Abstract
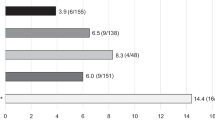
Kummell’s disease (KD) is a rare clinical complication of osteoporotic vertebral compression fractures (OVCFs). Minimally invasive surgery is an important way to treat KD. In this paper, we used Percutaneous Vertebroplasty (PVP) and Vesselplasty (VP) to treat KD. 125 patients with KD were admitted to our hospital. Among them, 89 patients received PVP and 36 received VP. All patients underwent operations successfully. VAS scores and ODI of both groups at each postoperative time point were lower than preoperatively. Postoperative Cobb angle of both groups postoperatively was lower than preoperatively (p < 0.05). The anterior height and ratio of vertebra compression of both groups postoperatively was lower than preoperatively (p < 0.05). Cement leakage occurred in 16 vertebrae (16/89) in PVP group and one (1/36) in VP group. Two patients suffered from transient paraplegia in PVP group immediately after operation. Adjacent vertebral fractures occurred in one patient in PVP group and one in VP group. Re-fracture of affected vertebra occurred in one patient in PVP group. Besides, four patients suffered from bone cement loosening in PVP group while one in VP group. Both PVP and VP play an important effect in pain relief and functional recovery for the treatment of KD. And VP is more effective than PVP in preventing cement leakage.
Summary
Percutaneous Vertebroplasty (PVP) and Vesselplasty (VP) were important procedures in treating Kümmell’s Disease (KD). As they have achieved good results in pain relief and functional recovery. Besides, they could reconstruct vertebral strength and prevent the aggravation of kyphosis in a long time. More importantly, VP is more effective than PVP in preventing cement leakage.



Similar content being viewed by others
References
Lim J, Choi SW, Youm JY, Kwon HJ, Kim SH, Koh HS (2018) Posttraumatic delayed vertebral collapse: Kummell’s Disease. J Korean Neurosurg Soc 61(1):1–9
Matzaroglou C, Georgiou CS, Assimakopoulos K, Giannakenas C, Karageorgos A, Saridis A, Kafchitsas K, Wilke HJ (2011) Kummell’s disease: pathophysiology, diagnosis, treatment and the role of nuclear medicine. Rationale according to our experience. Hell J Nucl Med 14(3):291–299
He D, Yu W, Chen Z, Li L, Zhu K, Fan S (2016) Pathogenesis of the intravertebral vacuum of Kummell’s disease. Exp Ther Med 12(2):879–882
Adamska O, Modzelewski K, Stolarczyk A, Kseniuk J (2021) Is Kummell’s Disease a Misdiagnosed and/or an Underreported Complication of Osteoporotic Vertebral Compression Fractures? A Pattern of the Condition and Available Treatment Modalities. J Clin Med 10(12)
Li Y, Qian Y, Shen G, Tang C, Zhong X, He S (2023) Percutaneous mesh-container-plasty versus percutaneous kyphoplasty for the treatment of Kummell’s disease: a retrospective cohort study. J Orthop Surg Res 18(1):260
Dai SQ, Qin RQ, Shi X, Yang HL (2021) Percutaneous vertebroplasty versus kyphoplasty for the treatment of neurologically intact osteoporotic Kummell’s disease. BMC Surg 21(1):65
Gao X, Du J, Zhang Y, Gong Y, Zhang B, Qu Z, Hao D, He B, Yan L (2022) Predictive Factors for Bone Cement Displacement following Percutaneous Vertebral Augmentation in Kummell’s Disease. J Clin Med 11(24)
He CJ, Liu GD (2018) Comparison of the efficacy and safety of bone-filling Mesh Container and simple percutaneous balloon kyphoplasty in the treatment of Osteoporotic Vertebral Compression fractures. Pain Physician 21(3):259–268
Khan M, Kushchayev SV (2019) Percutaneous vertebral body augmentations: the state of art. Neuroimaging Clin N Am 29(4):495–513
Zhang Y, Shi L, Tang P, Zhang L (2017) Comparison of the Efficacy between two micro-operative therapies of old patients with osteoporotic vertebral Compression fracture: a Network Meta-Analysis. J Cell Biochem 118(10):3205–3212
Chen C, Fan P, Xie X, Wang Y (2020) Risk factors for cement leakage and adjacent vertebral fractures in Kyphoplasty for osteoporotic vertebral fractures. Clin Spine Surg 33(6):E251–E255
Matzaroglou C, Georgiou CS, Panagopoulos A, Assimakopoulos K, Wilke HJ, Habermann B, Panos G, Kafchitsas K (2014) Kummell’s Disease: clarifying the mechanisms and patients’ inclusion Criteria. Open Orthop J 8:288–297
Wood KB, Li W, Lebl DR, Ploumis A (2014) Management of thoracolumbar spine fractures. Spine J 14(1):145–164
Kim YC, Kim YH, Ha KY (2014) Pathomechanism of intravertebral clefts in osteoporotic compression fractures of the spine. Spine J 14(4):659–666
Maldague BE, Noel HM, Malghem JJ (1978) The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology 129(1):23–29
Ishiyama M, Numaguchi Y, Makidono A, Kobayashi N, Fuwa S, Ohde S, Saida Y (2013) Contrast-enhanced MRI for detecting intravertebral cleft formation: relation to the time since onset of vertebral fracture. AJR Am J Roentgenol 201(1):W117–W123
Libicher M, Appelt A, Berger I, Baier M, Meeder PJ, Grafe I, Dafonseca K, Noldge G, Kasperk C (2007) The intravertebral vacuum phenomen as specific sign of osteonecrosis in vertebral compression fractures: results from a radiological and histological study. Eur Radiol 17(9):2248–2252
Theodorou DJ (2001) The intravertebral vacuum cleft sign. Radiology 221(3):787–788
Zhang B, Chen G, Yang X, Fan T, Chen Z (2022) Percutaneous Kyphoplasty Versus Percutaneous Vertebroplasty for Neurologically Intact Osteoporotic Kummell’s Disease: a systematic review and Meta-analysis. Global Spine J 12(2):308–322
Huang X, Chang H, Xu H, Chen X, Wang H, Song Y (2022) Comparison of outcomes between Percutaneous Vertebroplasty and Percutaneous Kyphoplasty for the Treatment of Kummell’s Disease: a Meta-analysis. Clin Spine Surg 35(6):276–286
Flors L, Lonjedo E, Leiva-Salinas C, Marti-Bonmati L, Martinez-Rodrigo JJ, Lopez-Perez E, Figueres G, Raoli I (2009) Vesselplasty: a new technical approach to treat symptomatic vertebral compression fractures. AJR Am J Roentgenol 193(1):218–226
Krauss M, Hirschfelder H, Tomandl B, Lichti G, Bar I (2006) Kyphosis reduction and the rate of cement leaks after vertebroplasty of intravertebral clefts. Eur Radiol 16(5):1015–1021
Huang Y, Peng M, He S, Tang X, Dai M, Tang C (2016) Clinical efficacy of Percutaneous Kyphoplasty at the hyperextension position for the treatment of osteoporotic Kummell Disease. Clin Spine Surg 29(4):161–166
Acknowledgements
Fang Zhou and Pu Jia designed the experiment protocol; Ruideng Wang and Youliang Hao collected and processed the data; Ruideng Wang analyzed the data and drafted this manuscript; Fang Zhou and Pu Jia reviewed the manuscript and provided important comments and revision. All authors approved the final manuscript.
Funding
This work was supported by National Natural Science Foundation of China (81971160).
Author information
Authors and Affiliations
Contributions
Fang Zhou and Pu Jia designed the experiment protocol; Ruideng Wang and Mengmeng Chen collected and processed the data; Ruideng Wang analyzed the data and drafted this manuscript; Fang Zhou and Pu Jia reviewed the manuscript and provided important comments and revision. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Ruideng Wang, Youliang Hao, Pu Jia and Fang Zhou declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, R., Hao, Y., Chen, M. et al. Comparison of the Clinical Outcomes of Vesselplasty vs. Percutaneous Vertebroplasty for the Treatment of Neurologically Intact Osteoporotic Kümmell’s Disease: A Retrospective Study. Calcif Tissue Int 114, 360–367 (2024). https://doi.org/10.1007/s00223-024-01186-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-024-01186-4