naïve schizophrenia patients had severe cognitive deficits compared to healthy controls across all seven domains of the MCCB. However, no correlation was found between these patients’ serum prolactin levels and clinical severity or cognitive function. The drug-naïve schizophrenia patients had significant cognitive deficits compared to healthy controls. However, there was no significant relationship between prolactin levels and symptomatology and cognition in drug-naïve schizophrenia patients.

Similar content being viewed by others
Data availability
The data used in this study are not publicly available.
References
Aringhieri S et al (2018) Molecular targets of atypical antipsychotics: from mechanism of action to clinical differences. Pharmacol Ther 192:20–41
Brisman MH, Fetell MR, Post KD (1993) Reversible dementia due to macroprolactinoma. Case report. J Neurosurg 79(1):135–137
Degl’Innocenti A et al (1999) The influence of prolactin response to d-fenfluramine on executive functioning in major depression. Biol Psychiatry 46(4):512–517
Fan F et al (2019) Subcortical structures and cognitive dysfunction in first episode schizophrenia. Psychiatry Res Neuroimaging 286:69–75
Fitzgerald P, Dinan TG (2008) Prolactin and dopamine: what is the connection? A review article. J Psychopharmacol 22(2 Suppl):12–19
García RR, Aliste F, Soto G (2018) Social cognition in schizophrenia: cognitive and neurobiological aspects. Rev Colomb Psiquiatr (engl Ed) 47(3):170–176
Hagi K et al (2021) Association between cardiovascular risk factors and cognitive impairment in people with schizophrenia: a systematic review and meta-analysis. JAMA Psychiat 78(5):510–518
Havelka D et al (2016) Cognitive impairment and cortisol levels in first-episode schizophrenia patients. Stress 19(4):383–389
Herceg M et al (2020) Correlation between prolactin and symptom profile in acute admitted women with recurrent schizophrenia. Psychiatr Danub 32(3–4):367–372
Ittig S et al (2017) Sex differences in prolactin levels in emerging psychosis: indication for enhanced stress reactivity in women. Schizophr Res 189:111–116
Jones AS et al (2021) Prolactin ordering patterns in psychiatric inpatients and the impact this has on patient management. Australas Psychiatry 29(3):282–285
Jose J et al (2015) Association between prolactin and thyroid hormones with severity of psychopathology and suicide risk in drug free male schizophrenia. Clin Chim Acta 444:78–80
Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13(2):261–276
Labad J (2019) The role of cortisol and prolactin in the pathogenesis and clinical expression of psychotic disorders. Psychoneuroendocrinology 102:24–36
Lim K et al (2021) Large-scale evaluation of the Positive and Negative Syndrome Scale (PANSS) symptom architecture in schizophrenia. Asian J Psychiatr 62:102732
Marken PA, Haykal RF, Fisher JN (1992) Management of psychotropic-induced hyperprolactinemia. Clin Pharm 11(10):851–856
McGregor C, Riordan A, Thornton J (2017) Estrogens and the cognitive symptoms of schizophrenia: Possible neuroprotective mechanisms. Front Neuroendocrinol 47:19–33
Miller R (2009) Mechanisms of action of antipsychotic drugs of different classes, refractoriness to therapeutic effects of classical neuroleptics, and individual variation in sensitivity to their actions: part I. Curr Neuropharmacol 7(4):302–314
Montalvo I et al (2014) Increased prolactin levels are associated with impaired processing speed in subjects with early psychosis. PLoS One 9(2):e89428
Montalvo I et al (2018) Improvement in cognitive abilities following cabergoline treatment in patients with a prolactin-secreting pituitary adenoma. Int Clin Psychopharmacol 33(2):98–102
Moore L et al (2013) Serum testosterone levels are related to cognitive function in men with schizophrenia. Psychoneuroendocrinology 38(9):1717–1728
Mortimer AM (2007) Relationship between estrogen and schizophrenia. Expert Rev Neurother 7(1):45–55
Penadés R et al (2015) The search for new biomarkers for cognition in schizophrenia. Schizophr Res Cogn 2(4):172–178
Puljic K et al (2021) The association between prolactin concentration and aggression in female patients with schizophrenia. World J Biol Psychiatry 22(4):301–309
Rajkumar RP (2014) Prolactin and psychopathology in schizophrenia: a literature review and reappraisal. Schizophr Res Treat 2014:175360
Sheffield JM, Karcher NR, Barch DM (2018) Cognitive deficits in psychotic disorders: a lifespan perspective. Neuropsychol Rev 28(4):509–533
Shi C et al (2013) An ecologically valid performance-based social functioning assessment battery for schizophrenia. Psychiatry Res 210(3):787–793
Shi C et al (2015) The MATRICS Consensus Cognitive Battery (MCCB): co-norming and standardization in China. Schizophr Res 169(1–3):109–115
Shi C et al (2019) What is the optimal neuropsychological test battery for schizophrenia in China? Schizophr Res 208:317–323
Voráčková V et al (2021) Cognitive profiles of healthy siblings of first-episode schizophrenia patients. Early Interv Psychiatry 15(3):554–562
Vuk Pisk S et al (2019) Hyperprolactinemia—side effect or part of the illness. Psychiatr Danub 31(Suppl 2):148–152
Wasnik V et al (2019) Serum prolactin level and its correlation with psychopathology in drug free/drug naïve schizophrenia a case control study. Asian J Psychiatr 39:1–5
Yao S et al (2017) Cognitive function and serum hormone levels are associated with gray matter volume decline in female patients with prolactinomas. Front Neurol 8:742
Zhang XY et al (2002) Risperidone-induced increase in serum prolactin is correlated with positive symptom improvement in chronic schizophrenia. Psychiatry Res 109(3):297–302
Zhang X et al (2020) Glucose disturbances, cognitive deficits and white matter abnormalities in first-episode drug-naive schizophrenia. Mol Psychiatry 25(12):3220–3230
Zhu MH et al (2022) Amisulpride augmentation therapy improves cognitive performance and psychopathology in clozapine-resistant treatment-refractory schizophrenia: a 12-week randomized, double-blind, placebo-controlled trial. Mil Med Res 9(1):59
Acknowledgements
We would like to thank Yuying Qiu, Yongping Zhao, Shu Yang, Siying Kong, Ying Gao, Xiaoxiao Sun, Jiayue Wang, and Yeqing Dong from Tianjin Anding Hospital for their assistance in collecting the data.
Funding
This work was supported by the Tianjin Key Medical Discipline (Specialty) Construction Project (TJYXZDXK-033A), and the hospital-level project by Tianjin Anding Hospital (ADYKHT2021012). These funding sources had no other role in the study design, data collection, statistical analysis, drafting of the report, or submission of the paper for publication.
Author information
Authors and Affiliations
Contributions
GL and JL were responsible for the study design, statistical analysis, and manuscript preparation. FB, XQ, XZ, YJ, SW, ZX, CY, and ML were accountable for the data acquisition and editing of the manuscript. All the authors contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, G., Bai, F., Qu, X. et al. The relationship between serum prolactin levels and cognitive function in drug-naïve schizophrenia patients: a cross-sectional study. J Neural Transm 131, 385–391 (2024). https://doi.org/10.1007/s00702-024-02748-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-024-02748-4